Respiratory Pathology Guide
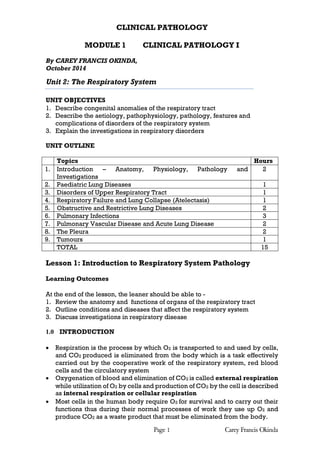
- 1. CLINICAL PATHOLOGY MODULE 1 CLINICAL PATHOLOGY I Page 1 Carey Francis Okinda By CAREY FRANCIS OKINDA, October 2014 Unit 2: The Respiratory System UNIT OBJECTIVES 1. Describe congenital anomalies of the respiratory tract 2. Describe the aetiology, pathophysiology, pathology, features and complications of disorders of the respiratory system 3. Explain the investigations in respiratory disorders UNIT OUTLINE Topics Hours 1. Introduction – Anatomy, Physiology, Pathology and Investigations 2 2. Paediatric Lung Diseases 1 3. Disorders of Upper Respiratory Tract 1 4. Respiratory Failure and Lung Collapse (Atelectasis) 1 5. Obstructive and Restrictive Lung Diseases 2 6. Pulmonary Infections 3 7. Pulmonary Vascular Disease and Acute Lung Disease 2 8. The Pleura 2 9. Tumours 1 TOTAL 15 Lesson 1: Introduction to Respiratory System Pathology Learning Outcomes At the end of the lesson, the leaner should be able to - 1. Review the anatomy and functions of organs of the respiratory tract 2. Outline conditions and diseases that affect the respiratory system 3. Discuss investigations in respiratory disease 1.0 INTRODUCTION Respiration is the process by which O2 is transported to and used by cells, and CO2 produced is eliminated from the body which is a task effectively carried out by the cooperative work of the respiratory system, red blood cells and the circulatory system Oxygenation of blood and elimination of CO2 is called external respiration while utilization of O2 by cells and production of CO2 by the cell is described as internal respiration or cellular respiration Most cells in the human body require O2 for survival and to carry out their functions thus during their normal processes of work they use up O2 and produce CO2 as a waste product that must be eliminated from the body.
- 2. The normal intake of air is 7 litres/min of which 5 litres is available for Page 2 Carey Francis Okinda alveolar ventilation. Factors that maintain adequate respiration include adequate intake of air, rapid diffusion along the alveolar ducts and through alveolar walls and adequate perfusion In chronic lung disease, ventilation, diffusion and perfusion disorders are present in varying degrees Under normal circumstances, the upper area of the lung is better ventilated than perfused while the base is better perfused than ventilated an imbalance magnified in lung disease. 2.0 DIVISIONS AND ORGANIZATION Divided into upper and lower tracts or divisions with organs of the upper respiratory tract are located outside the thorax or chest cavity whereas those in the lower division are located almost entirely within the chest The upper respiratory tract comprises of nose, pharynx, nasopharynx, oropharynx, laryngopharynx, larynx and trachea while the lower respiratory tract has the bronchial tree and lungs (these are the passages) Comprises of lungs and respiratory passages (airways), which work in intimate collaboration with the thoracic cage, respiratory muscles and the pulmonary circulation. It uses highly effective convective systems of ventilation and circulation for long distance transport of O2 and CO2 and uses diffusion exclusively for short distance movements of O2 and CO2 The main components of the respiratory system are: - the air pump, mechanism for oxygen and carbon dioxide carrying, gas exchange surface, circulatory system and regulatory mechanisms. 3.0 PHYSIOLOGY RESPIRATORY SYSTEM Respiratory physiology is a complex series of interacting and coordinated processes that ensure adequate and prompt supply of oxygen and removal of carbon dioxide in an effort to maintain the stability and consistency of the internal environment It involves physiological control mechanisms such as acid-base, water and electrolyte balance, circulation and metabolism. Lungs are structures where gas exchange between blood and inspired air takes place whereas the respiratory passages are structures along which air is conveyed to and from the lungs Functions 1. Provide oxygen to the blood stream and remove carbon dioxide 2. Enables sound production or vocalization as expired air passes over the vocal cords 3. Assists in abdominal compression during micturition, defecation and parturition (childbirth) 4. Lung Defence mechanism - protective and reflexive non-breathing air movements e.g. coughing and sneezing to keep the air passageways clean. 5. Temperature regulation – loss of heat during expiration 6. Maintenance of water balance - small amounts of water are lost during expiration
- 3. 7. Regulation of acid-base balance 8. Anticoagulant function – lungs contain mast cells which secret heparin which Page 3 Carey Francis Okinda prevents intravascular clotting 9. Metabolic functions – manufacture surfactant for local use, fibrinolytic system 10. Endocrine functions a. Pulmonary capillary endothelial cells secrete angiotensin converting enzyme (ACE) which activates angiotensin I into angiotensin II b. Lung tissues synthesize prostaglandins, acetylcholine, bradykinin and serotonin 4.0 INTRODUCTION TO PATHOLOGY OF THE RESPIRATORY SYSTEM The prime role of the respiratory system is oxygenation of blood and removal of carbon dioxide CO2 The function requires that air comes into close approximation with blood through the anatomical arrangement of the alveoli and blood vessels. 1) Constant inward and outward flow of the enormous air exposes the respiratory system to infection by both microbes present in inspired air and by downward spread of bacteria that colonize the nose and throat 2) Inhalation of pollutants such as dust, fumes, smokes increase the incidence of bronchitis, chronic lung disease and bronchial carcinoma 3) Vascular architecture of the lungs allows passage of blood into the lungs during each cycle makes the lungs to be vulnerable to effects of cardiovascular diseases. This is due to disturbance of pulmonary haemodynamics e.g. pulmonary oedema and on the other hand, lung diseases interfere with the pulmonary blood flow with noticeable effects on the heart and systemic circulation because cardiac and pulmonary functions are closely interdependent. 4) The lung is a frequent victim of malfunction elsewhere for example failure of the left side of the heart results in pulmonary congestion and oedema, systemic thrombosis on many occasions causes pulmonary embolism and the lungs are a common site for secondary tumours. Main diseases of the airways and the lungs are caused by infection and inflammation Environmental factors such as smoking and occupational exposure to dust contributing to the morbidity and mortality resulting from respiratory problems Tumours of the bronchial tree and lung are common and important, as almost all of them are malignant. The key effect of respiratory problems is poor oxygenation resulting in respiratory failure.
- 4. Page 4 Carey Francis Okinda 5.0 INVESTIGATIONS 1) Chest X-ray Use the ABCDEFGH mnemonic Chest X-ray - Systematic Approach Reading a chest X-ray (CXR) requires a systematic approach. The "right film for the right patient" Check that the film bears the patient's name, age or hospital number too The label may also tell features such as anteroposterior (AP) projection or supine position Check the date of the film to ascertain which one you are viewing Technical details Check the position of the side marker (left or right) against features such as the apex of the heart and air bubble in the stomach. A misplaced marker is more common than dextrocardia or situs inversus. Most films are a poster anterior (PA) projection. The usual indication for AP is a patient who is confined to bed. AP vs PA Views o Look at the relationship of the scapulae to the lung margins o A PA view shows the scapulae clear of the lungs whilst in AP projection they always overlap o Vertebral endplates are more clearly visible in AP and laminae in PA. This is important because the heart looks bigger on an AP view. Lateral films o A lateral view may have been requested or performed on the initiative of the radiographer or radiologist. As an X-ray is a two-dimensional
- 5. shadow, a lateral film helps to identify a lesion in 3 dimensions. The usual indication is to confirm a lesion seen on a PA film. o The heart lies in the anteroinferior field. Look at the area anterior and superior to the heart; this should be black because it contains aerated lung. Similarly, the area posterior to the heart should be black right down to the hemidiaphragms. The degree of blackness in these two areas should be similar, so compare one with the other. If the area anterior and superior to the heart is opacified, it suggests disease in the anterior mediastinum or upper lobes. If the area posterior to the heart is opacified there is probably collapse or consolidation in the lower lobes. The normal posture for films is erect (supine is usually for patients confined to bed). In an erect film, the gastric air bubble is clearly in the fundus with a clear fluid level but, if supine, in the antrum. In a supine film, blood will flow more to the apices of the lungs than when erect. Rotation should be minimal. This can be assessed by comparing the medial ends of the clavicles to the margins of the vertebral body at the same level. Oblique chest films are requested to look for achalasia of the cardia or fractured ribs. CXR should be taken with the patient in full inspiration but some people have difficulty holding full inspiration (except when seeking a small pneumothorax as this will show best on full expiration) A CXR in full inspiration should have the diaphragm at the level of the 6th rib anteriorly and the liver pushes it up a little higher in the right than on the left. Page 5 Carey Francis Okinda Penetration o Is affected by both the duration of exposure and the power of the beam o More kV gives a more penetrating beam o A poorly penetrated film looks diffusely light (an x-ray is a negative) and soft tissue structures are readily obscured, especially those behind the heart o An over-penetrated film looks diffusely dark and features such as lung markings are poorly seen. Airway Trace the lucency from the neck down towards the carina Should be midline and you should be able to see two bronchi splitting from it Bones and soft tissues Look at the shoulder joint and trace out each rib contour to check for fractures or other abnormalities such as lytic lesions Are both breast shadows present Attention may be merited to apices, periphery of the lungs, under and behind the hemidiaphragms and behind the heart Cardiac Check the cardio-thoracic ratio (CTR) o The width of the heart should be no more than half the width of the chest o About a third of the heart should be to the right and two thirds to the left of centre o Note: the heart looks larger on an AP film and thus you cannot comment on the presence or absence of cardiomegaly on an AP film.
- 6. Diaphragm (e.g. flat or elevated hemidiaphragm) Ascertain that the surface of the hemidiaphragms curves downwards, and that the costophrenic and cardiophrenic angles are not blunted Blunting suggests an effusion Extensive effusion or collapse causes an upward curve Check for free air under the hemidiaphragm - this occurs with perforation of the bowel but also after laparotomy or laparoscopy Edges (borders) of the heart The left border of the heart consists of the left atrium above the left ventricle The right border is only the right atrium alone and above it is the border of the superior vena cava. The right ventricle is anterior and so does not have a border on the PA chest X ray film. It may be visible on a lateral view. To rule out lingular and left middle lobe pneumonia or infiltrates Fields (The Lungs) The pulmonary arteries and veins are lighter and air is black, as it is Page 6 Carey Francis Okinda radiolucent. Check both lungs, starting at the apices and working down, comparing left with right at the same level The lungs extend behind the heart, so try to look there too Note the periphery of the lungs - there should be few lung markings here Disease of the air spaces or interstitium increases opacity Look for a pneumothorax which shows as a sharp line of the edge of the lung Gastric Bubble Check for a lucency in the left upper abdominal quadrant Hilum Look at the mediastinal contours, first to the left and then to the right. The trachea should be central. The aortic arch is the first structure on the left, followed by the left pulmonary artery. The branches of the pulmonary artery fan out through the lung. Instrumentation Look for obvious unusual opacities such a chest drain, a pacemaker or a foreign body. This is a two-dimensional picture and so a central opacity may not be something that was swallowed and is now impacted in the oesophagus. It might be a metal clip from a bra strap or a hair band on a plait.
- 7. Page 7 Carey Francis Okinda Interpretation Abnormal opacities When observing an abnormal opacity, note: Size and shape Number and location Clarity of structures and their margins Homogeneity The common patterns of opacity are: o Collapse o Consolidation o Heart and mediastinum Collapse and consolidation Collapse, also called atelectasis, and consolidation are caused by the presence of fluid instead of air in areas of the lung. An air bronchogram is where the airway is highlighted against denser consolidation and vascular patterns become obscured. Confluent opacification of the hemithorax may be caused by consolidation, pleural effusion, complete lobar collapse and after a pneumonectomy. To find consolidation, look for absence or blurring of the border of the heart or Hemidiaphragm. The lung volume of the affected segment is usually unaffected. Collapse of a lobe (atelectasis) may be difficult to see. Look for a shift of the fissures, crowding of vessels and airways, and possible shadowing caused by a proximal obstruction like a foreign body or carcinoma. A small pleural effusion will cause blunting of the costophrenic or cardiophrenic angles. A larger one will produce an angle that is concave upwards. A very large one will displace the heart and mediastinum away from it, whilst collapse draws those structures towards it. Collapse may also raise the hemidiaphragm
- 8. Heart and mediastinum The heart and mediastinum are deviated away from a pleural effusion or a pneumothorax, especially if it is a tension pneumothorax and towards collapse. If the heart is enlarged, look for signs of heart failure with an unusually marked vascular pattern in the upper lobes, wide pulmonary veins and possible Kerley B lines. These are tiny horizontal lines from the pleural edge and are typical of fluid overload with fluid collecting in the interstitial space. If the hilum is enlarged, look for structures at the hilum such as pulmonary artery, main bronchus and enlarged lymph nodes. Page 8 Carey Francis Okinda Chest X-ray in children Identification of the patient are still important A child, especially if small, is more likely to be unable to comply with instructions such as keeping still, not rotating and holding deep inspiration
- 9. Technical considerations such as rotation and under or over penetration of the film still merit attention and they are more likely to be unsatisfactory A child is more likely to be laid down and have an AP film with the radiographer trying to catch the picture at full inspiration Page 9 Carey Francis Okinda Assess lung volume Count down the anterior rib ends to the one that meets the middle of the hemidiaphragm A good inspiratory film should have the anterior end of the 5th or 6th rib meeting the middle of the diaphragm More than six anterior ribs shows hyperinflation Fewer than five indicates an expiratory film or underinflation. Tachypnoea in infants causes trapping of air Expiration compresses the airways, increasing resistance and, especially less than 18 months, air enters more easily than it leaves and is trapped, causing hyperinflation. Bronchiolitis, heart failure and fluid overload are all causes With underinflation, the 3rd or 4th anterior rib crosses the diaphragm. This makes normal lungs appear opaque and a normal heart appears enlarged. Positioning Sick children, especially if small, may not be cooperative with being positioned Check if the anterior ends of the ribs are equal distances from the spine Rotation to the right makes the heart appear central, and rotation to the left makes the heart look large and can make the right heart border disappear. Lung density Divide the lungs into upper, middle, and lower zones and compare the two sides Infection can cause consolidation, as in an adult Collapse implies loss of volume and has various causes The lung is dense because the air has been lost In children, the cause is usually in the airway, such as an intraluminal foreign body or a mucous plug Complete obstruction of the airway results in reabsorption of air in the affected lobe or segment Collapse can also be due to extrinsic compression such as a mediastinal mass or a pneumothorax. Differentiating between collapse and consolidation can be difficult or impossible, as both are denser. Collapse may pull across the mediastinum and deviate the trachea. This is important, as pneumonia is treated with consolidation antibiotics but collapse may require bronchoscopy to find and remove an obstruction. Pleural effusion In children, unilateral effusion usually indicates infection whilst bilateral effusion occurs with hypoalbuminaemia as in nephrotic syndrome. Bronchial wall thickening is a common finding on children's X-rays Look for "tram track" parallel lines around the hilar
- 10. The usual causes are viral infection or asthma but this is a common finding Page 10 Carey Francis Okinda with cystic fibrosis. Heart and mediastinum The anterior mediastinum, in front of the heart, contains the thymus gland It appears largest at about 2 years old but it continues to grow into adolescence. It grows less fast than the rest of the body and so becomes relatively smaller The right lobe of the lung can rest on the horizontal fissure, which is often called the sail sign. Assessment of the heart includes assessment of size, shape, position and pulmonary circulation The cardiothoracic ratio is usually about 50% but can be more in the first year of life and a large thymus can make assessment difficult, as will a film in poor inspiration. As with adults, one third should be to the left of centre and two thirds to the right. Assessment of pulmonary circulation can be important in congenital heart disease but can be very difficult in practice. 2) Bronchoscopy 3) Blood Gas analysis This is analysis of the oxygen and carbon dioxide levels in the blood 4) Total Blood count Shows the various red blood cell indices, white blood cells (total and differential count) and the platelets 5) Sputum Examination Refer to earlier class discussions
- 11. Page 11 Carey Francis Okinda 6) Blood cultures Done to determine the microbes present and their sensitivity to various drug agents (details in microbiology) 7) Peak Expiratory Flow The purpose is to measure lung function The patient inhales deeply and exhales hard into a plastic tube in order to get a reading for how fast the patient is able to exhale successfully The result of this test is a peak flow number. 8) Spirometry Is a non-invasive method of lung function testing, which measures the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled A spirometer is a device used Indications i) To determine how well the lungs receive, hold, and utilize air ii) To monitor a lung disease iii) To monitor the effectiveness of treatment iv) To determine the severity of a lung disease
- 12. v) To determine whether the lung disease is restrictive (decreased airflow) or obstructive (disruption of airflow) After taking a deep breath, a person forcefully breathes out into the spirometer as completely and forcefully as possible. The spirometer measures both the amount of air expelled and how quickly the air was expelled from the lungs. The measurements are recorded by the spirometer The normal, healthy values measured by the spirometer for the amount of air exhaled vary from person to person. The results are compared to the average expected in someone of the same age, height, sex, and race, Values below 80 percent of the average, it may be a sign of lung disease or Page 12 Carey Francis Okinda other airflow obstruction. 9) ECG 10) Ultrasound 11) CT Scan 12) MRI 13) Biopsy What are the indications of a biopsy?
- 13. Lesson 2: Paediatric Lung Disease Page 13 Carey Francis Okinda Learning Outcomes At the end of the lesson, the leaner should be able to - 1. Discuss the developmental anomalies of the respiratory system 2. Describe the causes and effects of acute respiratory distress syndrome (hyaline membrane disease) Developmental Abnormalities Developmental defects of the lungs include agenesis or hypoplasia of both lungs, one lung or single lobe; tracheal and bronchial anomalies – atresia, stenosis and tracheobronchial fistula; vascular anomalies; congenital lobar over-inflation (emphysema), bronchogenic cysts; congenital airway malformation and pulmonary sequestrations 1.0 PULMONARY HYPOPLASIA Incomplete development of both lungs resulting in reduced weight, volume and acini compared to body weight and gestational age Lung smaller than normal Incidence 10% associated with other congenital abnormalities and lung compression by abnormal masses and oligohydromnious Usually secondary to space occupying lesion in the uterus, oligohydromnious or impaired foetal respiratory movements as seen in congenital diaphragmatic hernia, renal cystic kidney, renal agenesis and anencephaly. 2.0 BRONCHIAL ATRESIA Results in severe narrowing of the bronchus 3.0 BRONCHOGENIC SEQUESTRATION Cysts attached to the trachea Represent accessory bronchial buds 4.0 BRONCHOPULMONARY SEQUESTRATION Patients develop abnormal lung mass without any normal connection to the airway or bronchial system There are two types of sequestration – extralobular and intralobular. Extralobular sequestrations – external to the lungs and found elsewhere in the thorax and mediastinum. Intralobular sequestrations – found in the lung tissue and usually associated with recurrent localized infections or bronchiectasis Summary of Paediatric lung disease -bronchial atresia -pulmonary hypoplasia -bronchogenic sequestration -bronchopulmonary sequestration -neonatal RDS /HMD
- 14. 5.0 Neonatal Respiratory Distress Syndrome (Hyaline Caesarean Section Maternal Diabetes Amniotic Fluid aspiration IMMATURE/DAMAGED TYPE II PNEUMOCYTES FIBRIN/HYALINE Membrane Endothelial Damage Alveolar Lining damage Hypoxia Pulmonary Vasoconstriction Page 14 Carey Francis Okinda Membrane Disease) Introduction Occurs due to deficiency of surfactant and primarily disease of premature infants Seen in infants of diabetic mothers (excess insulin production by the foetus suppresses surfactant production) Neonates born at the gestation 32 – 36 weeks have 20% mortality while those at < 28 weeks have 60% mortality The risk factors include prematurity, diabetic mother, neonatal aspiration and multiple births. Pathogenesis Immature or damaged lung is unable to make enough surfactant (a lecithin-rich surface-active lipid) that reduces surface tension in the alveoli and keeps the alveoli open Diagram 2.1: Pathogenesis of ARDS RISK FACTORS Prematurity (< 36 weeks) Low Level surfactant Lung Collapse Multiple Pregnancy ARDS results from widespread acute injury to the alveolar capillary membrane, which produces high permeability oedema and inhibits surfactant function (especially fibrin monomers) Epithelial injury also impairs new surfactant synthesis and inflammation may exacerbate the injury because of release of oxidants and lysosomal enzymes from activated leukocytes Lack of surfactant results in lung collapse with microatelectasis. Hypoxia causes damage to the alveolar lining cells and pulmonary arterial constriction resulting in endothelial damage hence plasma leaks into the alveoli where it is deposited as fibrin (bright pink-stained membrane) and thus the name hyaline membrane disease. Fibrin reduces gas exchange further worsening the hypoxic state.
- 15. Lung compliance is decreased because many airspaces contain oedema (and hence cannot accept air) and because abnormally high surface tension counteracts the negative intrapleural pressure. What are the differential Page 15 Carey Francis Okinda Pathology The lungs: - 1. Have fibrous obliteration of bronchioles 2. Peribronchial fibrosis 3. Overdistended alveolar Clinical Features Dyspnoea Tachypnoea (faster than 60 breaths a minute Makes a grunting sound when he breathes out Has respiratory distress (what are the features) Cyanosis Crepitations Diagnosis 1) Blood culture - check for infection 2) Blood gas analysis - check amount of oxygen in blood 3) Chest X-ray Differential Diagnosis diagnoses? Complications 1. Intracerebral bleed ( hypoxia related) 2. PDA (failure to close as normal closure is stimulated by oxygenation) 3. Necrotizing enterocolitis ( ischaemic/hypoxic damage of the gut) 4. Bronchopulmonary dysplasia (high pressure ventilation and oxygen toxicity to alveolar lining cells) RISK FACTORS OF ARDS -premature (<36wks gestation) -infants to diabetic mothers -cs -amniotic fluid aspiration -multiple pg - COMPLICATIONS -intracerebral bleed -PDA -necrotizing enterocolitis -bronchopulmonary dysplasia
- 16. Lesson 3: Upper Respiratory Tract Disorders Page 16 Carey Francis Okinda Learning Outcomes At the end of the lesson, the leaner should be able to - 1. Discuss the pathology of conditions affecting organs of the upper respiratory tract A. EPISTAXIS disorder Epistaxis is common affecting 60% of the population of which only 6% seek medical advice. The bleeding may be spontaneous or profuse and life threatening. Bleeding may originate from anywhere within the nose, but frequently from the Little’s area. The peak incidence is in children, young adults and above the age of 55 years. Causes 1. Nasal a. Idiopathic (85%) b. Trauma – nose pricking, fractures c. Inflammation – rhinitis, sinusitis d. Iatrogenic – nasal sprays, surgery e. Hereditary – Hereditary haemorrhagic telangiectasis f. Neoplasms – carcinoma, juvenile angiofibroma 2. Systemic a. Anticoagulants – warfarin, NSAIDS b. Hypertension c. Blood dyscrasias – leukaemia d. Hereditary coagulopathies – haemophilia B. ACUTE INFLAMMATIONS Infections of the nose, nasal sinuses, pharynx and larynx are common and usually self-limiting illnesses often because of viral infection, which on many occasions, is followed by bacterial super infection. Viral Infections Viral infections have characteristic features of acute inflammation such as redness; oedema, nasal stuffiness, swelling of the nasal mucosa, duct obstruction and abundant clear nasal discharge (mucous secretion) without exudation of neutrophils. Aetiology 1. Rhinovirus 2. Corona virus 3. Myxovirus e.g. Influenza 4. Paramyxovirus e.g. respiratory syncytial virus
- 17. Page 17 Carey Francis Okinda Bacterial Phase After the viral invasion, commensal bacteria present in the respiratory system e.g. Streptococcus mutans and Haemophilus influenza can superinfect the damaged tissue. This stage exhibits features of acute inflammation and exudation of neutrophils with a mucopurulent discharge. Pathogenesis Viruses adhere to the cell surface proteins e.g. the cilia and enter the host cells and replicate during which period the cells become damaged and readily invaded by commmensal bacteria 1. Common Cold (Acute Coryza) This is the commonest illustration of acute inflammations of the upper respiratory tract. It involves the nose and adjacent structures such as the nasal sinuses (maxillary, sphenoidal and frontal) where there occurs blocking of their drainage by the swollen mucosa resulting in sinusitis. Acute coryza is spread by droplet via sneezing. 2. Rhinitis Rhinitis is inflammation of the mucous membranes of the nose. Acute Rhinitis The commonest causes of acute rhinitis are common cold (acute coryza) and hay fever. Allergic Rhinitis “Hay Fever” Hay fever is an acute allergic or atopic rhinitis that occurs as a result of hypersensitivity (type I) to pollen, house dust, animal dandruffs and other antigens. Patients develop immediate symptoms of sneezing, itching and water rhinorrhoea. Chronic Rhinitis Chronic rhinitis follows an acute inflammatory episode that fails to resolve. Because of acute inflammation, there is inadequate draining of the nasal sinuses due to nasal obstruction, polyps or enlargement of the adenoids leading to chronic sinusitis and chronic nasopharyngitis. 3. Acute Sinusitis Acute sinusitis occurs often as a complication of acute infection of the nose with the responsible organs such as Strep. pyogenes, Strep. pneumoniae and Staph. aureas.
- 18. Page 18 Carey Francis Okinda C. THE PHARYNX 1. Acute Nasopharyngitis Acute nasopharyngitis usually accompany acute rhinitis or acute tonsillitis. The common organism implicated is Staphylococcus aureas. The histopathology includes - Hyperaemia Oedema Hyperactive mucosal glands Increased mucosal secretions Neutrophil polymorphs – usually sparse in viral infections but increase with secondary bacterial infections Superficial destruction of ciliated epithelium Swollen/enlarged/distended mucosal glands 2. Nasal Polyps Nasal polyps usually form on the middle turbinate bones and within the maxillary sinuses because of chronic recurrent inflammation of the nasal mucosa particularly of allergic aetiology that result in polypoid thickening of the mucosa. Polyps are rounded or elongated masses that are usually bilateral with gelatinous consistency and smooth and shiny surface. Diagram 3.1: Nasal Polyps D. THE LARYNX AND TRACHEA 1. Acute Laryngitis and Tracheaitis Acute laryngitis and tracheaitis are common occurrences Aetiology 1. Viral - Adeno virus;Epstein Barr virus (EBV) 2. Bacteria - Strep. Pneumonia, Strep. Pyogenes, Neisseria catarrhalis, Heamophilus influenzae and Corynebacterium diptheriae
- 19. Complicates acute febrile states such as measles, influenza and typhoid and may spread to cause bronchitis resulting in laryngo-tracheo-bronchitis (LTB). In situations where there is secondary infection with Strep. pyogenes, Strep. pneumoniae and Staph. aureas leads to pseudomembranous inflammation. Tonsillitis is common because of streptococcal infection while Heamophilus influenza type B usually causes acute epiglottitis, which is a childhood illness. Page 19 Carey Francis Okinda Chronic Laryngitis Frequently associated with excessive, smoking, repeated attacks of infection and atmospheric pollution. TB Laryngitis Is usually secondary to pulmonary tuberculosis when the tubercle bacilli are carried directly in the sputum to the larynx affecting the larynx and to a less extend to the trachea. It causes thickening, caseation and ulceration of the pharynx. The lesion is very painful and inflammatory swelling and oedema of the glottis may supervene. E. UPPER AIRWAY OBSTRUCTION Upper airway obstruction is one of the most serious emergencies faced by clinicians Early diagnosis followed by restoration of airflow is essential to prevent cardiac arrest or irreversible brain damage that occurs within minutes of complete airway obstruction May be functional or anatomic and may develop acutely or subacutely Occurs at any level of the upper respiratory tract but laryngeal obstruction has a particular importance because the larynx is the narrowest portion of the upper airway. Causes 1) Traumatic causes Laryngeal stenosis; airway burn; acute laryngeal injury; facial trauma (mandibular or maxillary fractures); haemorrhage 2) Infections - suppurative parotitis; retropharyngeal abscess; tonsillar hypertrophy; Ludwig’s angina; epiglottitis; laryngitis.; Laryngotracheobronchitis (croup); Diphtheria 3) Iatrogenic causes a) Tracheal stenosis post-tracheostomy b) Tracheal stenosis post-intubation c) Mucous ball from transtracheal catheter 4) Foreign bodies 5) Vocal cord paralysis 6) Tumours a) Laryngeal tumours (benign or malignant) b) Laryngeal papillomatosis c) Tracheal stenosis (caused by intrinsic or extrinsic tumours) 7) Angioedema
- 20. a) Anaphylactic reactions b) Angiotensin-converting enzyme inhibitors Page 20 Carey Francis Okinda Clinical Features Marked respiratory distress; altered voice; dysphagia; odynophagia; the hand-to-the-throat choking sign; stridor; facial swelling; prominence of neck veins; absence of air entry into the chest; tachycardia In an unconscious or sedated patient, the first sign of airway obstruction may be inability to ventilate with a bag-valve mask after an attempt to open the airway with a jaw-thrust maneuver Asphyxiation progresses; cyanosis; bradycardia; hypotension; irreversible cardiovascular collapse Investigations 1) Plain Chest and Neck Radiographs 2) Computed Tomography 3) Spirometry 4) Bronchoscopy F. TUMOURS Benign tumours 1. Polyps 2. Squamous papilloma 3. Lipomas 4. Angiomas Malignant Tumours 1. Squamous cell carcinoma e.g. ca larynx. Laryngitis Laryngitis is inflammatory process/condition of the larynx due to various causes. Types 1. Simple laryngitis/acute laryngitis 2. Chronic laryngitis 3. Diphtheric laryngitis 4. Tuberculous laryngitis 5. Syphilitic laryngitis Group Work – LTB 1. What are the causes? 2. Definition and predisposing factors 3. What is the pathophysiology and the pathology? 4. What are the features? 5. Diagnosis and differential diagnosis 6. What are the complications? 7. Management
- 21. Lesson 4: Respiratory Failure & Atelectasis (Lung Collapse) Task: Using examples explain how the above factors cause respiratory failure. Page 21 Carey Francis Okinda Learning Outcomes At the end of the lesson, the learner should be able to - 1. Describe the causes of lung collapse 2. Discuss the effects and features of lung collapse 3. Describe causes and effects of lung collapse 4. Discuss the pathophysiology and complications of lung collapse 5. Investigate a patient with lung collapse Respiratory Failure 1.0 INTRODUCTION Normal respiratory function maintains blood gases within physiological limits where the normal PaO2 is 10.7 kPa – 13.3 kPa (80 – 100 mmHg) and PaCO2 is 4.7kPa – 6.0 kPa (35 – 45 mmHg) Respiratory failure is defined as when PaO2 falls below 8 kPa (60 mmHg). Respiratory failure is a syndrome of inadequate gas exchange due to dysfunction of one or more essential components of the respiratory system namely chest wall, airways, alveolar–c capillary units, pulmonary circulation, nerves and CNS/brain Stem 2.0 MECHANISMS OF ARTERIAL HYPOXAEMIA a) Low inspired partial pressure of O2 as a result of ambient air at high altitude and reduced oxygen tension in inspired air b) Mismatch of alveolar ventilation to perfusion c) Alveolar hypoventilation d) Increased shunt fraction of blood passing from the right heart to systemic arterial circulation in right to left cardiac shunts without being oxygenated e) Disease of the alveolar capillary membrane locking exchange of gases 3.0 PREDISPOSING FACTORS 1. Infection in the tracheobronchial tree, pneumonia, fever 2. Change in tracheobronchial secretions (increased volume and viscosity) 3. Bronchospasms
- 22. 4. Disturbance in ability to clear secretions 5. Drugs – sedatives, narcotics, anaesthetics 6. Oxygen therapy 7. Trauma 8. Cardiovascular disorders 9. Pneumothorax Page 22 Carey Francis Okinda 4.0 CAUSES 1. Extrinsic Lung Disorders a. Respiratory centre depression e.g. Drug overdose (sedatives, narcotics); cerebral trauma or infarction; bulbar poliomyelitis and encephalitis b. Neuromuscular disorders - cervical cord injury; Guillain-Barre Syndrome; myasthenia gravis and muscular dystrophy c. Pleural and chest wall disorders e.g. chest injury (flail chest, rib fracture); pneumothorax; pleural effusion; kyphoscoliosis (abnormal lung) and obesity – Pickwickian syndrome 2. Intrinsic Lung Disorders a. Diffuse obstructive disorders e.g. emphysema and chronic bronchitis (COPD); asthma and status asthmaticus and cystic fibrosis b. Diffuse restrictive disorders e.g. Interstitial fibrosis e.g. silica and coal; pulmonary oedema (cardiogenic, non-cardiogenic e.g. ARDS); atelectasis ; consolidated pneumonia c. pulmonary vascular disorders e.g. pulmonary emboli and severe emphysema 5.0 CLASSIFICATION 1. Type I – Failure of oxygen exchange (PaO2 <60) 2. Type II – Failure to exchange or remove carbon dioxide (PaCO2 >45) 1. Type III – Post operative respiratory failure (both oxygen and ventilatory failure) 2. Type IV – Shock 5.1. Type I Respiratory Failure Is a state of hypoxaemia without CO2 retention (blood carbon dioxide remains within the normal limits) Failure of oxygen exchange Pathophysiologic mechanisms of arterial hypoxaemia include 1) Decreased partial pressure of O2 in alveoli a) Hypoventilation b) Decreased partial pressure of O2 in the inspired air c) Underventilated alveoli (areas of low ventilationperfusion) 2) Intrapulmonary shunt (areas of zero ventilation-perfusion) 3) Decreased mixed venous O2 content (low-haemoglobin saturation) a) Increased metabolic rate b) Decreased cardiac output c) Decreased arterial O2 content
- 23. Page 23 Carey Francis Okinda Causes 1. Adult respiratory distress syndrome (ARDS) 2. Asthma 3. Pulmonary oedema 4. Chronic obstructive pulmonary disease (COPD) 5. Interstitial fibrosis 6. Pneumonia 7. Pneumothorax 8. Atelectasis Diagnosis 1. Arterial blood gases analysis – reduced PaCO2 2. Respiratory function tests – reduced FEVR and FEV1 5.2. Type II Respiratory Failure Failure to exchange or remove carbon dioxide A state of decreased PaO2 and increased PaCO2 (> 6.7 kPa/50 mmHg) Results from alveolar hypoventilation and is commonly from chronic bronchitis and emphysema Causes 1) Disorders affecting central ventilatory drive a) Brain stem infarction or haemorrhage b) Brain stem compression from supratentorial mass c) Drug overdose, narcotics, benzodiazepines, anaesthetic agents etc. 2) Disorders affecting signal transmission to the respiratory muscles a) Myasthenia Gravis b) Gullain-Barrè syndrome c) Spinal –Cord injury and Head injury d) Multiple sclerosis e) Residual paralysis (Muscle relaxants) 3) Disorders of respiratory muscles or chest-wall a) Muscular dystrophy b) Polymyositis c) Flail Chest d) Thoracic wall deformities Mechanism Reduced alveolar ventilation results in reduced ventilator effort and there is inability of the alveolar to overcome increased resistance to ventilation. 5.3. Type III Respiratory Failure Perioperative respiratory failure Increased atelectasis due to low functional residual capacity (FRC) in the setting of abnormal abdominal wall mechanics
- 24. Often results in type I or type II respiratory failure and can be enhanced by anaesthetic or operative technique, posture, incentive spirometry, post-operative analgesia, attempts to lower intra- abdominal pressure Causes 1. Inadequate post- operative analgesia, upper abdominal incision 2. Obesity, ascites 3. Pre- operative tobacco smoking 4. Excessive airway secretions 5. Adult ARDS 6. Asthma 7. Chronic obstructive pulmonary disease 5.4. Type IV Respiratory Failure Describes patients who are intubated and ventilated in the process of Page 24 Carey Francis Okinda resuscitation for shock Goal of ventilation is to stabilize gas exchange and to unload Causes 1. Cardiogenic shock 2. Septic shock 3. Hypovolemic shock 6.0 EFFECTS ON CVS Chronic respiratory failure has major effects in the cardiovascular system including pulmonary hypertension and polycythaemia. Pulmonary Hypertension Pulmonary vasoconstriction results in increased pulmonary artery pressure and increased work of the ventricles The effects are felt in pulmonary arteries resulting in intimal proliferation and occlusion of the lamina. Polycythaemia Hypoxia stimulates release of erythropoietin by the kidney, which is the cause of increased viscosity of blood and the risk of thrombosis. 7.0 FEATURES OF RESPIRATORY FAILURE Tachycardia, tachypnoea, sweating, inability to speak Use of accessory muscles of respiration Pulsus paradoxical and paradoxical respiration (abdominal and thoracic components move in opposite directions), asynchronous respiration (discrepancy in the rate of movement of the abdominal and thoracic components), respiratory alternans 8.0 INVESTIGATIONS 1) Chest x-ray 2) ECG 3) Echocardiogram
- 25. Page 25 Carey Francis Okinda 4) Pulmonary function tests 5) Bronchoscopy 6) Blood gas analysis Collapse of Lung Tissue – Atelectasis 1.0 INTRODUCTION Lung collapse comprises of atelectasis and acquired collapse ‘Atelectasis’ is a Greek word for imperfect expansion Atelectasis refers to incomplete expansion of the lungs (neonatal atelectasis) or the collapse of a previously inflated lung (acquired atelectasis) encountered in adults. Atelectasis has important clinical consequences of disturbing the respiratory function namely: - 1) Obstruction of an airway results in resorption of air from the lung distal to the obstruction 2) Compression of the lung as seen when fluid or air accumulates in the pleural cavity 3) Scarring of the lung resulting in contraction of parenchyma and collapse 4) Loss of normal surfactant (developmental or acquired) results in generalized failure of lung expansion (microatelectasis). Diagram 4.1: Lung Collapse 2.0 ATELECTASIS (Neonatal) Atelectasis is incomplete expansion of neonatal lung (failure of lungs to expand at birth). Aetiology 1. Failure of the respiratory centre 2. Prematurity – lack of surfactant, immaturity of the respiratory centre 3. Hyaline membrane disease 4. Laryngeal dysfunction 5. Obstruction of airway passages 6. Idiopathic 7. Cerebral damage – depresses respiration
- 26. 3.0 ACQUIRED LUNG COLLAPSE Can occur because of resorption atelectasis, compression atelectasis and contraction atelectasis Page 26 Carey Francis Okinda Resorption Atelectasis Occurs because of complete obstruction of an airway resulting in resorption of oxygen trapped in independent alveoli without impairing blood flow through the affected alveoli Lung volume is reduced and hence the mediastinum shifts to towards the atelestatic lung Excessive secretions e.g. mucous plugs or exudates with smaller bronchi may cause the obstruction Seen in bronchial asthma, chronic bronchitis, bronchiectasis, post-operative states and aspiration of foreign bodies Secretions then replace the air and oedema fluid, which become infected quite easily resulting suppuration and tissue destruction that results in irreversible pulmonary fibrosis. Diagram 3.2: Resorption Compression Atelectasis Occurs when pleural cavity is partially or completely filled with fluid exudates; tumours blood or air e.g. pneumothorax and tension pneumothorax Commonly encountered in patients with cardiac failure who develop pleural effusion and patients with neoplastic effusions within pleural cavities Pressure collapse results from compression of the lung tissue from without due to pressure on the visceral pleura fluid or air The mediastinum shifts away from the affected lung
- 27. Diagram 4.3: Compression Atelectasis Page 27 Carey Francis Okinda Causes 1. Pleural effusion 2. Haemothorax 3. Empyema 4. Pneumothorax 5. Haemo-pneumothorax Contraction Atelectasis Occurs when local or generalized fibrotic changes in the lungs/pleural cavity prevent full expansion of the lung. Diagram 4.4: Contraction Atelectasis CLINICAL TASK 1. What are the clinical features of lung collapse? 2. What investigations will be important? 3. What are the differentials?
- 28. Page 28 Carey Francis Okinda Left Side Collapse Upper Lobe Collapsed
- 29. Lesson 5: Bronchial Obstruction and Emphysema Page 29 Carey Francis Okinda Learning Outcomes At the end of the lesson, the learner should be able to - 1. Describe causes and effects of bronchial obstruction and emphysema 2. Diagnose bronchial obstruction and emphysema 3. Investigate bronchial obstruction and emphysema Obstructive Pulmonary Diseases The bronchi have ciliated mucous secreting cells that defend the airways and lungs against bacteria and foreign bodies Chronic irritation of the bronchi leads to hyperplasia and hypertrophy of the mucous secreting glands and goblet cells Obstructive pulmonary diseases affect the airways and are characterized by increased resistance to airway flow due to partial or complete obstruction at any level along the respiratory passages (trachea respiratory bronchioles) The main diffuse obstructive disorders are emphysema, chronic bronchitis, bronchiectasis and asthma Patients with bronchial obstruction have limitations of maximal airflow rates during forced expiration at 1 second (reduced FEV1). Emphysema and chronic bronchitis are grouped together as chronic obstructive pulmonary diseases (C.O.P.D) or chronic obstructive airway diseases (C.O.A.D) COPD refers to patients who have largely irreversible airways obstruction. Key aetiological factors in COPD are smoking (major risk), environmental pollutants (e.g. occupation – mines, dust) andantitrypsin deficiency. Table 1: Disorders of Airflow Obstruction Clinical Anatomic Term site Major Pathologic changes Aetiology Signs/symptoms Chronic Bronchitis Bronchus Mucous gland hyperplasia and hypersecretion Tobacco smoke and pollutants Cough and sputum production Bronchiectasis Bronchus Airway dilatation and scarring Persistent or severe infections Cough, purulent sputum and fever Asthma Bronchus Smooth muscle hyperplasia, excess mucous and inflammation Immunologic or undefined causes Episodic wheezing, cough and dyspnoea Emphysema Acinus Airspace enlargement and wall destruction Tobacco smoke Dyspnoea BRONCHIAL OBSTRUCTION Occurs in various degrees from partial obstruction to complete obstruction affecting small and large bronchi The obstruction, which may be sudden or gradual, results in accumulation of secretions with oedema formation leading to some degree of dilatation of the bronchi
- 30. Secondary bacterial infection ensues producing suppurative bronchitis and by extension suppurative bronchopneumonia. Page 30 Carey Francis Okinda 1.0 CAUSES 1. Tumours - Bronchial carcinoma and Bronchial adenoma 2. Enlarged tracheobronchial lymph nodes – malignancy, tuberculous 3. Inhaled foreign body (FB) 4. Bronchial casts or plugs consisting of inspissated mucous or blood clot 5. Collections of mucous or mucopus retained due to ineffective expectoration 6. Congenital bronchial atresia 7. Fibrous bronchial stricture (post TB) 8. Aortic aneurysm 9. Giant left atrium 10. Pericardial effusion 2.0 EFFECTS 1. Lung collapse - complete obstruction of the bronchioles leads to absorption of the air in the alveoli with the alveolar spaces collapsing. 2. Emphysema (obstructive) - Results in a resonant note on percussion, diminished breath sounds and a displaced mediastinum 3. Secondary infection/suppuration 4. Impaired pulmonary function – dyspnoea and hypoxaemia 5. Features related to obstruction EMPHYSEMA Emphysema is abnormal permanent dilatation/enlargement of airspaces distal to the terminal bronchiole accompanied by destruction of the bronchiole walls without fibrosis It is a constituent of COPD/COAD Diagram 5.1: Emphysema
- 31. Elactase normally inactivated by protease inhibitors (e.g.-1-antitrypsin) .-1-antitrypsin deficiency leads to failure of elastase inactivation Elastases destroy alveolar wall Page 31 Carey Francis Okinda 1.0 AETIOLOGY The main factors are - 1. Smoking – major risk factor that is dose related 2. -antitrypsin deficiency – a protease inhibitor that prevents lung damage especially in smokers 3. Occupation – dusty environments e.g. coal mines 2.0 PATHOGENESIS Is due to imbalance between protease and anti-protease activities in the lung resulting in destruction of the alveolar walls (Anti-protease hypothesis) o -antitrypsin protease inhibitor) is a glycoprotein constituent of globulin in plasma is synthesised in the liver and is usually present in serum and tissue fluids. Protease inhibits protelytic enzymes, which degrade elastin or neutrophil derived elastase. Increased neutrophil infiltration of the lung causes excessive production of elastase o Deficiency of-antitrypsin occurs in homozygous states however in smoking accelerates the damage in heterozygous situations Smoking o Reduces anti-elastase and increases elastolytic protease in the lungs due to oxidants in cigarette smoke which inhibit -antitrypsin and smokers have increased phagocytes and neutrophils in the lungs After the damage the pressure inspired air expands the damaged portion into an emphysematous space With continued enlargement more pressure is required to cause further dilatation resulting in increased dilatation and damage Coughing in chronic bronchitis aggravates the situation Diagram 5.2: Pathogenesis of Emphysema Smoking Neutrophils and macrophages release elastase 3.0 PATHOLOGY Macroscopy Voluminous pale lungs with dilatation of air spaces Microscopy Dilatation of air spaces Destruction of septal wall resulting in thin walls Compressed capillaries Rupture of walls producing honeycombs Emphysema
- 32. Page 32 Carey Francis Okinda 4.0 CLASSIFICATION Classification is based on anatomical distribution within the lobule. a) Centrilobular/centriacinar b) Panaacinar/panlobular c) Paraseptal/distal acinar d) Irregular 4.1. Centrilobular/Centriacinar Predominant in male smokers and chronic bronchitis Central or proximal parts of the acinar are involved Involves enlargement of terminal airspaces and the respiratory bronchioles because of destruction and enlargement of the central or proximal parts of the respiratory unit (the acinar). Distal acinar are spared Associated with cigarette smoking, chronic bronchitis and inflammation of distal airways 4.2. Panacinar (Panlobular) Emphysema Affects all acinar which are uniformly enlarged from the level of the respiratory bronchioles to the terminal blind alveoli Associated with 1-antitrypsin deficiency 4.3. Distal Cinar (Paraseptal) Emphysema Affects distal portion of the acinus Proximal portions of the acinus are spared Usually due to infections accompanied by inflammatory changes and fibrosis 4.4. Irregular Emphysema Acinar irregularly affected Mainly associated with scarring Most common form of emphysema 5.0 CLINICAL FEATURES Cough, expectoration; wheezing; slowly increasing severe exertional dyspnoea; respiratory distress; chest – barrel shaped; hyper-resonant percussion note; hyperventilation; tachycardia; patients are “pink puffers” – they remain well oxygenated and have tachycardia; do not tolerate, hypoxia; Weight loss 6.0 COMPLICATIONS 1) Cor pulmonale 2) Congestive Cardiac failure 3) Pulmonary hypertension TASK Compare and contrast emphysema and chronic bronchitis. State the important investigations
- 33. Lesson 6: Bronchiectasis, Bronchitis and Bronchiolitis Page 33 Carey Francis Okinda Learning Outcomes At the end of the lesson, the learner should be able to - 1. Describe causes and effects of bronchiectasis, bronchitis and bronchiolitis 2. Diagnose bronchiectasis, bronchitis and bronchiolitis 3. Investigate bronchiectasis, bronchitis and bronchiolitis Bronchiectasis 1.0 INTRODUCTION Bronchiectasis is localized or generalized permanent abnormal dilatation of the bronchi or bronchioles (more than 2 mm in diameter) caused by destruction of the muscle and elastic tissue, resulting from or associated with chronic necrotizing infections Usually results from the weakening of the bronchial wall a sequel of destruction of elastic and muscular components of the walls following necrotizing infection of the bronchi and bronchioles. Diagram 6.1: Bronchiectasis 2.0 AETIOLOGY The main categories: - 1. Pulmonary infection 2. Bronchial obstruction
- 34. Page 34 Carey Francis Okinda 3. Associated factors a. Congenital and hereditary conditions e.g. Cystic fibrosis; Intralobular sequestration of the lung; Immunodeficiency states; Kartagener’s syndrome (Bronchiectasis, sinusitis, displacement of viscera (heart) – immobility of the cilia; Congenital bronchiectasis; atelectasis b. Post infection conditions e.g. Necrotising pneumonia caused by bacteria (Myocobacterium tuberculosis, Staphylococcus aureus, Haemophilus influenza and Pseudomonas), viral (HIV, adenoviruses and influenzae), fungal (Aspergillus) c. Bronchial obstruction e.g. tumours, foreign bodies and mucous impaction d. Others e.g. Bronchiolitis and bronchopneumonia in childhood; Rheumatoid arthritis; S.L.E; Inflammatory bowel syndrome; post-transplant 3.0 PATHOGENESIS The major factors in the pathogenesis of bronchiectasis are obstruction and infection. Diagram 6.2: Pathogenesis of Bronchiectasis 3.1. Obstruction Obstruction leads to accumulation and stagnation of secretions Secretion later become infected resulting in an inflammatory reaction that leads to destruction and weakening of the bronchial walls facilitating dilatation of the bronchi. Obstruction reduces mural clearing mechanisms resulting in pooling of secretions distal to the point of obstruction and increases susceptibility to infections. Necrotizing inflammation results in destruction of the bronchi and bronchioles leading to formation of multiple large spaces or cavities. This destruction tends to include the surrounding lung tissue, which heals by fibrosis with resultant obliteration and destruction of smaller bronchi and bronchioles.
- 35. Cavities formed accommodate a lot of secretion within the bronchi, which become infected becoming purulent Without treatment of the infection, the fluid trapped within cavities becomes infected persistently by putrefying microorganisms resulting in formation of purulent fluid that becomes decomposed producing foul smelling breath and sputum. The organisms spread from this focus to the alveoli by air passages or direct spread through the vein forming a septic embolus that forms secondary abscesses (especially in the brain). Diagram 6.3: Pathogenesis - Obstruction Destruction of the bronchi involves ulceration of the bronchial walls. The respiratory passage may wholly or partly be lined by respiratory simple columnar epithelium but later become squamous metaplasia Haemoptysis which may be little or massive occur as bleeding from thin walled vessels in the dilated bronchi/bronchioles. Chronic bronchiectasis leads to haemodynamics changes due to alveolar hypoxia and fibrous obliteration of the pulmonary arteries, which results in enlargement, and development of bronchopulmonary vascular anastomoses. Page 35 Carey Francis Okinda 3.2 Infections Chronic necrotizing inflammation of the bronchial walls causes destruction of the elastic and muscle tissues resulting in damage of the walls leading to dilatation of the bronchi that allows accumulation and stagnation of the secretions that easily become secondarily infected causing further damage of the bronchial wall. Microorganisms associated with this phenomenon are bacterial infection with Mycobacterium tuberculosis, Heamophilus influenzae, Staphylococcus and fibrosing, suppurative pneumonias and corrosive chemicals. Infection may be primary infection of secondary to local obstruction and impaired systemic defence systems. Repeated infections results in increased damage to the airway walls with destruction of the supporting smooth muscle and elastic tissues and eventually fibrosis with further dilatation of the bronchi. The infection also causes necrosis of the walls leading to healing with fibrosis hence dilatation of the bronchi. small bronchi progressively become obliterated due to fibrosis (bronchitis obliterans)
- 36. Diagram 6.4: Pathogenesis – Infections Page 36 Carey Francis Okinda 4.0 PATHOLOGY Macroscopy 1. Dilated bronchi with thickened walls 2. Lumen filled with mucous or muco-pus 3. Firbrotic surrounding lung 4. Dilatation Microscopic 1. Epithelium - normal, ulcerated or squamous epithelium 2. Bronchial wall - infiltrated by acute and chronic inflammatory cells, destruction of muscle and elastic tissues 3. Lung fibrosis 4. Adherent pleura 5.0 CLINICAL FEATURES 1. Severe , persistent/chronic cough 2. Sputum – haemoptysis, foul smelling, purulent 3. Recurrent pneumonia 4. Fever, weight loss, anaemia, weakness 5. Sinusitis 6. Digital clubbing 7. Metastatic abscess 8. Cyanosis 6.0 DIAGNOSIS 1. Bronchophony 2. Bronchoscopy 3. Sputum – colour, volume, cellular component, bacterial infection, Gram stain, culture, white blood cells, bacteriological examination 4. Blood count 5. ECG 6. Urinalysis 7. Oxygen tension 8. Lung function tests What is the relationship between Bronchiectasis and cystic fibrosis?
- 37. Page 37 Carey Francis Okinda 7.0 EFFECTS/COMPLICATIONS 1) Suppuration/empyema 2) Septic emboli (Brain abscess) 3) Pyaemia - brain abscess (metastatic) and meningitis – from involvement of the pulmonary vein 4) Finger clubbing (Hypertrophic pulmonary osteodystrophy) 5) Pulmonary hypertension 6) Cor pulmonalae 7) Amyloidosis 8) COPD 9) Recurrent pneumonia 10) Respiratory failure BRONCHITIS 1.0 Acute Bronchitis This is inflammation of the large and medium bronchi. 1.1. Aetiology 1. Viral - respiratory syncytial virus; rhinovirus; echovirus; parainfluenza types 1, 2 3; Influenza, Herpes viruses, Coxsackie viruses, Corona viruses, Adenoviruses and Measles 2. Mycoplasma - Candida albicans, Candida tropicalis, Histoplasma capsulatum and Cryptococcus neoferans 3. Bacteria (secondary infection) - Strep pneumonia, H. Influeanzae, Strep pyogenes (common in infants, ), Staph aureus (common in infants) and Salmonella typhi Diagram 6.5: Bronchitis
- 38. Page 38 Carey Francis Okinda 1.2. Pathogenesis Invasion by microbes leads to inflammatory reaction by the bronchial epithelium There is activation of the mucous and serous glands leading to production of mucous secretions that cause crackles on auscultation. Spread of the inflammatory reaction to involve bronchioles in debilitated subjects’ results in bronchiolitis and bronchopneumonia, which is fatal. Because of inflammatory oedema, there is reduction in lumen size resulting in wheezing and rhonchi. 1.3. Pathology Macroscopy Congested, swollen/oedematous, hyperaemia and tenacious mucous exudate, sputum – yellow/green Microscopy Congested mucosa with infiltration by neutrophils 1.4. Clinical Features Cough – initially unproductive but later yellow/green sputum. Wheezes/rhonchi, crepitations Shortness of breath Fever Neutrophilia 2.0 Chronic Bronchitis 2.1. Introduction Chronic bronchitis is defined clinically as persistent cough with sputum production on most days for at least 3 months in at least two consecutive years It is not primarily an inflammatory condition but consists of metaplastic changes as a result of chronic irritation of the bronchial epithelium. 2.2. Aetiology 1. Smoking - prolonged cigarette smoking impairs cilia movement, causes hyperplasia and hypertrophy of mucous secreting glands, inhibits function of alveolar macrophages and stimulates the vagus nerve causing bronchoconstriction. 2. Atmospheric pollution - sulphur dioxide, nitrous oxide, toxic fumes and particulate dust particles. 3. Occupational hazards - Cotton mills, Plastic factories 4. Infection- bacterial, viral and myocoplasmal infections occur as a result of bronchitis and predispose to acute exacerbations of chronic bronchitis 5. Familial/genetic factors - poorly understood
- 39. Bronchiolar and Bronchial injury Page 39 Carey Francis Okinda 2.3. Pathogenesis Chronic irritation of the bronchial epithelial cells causes hypertrophy and hyperplasia of the mucous glands leading to excessive secretion of mucous secretions(more goblet cells than ciliated cells) Excessive mucous production and destruction of cilia leads to accumulation of the secretions and exudate in the bronchi and bronchioles causing obstruction. This extends to involve the bronchioles hence bronchiolitis ensues. Destruction of the epithelial causes some areas of ulceration, which heal by fibrosis causing narrowing of the bronchial lumen. Invasion of secretions by bacteria mainly H. influenzae and Strep. pneumoniae results in secondary infection leading to pus formation. Destruction of the epithelia occurs resulting in metaplasia where the squamous epithelium is replaced by columnar epithelium. Diagram 6.6: Evolution of Chronic Bronchitis Bronchospasms 2.4. Pathophysiology Mucous hypersecretion is a physiological response to inhaled irritants Increased secretion impairs normal clearance Impaired cilia function and increased accumulation of mucous secretions Increased susceptibility to acute respiratory infections with bacterial - suppuration. 2.5. Pathology Macroscopy Hyperaemia and oedema of mucous membrane Mucous secretions and increased size of mucous glands Plugging of bronchi and bronchioles Fibrosis and inflammatory changes Microscopy Venous congestion Metaplasia, hypertrophy and dysplasia Inflammatory cells Infections Hyper secretion of mucous Reversible obstruction in bronchioles and small bronchi Chronic Bronchitis Continued and repeated infections Continued and repeated injury (e.g. smoking)
- 40. Increased thickness of the mucosal gland layer (at post mortem, Reid index which is the ratio of glandular layer to the whole thickness is significant if the value is more than 1:2.) Page 40 Carey Francis Okinda 2.6. Differential Diagnosis 1. Bronchial asthma 2. Emphysema 3. COPD 4. Bronchiectasis 5. Chronic pulmonary infections 6. Chronic sinusitis with post-nasal drip 2.7. Complications 1. Respiratory failure 2. Emphysema BRONCHIOLITIS 1.0 INTRODUCTION Bronchiolitis is inflammation of small, intralobular bronchi and bronchioles seen in children, old people and debilitated states. Bronchiolitis is a lower respiratory tract infection usually caused by a virus and occurs in children younger than two years old It is fatal as organisms spread to adjacent acini resulting in bronchopneumonia It is usually caused by a virus which causes inflammation of the small airways (bronchioles) partially or completely blocking the airways resulting in wheezing. Less oxygen enters the lungs, potentially causing a decrease in the blood level of oxygen. Catarrhal bronchitis is characterized by excessive secretion of mucous and increased inflammatory exudate. The mucoid sputum becomes mucopurulet after invasion by bacteria such as Strep. pneumoiae, H. influezae, Strep. pyogenes ad Staph. aureas. In severe cases, superficial layers are sloughed off resulting in ulcer formation (ulcerative bronchitis). Breast-feeding is considered protective and should be encouraged. Breast milk with colostrum rich has high levels of immunoglobulin A (IgA) Infants are affected most often because of their small airways, high closing volumes, and insufficient collateral ventilation 2.0 CAUSES Respiratory syncytial virus (RSV) – most common cause Human metapneumovirus (hMPV) - second most common cause Adenovirus - occasionally causes a similar syndrome with a more virulent course Parainfluenza virus Other less common causes include Mycoplasma pneumonia, Enterovirus, Influenza virus, Rhinovirus, Chlamydophila pneumoniae
- 41. Page 41 Carey Francis Okinda 3.0 RISK FACTORS 1. Low birth weight, particularly premature infants 2. Gestational age (independently associated with hospital resource use and outcome among infants hospitalized for RSV infection) 3. Lower socioeconomic group 4. Crowded living conditions, day-care, or both 5. Parental smoking 6. Chronic lung disease, 7. Severe congenital or acquired neurologic disease 8. Congenital heart disease (CHD) with pulmonary hypertension 9. Congenital or acquired immune deficiency diseases 10. Age less than 3 months 11. Airway anomalies 4.0 PATHOPHYSIOLOGY Bronchioles are small airways (< 2 mm in diameter), lack cartilage, and submucosal glands. The terminal bronchiole, a 16th-generation airway, is the final conducting airway that terminates in the respiratory bronchioles. The acinus (gas exchange unit) consists of respiratory bronchioles, the alveolar duct, and alveoli The bronchiolar lining consists of surfactant-secreting clara cells and neuroendocrine cells, which are the source of bioactive products such as somatostatin, endothelin, and serotonin. Mechanisms 1. Bronchiolar injury and the consequent interplay between inflammatory and mesenchymal cells can lead to diverse pathologic and clinical syndromes. Effects of bronchiolar injury include: a. Increased mucus secretion b. Bronchial obstruction and constriction c. Alveolar cell death, mucus debris, viral invasion d. Air trapping e. Atelectasis f. Reduced ventilation that leads to ventilation-perfusion mismatch g. Laboured breathing 2. Complex immunologic mechanisms - Type 1 allergic reactions mediated by immunoglobulin E (IgE) may account for some clinically significant bronchiolitis. 3. Necrosis of the respiratory epithelium and epithelial regeneration with non-ciliated cells impairs elimination of secretions. 4. Proliferation of goblet cells results in excessive mucus production 5. Cytokines and chemokines - released by infected respiratory epithelial cells, amplify the immune response 6. Airway obstruction was due to epithelial and inflammatory cell debris mixed with fibrin, mucus, and oedema fluid but not to bronchial smooth muscle constriction
- 42. Page 42 Carey Francis Okinda 5.0 CLINICAL FEATURES Symptoms Early symptoms are those of a viral URTI, including mild rhinorrhoea, cough and fever. Fever >39°C Paroxysmal cough and dyspnoea develop within 1-2 days. Wheeze, cyanosis, vomiting, irritability and poor feeding Signs Look for tachypnoea, tachycardia, fever, cyanosis and signs of dehydration. It is unusual for a child to appear 'toxic' (suggested by drowsiness, lethargy, pallor, mottled skin) Mild conjunctivitis, pharyngitis. Evidence of increased respiratory work: intercostal, subcostal and supraclavicular recession, nasal flaring. Widespread fine inspiratory crackles, high-pitched expiratory wheezing Liver and spleen may be palpable due to hyperinflation of the lungs. Diagram 6.7: Features of Bronchiolitis 6.0 PATHOLOGY Virus-induced inflammation of the bronchiolar epithelium, with hypersecretion of mucus and oedema of the surrounding submucosa These changes result in formation of mucous plugs obstructing bronchioles with consequent hyperinflation or collapse of the distal lung tissue Resistance in small air passages is increased during inspiration and expiration, but because airway radius is smaller during expiration, resultant ball valve respiratory obstruction leads to early air trapping and overinflation Atelectasis may occur when obstruction becomes complete and trapped air is absorbed
- 43. Diagnosis and Grading Feature Mild Moderate Severe Wheeze Page 43 Carey Francis Okinda None or end expiratory Entire expiration Inspiratory & Expiratory Feeding Normal Less than usual. Frequently stops feeding. More than ½ normal feeds. Not interested. Gasping / coughing. Less than ½ normal feeds Oxygen No oxygen requirement May require oxygen Requires oxygen In drawing No / mild in drawing Intercostal and / or tracheosternal Severe with nasal flaring Behaviour Normal Some/intermittent irritability Irritability and/or lethargy 7.0 DIFFERENTIAL DIAGNOSIS 1. Asthma 2. Bronchitis 3. Pulmonary oedema 4. Foreign body inhalation 5. Pneumonia 6. Aspiration 7. Cystic fibrosis 8. Pneumothorax 8.0 INVESTIGATIONS 1. Pulse oximetry 2. Nasopharyngeal aspirate for viral cultures for RSV, influenza A and B, parainfluenza and adenovirus 3. CXR a. Children with a clear clinical diagnosis of bronchiolitis do not require a chest x-ray. b. Show signs of hyperinflation, peribronchial thickening, and often-patchy areas of consolidation and collapse 4. Full Blood Count 5. Electrolytes and renal function 6. Blood and urine culture: consider if pyrexia >38.5°C or the child has a 'toxic' appearance. 7. Arterial blood gases: may be required in the severely ill patients, especially in those who may need mechanical ventilation. 9.0 COMPLICATIONS Cyanosis Dehydration: when the normal water content of the body is reduced Fatigue: extreme tiredness and a lack of energy Severe respiratory failure: an inability to breathe unaided Pneumonia Atelectasis Pleural effusion
- 44. Page 44 Carey Francis Okinda Lesson 7: Bronchial Asthma Learning Outcomes At the end of the lesson, the learner should be able to: - 1) Discuss the causes , pathogenesis and pathophysiology of asthma 2) Investigate a patient with asthma 3) Discuss complications of asthma 1.0 INTRODUCTION Bronchial asthma is a chronic relapsing inflammatory disorder characterized by increased responsiveness of the tracheobronchial tree to various stimuli resulting in widespread paroxysmal contraction of bronchial airways due to muscular spasms and plugging by increased thick mucous secretions from the mucosal glands The changes that occur result in a state whereby the respiratory tree is drawn longer with a reduced diameter forming a physiological valve mechanism that leads to easy or normal inspiration and difficult and prolonged expiration The short inspiration and long expiration produces the characteristic wheeze/rhonchi in bronchial asthma. Asthmatic attacks cause shortness of breath and wheezing respirations because of restricted movement of air through tightly constricted air passages Bronchial spasms exert great effect on expiration than inspiration because the calibre of bronchioles varies with the phase of respiration. Diagram 7.1: Anatomical Considerations in Asthma
- 45. Page 45 Carey Francis Okinda 2.0 AETIOLOGY Unclear but associations exist with genetic makeup, atopy or allergy and increased responsiveness of the airways Precipitants include occupational sensitises, allergens, infections and non-specific e.g. cold air, exercise, diet, atmospheric pollution/irritants, dust, vapours, fumes, emotion, drugs e.g. NSAIDS 3.0 AETIOLOGICAL CLASSIFICATION 1. Extrinsic (atopic, allergic) asthma 2. Intrinsic (cryptogenic, non-atopic, idiosyncratic) asthma. 3. Exercise induced asthma 4. Drug induced 5. Occupational asthma 6. Asthma associated with COPD Diagram 7.2: Progression in Asthma Hypersensitivity Hypersensitive airway disease Bronchitis Asthma (overt) 3.1. Extrinsic (Atopic, Allergic) Asthma Commonest type of asthma that has a definite cause associated with the disease as it runs in families and individuals with history of allergy Individuals may have a history of diseases such as rhinitis, urticaria and infantile eczema. Atopic or extrinsic asthma begins in childhood and early adult life Subjects with extrinsic asthma have increased levels of IgE representing type I hypersensitivity reaction mechanisms and they do show characteristic wealing skin reactions to common allergens in the environment. Pathogenesis Exposure of pre-sensitized IgE coated mast cells to allergens (antigens) results in release of chemical mediators in a reaction that first takes place on the mucosal surface and results in the opening of the intercellular tight junctions thereby enhancing penetration of the mast cells by antigens to reach the numerous submuocal mast cells. Direct stimulation of the subepithelial vagal (parasympathetic) receptors provokes bronchoconstriction through both central and local reflexes. This is an acute or immediate response, which consists of bronchoconstriction, oedema, mucous secretion and hypotension (in severe cases). Mast cells release cytokines, which result in influx of leucocytes (neutrophils, monocytes, lymphocytes, basophils and oesinophils) which mediate the late phase reaction together with recruited chemotaxic factors.
- 46. Other sources of mediators of the late phase reaction include the vascular endothelium and airway epithelial cells (produce cytokines in response to infection, drugs and gases. Page 46 Carey Francis Okinda Diagram 7.3: Pathogenesis 3.2. Intrinsic Asthma (Non-atopic) Develops in adult life staring during the middle age and is commonly associated with chronic bronchitis There is a negative family history of the disease as well as personal history of allergy as these individuals fail to reveal a responsive allergen. However, there may be a history of respiratory symptoms compatible with childhood asthma Individuals with intrinsic asthma tend to develop drug hypersensitivity especially with aspirin and penicillin. 3.3. Drug Induced Drugs such as aspirin trigger asthma by inhibiting COX pathway of arachidonic acid metabolism without affecting the lipoxygenase route thus resulting in increased production of bronchoconstritive leukotrienes. 3.4. Exercise Induced Is a phenomenon that can occur in isolation or in association with any type of asthma Many patients experience airway obstruction, 5 to 20 minutes after completing the exercise or in the course of it, by a mechanism that seems to
- 47. include the cooling, the relative dryness of the airway secondary to increased ventilation and loss heat the air. The precise pathophysiology remains unclear, but may involve heat and Page 47 Carey Francis Okinda water loss from the airway The osmotic hypothesis proposes that this water loss leads to dehydration and hyperosmolarity of the airway surface liquid causing the release of water from airway cells. This water loss results in cell shrinkage, vascular leak and the release of mediators, which cause airway smooth muscle contraction, edema, and bronchoconstriction. This shift in water from the cells and the subsequent regulatory volume increase most likely involve alterations in ion channels and signalling pathways The thermal hypothesis proposes that the rapid rewarming of the airway following heat loss during exercise is associated with a reactive hyperemia of the bronchial vasculature, which results in congestion of the vascular bed and airway obstruction. 3.5. Occupational Asthma Occupational asthma is stimulated by fumes (epoxy resin, plastics), organic and chemical dusts (wood, cotton, platinum), gases (toluene), chemicals (formaldehyde and penicillin products). 4.0 PATHOGENESIS AND PATHOPHYSIOLOGY The pathogenesis of bronchial asthma pivots around: -airway hypersensitivity, inflammation and airway obstruction 4.1. Airway Hypersensitivity (hyperesponsiveness) There is increased responsiveness of the respiratory airways of the lung to allergens in the environment whose inhalation triggers an immediate acute response initiated by IgE sensitised mast cells in the mucosal surface of the respiratory tree Mast cells degranulate releasing mediators of inflammation such as histamine, leukotrienes, prostaglandins and platelet aggregating factor (PAF) and chemostatic factors for oesinophils and neutrophils The respiratory tree is hypersensitive to normal allergens, which can trigger off reactions. These allergens include inhaled and non-inhaled ones. The inhaled allergens include - aeroallergens (house dust mites, pollens, animal dander and fungal spores) air pollution, extreme cold. The non-inhaled are exercise and ingested substances. 4.2. Inflammation and oedema Following the hypersensitivity reaction and release of mediators of inflammation, there ensues an inflammatory reaction that results in oedema formation, bronchoconstriction and hypersecretion of mucous and accumulation of oesinophils and neutrophils. There is infiltration of the airways with inflammatory cells, Thelper lymphocytes, oesinophils and mast cells, which is a common feature in asthma.
- 48. 4.3. Airway Obstruction/bronchoconstriction The pathologic basis of airway obstruction is: - 1. Constriction of the airway’s smooth muscles due to release of bioactive mediators and neurotransmitters. 2. Thickening of the airway epithelium due to oedema formation 3. Presence of liquids and mucous secretions within the confines of the Page 48 Carey Francis Okinda bronchial lumen 4.4. Airway remodelling In some patients permanent structural changes can occur in the airway The changes are associated with a progressive loss of lung function that is not prevented by or fully reversible by current therapy Airway remodelling involves an activation of many of the structural cells, with consequent permanent changes in the airway that increase airflow obstruction and airway responsiveness and render the patient less responsive to therapy The changes can include thickening of the sub-basement membrane, subepithelial fibrosis, airway smooth muscle hypertrophy and hyperplasia, blood vessel proliferation and dilation, and mucous gland hyperplasia and hyper secretion 4.5. Cells Involved Mast Cells The number is increased in the respiratory epithelium and surface secretions They cells generate and release powerful smooth muscle and vasoactive mediators such as histamine, prostaglandin D2 (PD2) and leukotrienes C4 (LTC4) that cause the immediate asthmatic reaction. Note that 2 adrenoreceptor e.g. salbutamol inhibit release of mediators by the mast cells. The Epithelium Shed during exacerbations of asthma resulting in desquamations, which increase permeability of the airway to inhaled allergens and exposure of nerve fibre endings Desquamated materials from the columnar epithelium can be identified in the sputum as twisted strips called Curschmann’s spirals Inflamed epithelium produces mediators such as cytokines, granulocytes macrophage colony stimulating factor (GM-CSF) that prolong the life of tissue oesinophils, TNF and interlukins that capture the inflammatory cells within the epithelium. Inflammatory Cells i). Macrophages and Lymphocytes - are abundant in the mucous membranes of the airways and alveoli. ii). Oesinophils - are abundant in bronchial secretions and when activated they release mediators such as PAF and LTC4, major basic protein (MBP) and
- 49. eosinophil cationic protein (ECP) which are toxic to epithelial cells. Oedema, vascular congestion and infiltration by oesinophils produce the Charcot Leyden crystals. iii). Vascular Epithelium - exhibits congestion, leakage, increased permeability and contraction. 2 agonists and theophylline can prevent the contraction. Page 49 Carey Francis Okinda 4.6. Nerves Exposure of the nerve endings especially C-fibre afferent nerves leads to release of neurotransmitters such as substance P, neurokinin (NK) A and calcitonin gene-related peptide (CGRP) which are tachykinins that increase the inflammatory response This usually contributes to bronchoconstriction, microvasculature leakage and mucous secretion Vasoactive intestinal peptide (VIP) and nitric oxide are potent neurotransmitters that are rapidly degraded in inflammation resulting in bronchoconstriction and adrenergic systems of the autonomic nervous system are activated resulting in increased release of mediators from the mast cells but the cholinergic system, which is extensive in the smooth muscles of the respiratory passages remains normal, is asthma. 5.0 PATHOLOGY Macroscopy (at autopsy) Overinflated lungs that do not deflate when the thorax is opened Widespread plugging of airways with thick mucous Diagram 7.4: Pathological Changes in Asthma Microscopy Desquamation of the epithelium Hypertrophy of smooth muscle Thickening of the basement membrane Infiltration by oesinophils and inflammatory cells
- 50. Hyperplasia of mucosal glands Goblet cell metaplasia Curschmann’s spirals – mucosal plugs containing normal or desquamated epithelium forming twisted strips. Charcot Leyden crystals – sputum containing numerous oesinophils and diamond shaped crystals derived from eosinophils. Outline the clinical classification of asthma stating the main clinical features Page 50 Carey Francis Okinda 6.0 CLINICAL FEATURES Clinical features of asthma vary with age, severity, duration of disease, amount and nature of treatment and presence of complications. Main Features include – cough, headache, difficulty in breathing, hyperventilation, wheezing and chest pain/tightness Severe asthma o Inability to complete a sentence in one breath o Respiratory rate > 25 breaths per minute o Tachycardia > 110 (pulsus paradoxicus) o PEFR< 50% of predicted normal best Life threatening asthma o Silent chest, cyanosis or feeble respiratory effort o Exhaustion, confusion or coma o Bradycardia, hypotension o PEFR< 30% TASK 7.0 DIFFERENTIAL DIAGNOSIS Common 1. Acute bronchiolitis (infections, chemical) 2. Aspiration (foreign body) 3. Bronchial stenosis 4. Cardiac failure 5. Chronic bronchitis 6. Cystic fibrosis 7. Eosinophilic pneumonia Uncommon 1. Airway obstruction due to masses a. External compression (thoracic, superior vena cava syndrome, substernal thyroid) b. Intrinsic airway – pulmonary lung cancer and metastatic breast cancer 2. Pulmonary emboli
- 51. 8.0 INVESTIGATIONS 1. Lung Function tests – diagnosis of asthma is based on demonstration of a > 15% improvement I FEV1 or PEFR following inhalation of a bronchodilator. Peak flow charts – take PEFR on walking, middle of the day and before bed. It shows reduced PEFR, MMEFR Page 51 Carey Francis Okinda Reduced FEV1 Diagram 7.5: Lung Volumes Diagram 7.6: FEV Note: FEV1 is reduced in obstructive disease > in restrictive disease FEV1 x 100/sec (the normal ratio is 80 – 97%) FVC During an asthmatic attack FEV1 is greatly reduced while FVC is increased hence, the ration is markedly reduced 2. Exercise tolerance 3. Analysis of arterial gases Check for the partial pressures of oxygen and carbon dioxide (normal - oxygen PaO2 is over 12 kPa (90 mmHg) and PaCO2 is less than 6.0 kPa (45 mmHg). This is reversed in asthma due to carbon dioxide retention resulting from the physiological valve.
- 52. 4. Haemogram - increased haemoglobin, normal WBC (only increase in the presence of an infection), eosinophils> 0.4 x 109/L 5. Sputum Examination - Charcot Leyden spirals, Curschmann’s crystals, Page 52 Carey Francis Okinda White blood cells 6. Bronchial provocation test (is not done if the FEV1 is < 1.5 litres) 7. Chest X-ray - shows hyperinflation, depressed diaphragm and excludes pneumothorax (a complication) 8. Skin test 9. Allergen provocation test 9.0 COMPLICATIONS 1. Pneumothorax 2. Pneumomediastinum 3. Respiratory failure 4. Heart failure/CCF/Cor Pulmonale 5. COPD 6. Pneumonia 7. Lung Collapse What is the pathophysiology of these complications?
- 53. Lesson 8: Restrictive Pulmonary Diseases Alveolitis Inflammatory destruction of pulmonary parenchyma Page 53 Carey Francis Okinda Leaning Outcomes At the end of the lesson, the learner should be able to - 1) Classify restrictive diseases of the lungs 2) Describe the pathogenesis and pathology of restrictive lung diseases 3) Investigate patients with restrictive lung diseases 1.0 INTRODUCTION A group of lung diseases that cause reduced compliance of the lungs resulting in difficult to expand with respiration usually because of abnormalities of alveolar walls which are rigid due to oedema or fibrosis ARLD is characterized by oedema and exudation CRLD diseases present with inflammation and fibrosis and is characterized by reduced expansion of the lung parenchyma with reduced total lung capacity. 2.0 CLASSIFICATION There are three types: - 1. Restriction due to chest wall disorders such as: - kyphosis, poliomyelitis and severe obesity 2. Pleural diseases (see later in the unit) 3. Restriction due to interstitial and infiltrative diseases characterized by non-infectious involvement of interstitial connective tissue of the lung parenchyma 3.0 PATHOGENESIS Characterized by damage to the alveolar walls resulting in haemorrhage and high protein exudation into the alveolar producing the hyaline membrane disease; oedema and inflammation of interstitium and fibrosis in the interstitial. Diagram 8.1: Pathogenesis of Restrictive Lung Disease Stimuli Inflammation Increased accumulation of lymphocytes, macrophages, neutrophils, oesinophils Widespread destruction - “HONEYCOMB” lung Fibrosis
- 54. Find out the inorganic (mineral dusts) and organic (biologic) dusts Page 54 Carey Francis Okinda 4.0 CLINICAL FEATURES 1) Dyspnoea 2) Tachycardia 3) End-inspiratory crackles 4) Cyanosis without wheezing or evidence of airway obstruction 5) CXR shows diffuse infiltration by small nodules, irregular lines and grand glass shadows 6) Secondary pulmonary hypertension 7) Right heart failure/Cor pulmonale 8) Reduced CO diffusing capacity 9) Reduced lung volume 10) Reduced lung compliance 5.0 PNEUMOCONIOSIS Lung disease caused by inhalation of dust (dust diseases/occupational lung disease) Type of disease produced varies according to the nature of the dust causing the problem Extent of damage caused by inhaled gases is determined by - 1. Size and shape of the particles 2. Solubility and physiochemical composition 3. Amount of dust retained in the lungs 4. Additional effects of other irritants such as tobacco. 5. Host factors – efficiency in clearing mechanisms and immune status Tissue response will include – 1. Fibrous nodules e.g. coal-workers pneumonitis and silicosis 2. Interstitial fibrosis e.g. asbestosis 3. Hypersensitivity reactions – e.g. in berylliosis 6.0 FIBROSING LUNG DISEASE (INTERSTITIAL LUNG DISEASE) Fibrosing lung disease is characterized by chronic inflammation in the walls of the alveoli resulting in progressive diffuse fibrosis in the lung parenchyma Presents with dyspnoea and dry cough Cause of Chronic Interstitial Lung Disease 1) Idiopathic interstitial pneumonitis (interstitial pneumonia) 2) Connective tissue disease e.g. rheumatoid disease 3) Drug induced damage e.g. cytotoxics 4) Atypical pneumonia (Chlamydia, Mycoplasma) 5) Pneumonia 6) Extrinsic allergic alveolitis 7) Sarcoidosis 8) Radiation damage
- 55. Page 55 Carey Francis Okinda 7.0 SILICOSIS Caused by prolonged exposure to silicon dioxide (silica/quartz) Common in slate mining, metal foundries, stone masonry, tunnelling, granite quarrying and coal mining Lung lesions slowly progress over many years Damages lung macrophages and if the exposure is chronic thus leads to death of macrophages There is release of cytokines, which enhance fibrosis. A silicotic lung is susceptible to tuberculosis Clinical Features Dyspnoea Complications 1. Obstructive pulmonary disease 2. pulmonary tuberculosis 3. rheumatoid arthritis (Caplan’s syndrome) 4. Cor pulmonale 8.0 ASBESTOSIS Causes lung and pleural diseases Produces pleural plaques, pleural effusions, visceral pleural fibrosis, asbestosis (chronic progressive fibrosis of the lung), malignant mesothelioma (a highly malignant lung tumour) and cancer of the lung (bronchogenic carcinoma). Clinical Features Insidious onset, dyspnoea, cough – dry or productive, pulmonary hypertension, cor pulmonale and various forms of cancer 9.0 ADULT ACUTE RESPIRATORY DISTRESS SYNDROME ARDS is a manifestation of diffuse alveolar damage with widespread systemic metabolic derangements Diagnosis depends on presence of precipitant ARDS, refractory hypoxaemia (PaO2< 8.0 kPa in > 40% O2), radiological evidence of evolving pulmonary shadowing and clinical signs of lungs being abnormally rigid with low total compliance. Causes 1) Major trauma especially associated with increased intracranial pressure 2) Septicaemia 3) Pulmonary aspiration of gastric contents 4) Major burns 5) Inhalation of toxic fumes or smoke 6) Near drowning 7) D.I.C
- 56. Progression to fibrosis of alveoli Restrictive lung disease Hypoxia Respiratory failure Page 56 Carey Francis Okinda 8) Massive blood transfusion 9) Acute pancreatitis 10) Radiation injury Pathogenesis Diagram 8.2: Pathogenesis of ARDS 10.0 IMMUNOLOGIC LUNG DISEASE Immunologic mechanisms play a crucial role in lung disease as outlined in the table below Table 1: Pathophysiology of Restrictive Lung Diseases Disease Pathogenesis/pathology Bronchial asthma Explain Hypersensitivity (allergic) pneumonitis Immune mediated inflammation of the lung tissues - Examples – Farmer’s lung, Bird breeders lung, Malt workers lung, Mushroom workers lung Pulmonary Eosinophilia Immunological meditated lung diseases characterized by infiltration of the lungs and elevated eosinophil counts e.g. Loeffler’s syndrome Good Pastures Syndrome Necrotizing haemorrhagic interstitial pneumonitis 11.0 VASCULAR COLLAGEN DISEASE Table 2: Pathogenesis of Restrictive Lung Disease in Vascular Collagen Disease Disease Pathogenesis/pathology Rheumatoid arthritis Pleural effusion; Interstitial pneumonitis; Rheumatoid pneumoconiosis S.L.E Pleurisy; Pleural effusion; Interstitial pneumonitis; Pulmonary haemorrhage; Vasculitis “Honeycomb” lung with numerous cysts especially in the lower lobes Right Ventricular Failure Pulmonary hypertension Right ventricular hypertrophy Compare and contrast obstructive and restrictive lung diseases
- 57. Lesson 9: Pulmonary Infections – Pneumonia Page 57 Carey Francis Okinda Learning Outcomes 1) Identify causes of pulmonary infections 2) Discus predisposing factors to pulmonary infections 3) Describe the pathology of different types of pneumonia 4) Investigate pneumonia 1.0 INTRODUCTION Respiratory tract infections are more frequent than any other infections. Majority URTIs are caused by viruses (common cold, pharyngitis) while bacterial, viral, mycoplasmal and fungal infections of the lung (pneumonia) Acute and chronic pulmonary infections which are frequent causes of death are common at all ages and occur when normal lung or systemic defence mechanisms are impaired Impairment of the defence mechanisms includes - 1. Loss or decreased/suppression of cough reflex leading to aspiration 2. Injury to mucociliary apparatus by cigarette smoking and gaseous inhalation, genetic disorders, inhalation of corrosive substances 3. Decreased phagocytic or bactericidal function of the alveolar macrophages 4. Pulmonary oedema or congestion (congestive cardiac failure) 5. Accumulation of secretions e.g. Post-operative , cystic fibrosis and bronchial obstruction Defective innate immunity (neutrophil and complement defects) and humoral immunodeficiency) result in increased incidence of infections with pyogenic bacteria Defects in cell mediated immunity lead to increased infections with intracellular microbes e.g. mycobacterium and herpes viruses and Pneumocystis jiroveci 2.0 DEFINITION Pneumonia is inflammation of the lung parenchyma distal to the terminal bronchioles (respiratory bronchiole, alveolar ducts, alveolar sacs and alveoli) characterized by vascular changes and exudation of fluid and cells Inflammation may reach the pleural surface causing irritation and inflammation of the pleura and accumulation of fluid exudate (pleural effusion). The process is influenced by the spongy character of the lung that allows unimpeded spread of the inflammatory exudate filling the alveolar and affected portions of the lung become relatively solid (consolidation). 3.0 PREDISPOSING FACTORS Viral infections, hospitalization, cigarette smoking, alcohol excess, bronchiectasis, bronchial obstruction, immunosuppression, intravenous drug use, inhalation, crowding, post operation How would these factors predispose individuals to pulmonary infections?
- 58. Page 58 Carey Francis Okinda 4.0 ROUTES OF INFECTION 1. Inhalation of microbes present in the air 2. Aspiration – naso and oropharynx 3. Haematogenous spread from a distant foci of infection 4. Direct spread from an adjacent site of infection 5.0 PATHOGENESIS A number of defence mechanisms at different levels normally protects the lung and failure of the defence mechanisms and presence of predisposing factors results in development of pneumonia. Such situations include - a) Altered consciousness - oropharyngeal contents can be aspirated into the lungs in states of unconsciousness e.g. coma, cranial trauma, seizures, cerebro-vascular accidents, drug overdose and alcoholism. b) Depressed cough and gag reflexes - allows aspiration of gastric contents e.g. in old age, pain from trauma, thoraco-abdominal surgery, neuromuscular disease, malnutrition, kyphoscoliosis, severe obstructive pulmonary disease, endotracheal intubation and tracheostomy c) Impaired mucociliary transport - impairment or destruction of the mucous-covered ciliated epithelium as in cigarette smoking, respiratory viral infections, immotile cilia syndrome, inhalation of hot or corrosive gases and old age. d) Impaired alveolar macrophage function - cigarette smoking, hypoxia, starvation, anaemia, pulmonary oedema and viral respiratory infections. e) Endobronchial obstruction - interferes with effective clearance of the bronchial tree f) Leucocyte dysfunctions - congenital and acquired immunodeficiency, HIV/AIDS and granulocyte abnormalities.
- 59. Page 59 Carey Francis Okinda 6.0 INVESTIGATIONS 1) Chest x-ray PA and lateral view o Chest radiography may reveal a lobar consolidation (common in typical pneumonia most commonly in the lower lobes; or it could show bilateral diffuse interstitial infiltrates and cavitations. o Used to evaluate for complications of pneumonia like empyema, lung abscess, pneumothorax etc. o Gives a clue for suspecting the aetiological agent. Multi lobar involvement (Bacteraemic pneumococcal) Pleural effusions (Bacteraemic pneumococcal) Lymphadenopathy (Mycoplasma infection) Multilobe involvement, cavitation, or spontaneous pneumothorax (Staphylococus aureus). Upper lobe preponderance may denote klebsiella pneumonia. 2) Chest CT (computed tomography) can reveal pneumonia that is not seen on chest x-ray 3) HIV serology 4) Lung Function Tests 5) Blood picture o Show a high blood cell count, indicating the presence of bacterial infection. o Leucopenia may suggest viral pneumonia. 6) Sputum gram stain and culture o The presence of > 25 white blood cells and, 10 squamous epithelial cells per high power field suggests that the sputum is appropriate for examination. o Specialized cultures for Mycobacterium sp., Legionella sp., and endemic fungi may be valuable in the appropriate clinical circumstance. If the patient is not receiving antibiotics at the time of admission 7) Sputum culture and sensitivity results may be useful 8) Blood culture 9) Urea and electrolytes 10) Blood chemistry a) Glucose b) Electrolytes c) Liver and renal function tests 11) Pulse oximetry 12) Arterial Blood Gases – If oxygen saturation < 90% 13) Serum antibodies - Detection of antibodies to Streptococcus pneumonia, mycoplasma, chlamydia, adenovirus, influenza A and B viruses, parainfluenza viruses 1, 2, and 3, and respiratory syncytial virus etc. 14) Polymerase Chain Reaction (PCR) - useful for identifying certain atypical bacteria strains, including mycoplasma, Chlamydia pneumonia and Haemophilus influenzae type b. One study found that using a real-time PCR