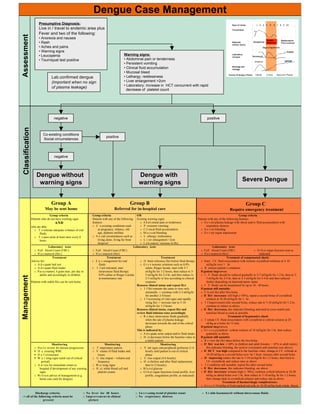
Dengue algorithm
- 1. Dengue Case Management Presumptive Diagnosis: Live in / travel to endemic area plus Fever and two of the following: Assessment • Anorexia and nausea • Rash • Aches and pains • Warning signs • Leucopenia Warning signs: • Tourniquet test positive • Abdominal pain or tenderness • Persistent vomiting • Clinical fluid accumulation • Mucosal bleed Lab.confirmed dengue • Lethargy; restlessness (important when no sign • Liver enlargement >2cm • Laboratory: Increase in HCT concurrent with rapid of plasma leakage) decrease of platelet count negative positive Classification Co-existing conditions positive Social circumstances negative Dengue without Dengue with warning signs warning signs Severe Dengue Group A Group B Group C May be sent home Referred for in-hospital care Require emergency treatment Group criteria Group criteria OR Group criteria Patients who do not have warning signs Patients with any of the following Existing warning signs: Patients with any of the following features. AND features: o A b d o minal pain or tenderness o S e v ere plasma leakage with shock and/or fluid accumulation with who are able: o C o-existing conditions such o P ersistent vomiting respiratory distress o T o tolerate adequate volumes of oral as pregnancy, infancy, old o C l i nical fluid accumulation o S e v ere bleeding fluids age, diabetes mellitus o M u c o sal bleeding o S e v ere organ impairment o T o pass urine at least once every 6 o S o cial circumstances such as o L ethargy/ restlessness hours living alone, living far from o L i ver enlargement >2cm hospital o L a b oratory: increase in Hct Laboratory tests Laboratory tests Laboratory tests o Full blood Count (FBC) o Full blood Count (FBC) o Full blood Count (FBC) o O t h er organ function tests as o H a e matocrit (Hct ) o H a e matocrit (Hct) o H a e matocrit (Hct) indicated Treatment Treatment Treatment Treatment of compensated shock: Advice for: o E n c ouragement for oral o O btain reference Hct before fluid therapy o Start I.V. fluid resuscitation with isotonic crystalloid solutions at 5-10 o A d e quate bed rest fluids o G i v e isotonic solutions such as 0,9% ml/kg/hr over 1 hr o A d e quate fluid intake o I f not tolerated, start saline, Ringer lactate, start with 5-7 o R eassess patient’s condition, o P a r a c etamol, 4 gram max. per day in intravenous fluid therapy ml/kg/hr for 1-2 hours, then reduce to 3- If patient improves: adults and accordingly in children 0,9% saline or Ringer Lactate 5 ml/kg/hr for 2-4 hr, and then reduce to o I . V. fluids should be reduced gradually to 5-7 ml/kg/hr for 1-2 hr, then to 3- Management at maintenance rate 2-3 ml/kg/hr or less according to clinical 5 ml/kg/hr for 2-4 hr, then to 2-3 ml/kg/hr for 2-4 hr and then reduced Patients with stable Hct can be sent home response further depending on haemodynamic status Reassess clinical status and repeat Hct o I . V. fluids can be maintained for up to 24 - 48 hours o I f Hct remains the same or rises only If patient still unstable: minimally -> continue with 2-3 ml/kg/hr o C h eck Hct after first bolus for another 2-4 hours o If Hct increases/ still high (>50%), repeat a second bolus of crystalloid o I f worsening of vital signs and rapidly solution at 10-20 ml/kg/hr for 1 hr. rising Hct -> increase rate to 5-10 o I f improvement after second bolus, reduce rate to 7-10 ml/kg/hr for 1-2 hr, ml/kg/hr for 1-2 hours continue to reduce as above. Reassess clinical status, repeat Hct and o If Hct decreases, this indicates bleeding and need to cross-match and review fluid infusion rates accordingly transfuse blood as soon as possible o R e duce intravenous fluids gradually Treatment of hypotensive shock when the rate of plasma leakage o I nitiate I.V. fluid resuscitation with crystalloid or colloid solution at 20 decreases towards the end of the critical ml/kg as a bolus for 15 min phase. If patient im p r o v e s This is indicated by: o G i v e a crystalloid / colloid solution of 10 ml/kg/hr for 1 hr, then reduce o A d e quate urine output and/or fluid intake gradually as above o H ct decreases below the baseline value in If patient still unstable a stable patient o R e view the Hct taken before the first bolus Monitoring Monitoring Monitoring o If Hct was low (<40% in children and adult females, < 45% in adult males) o D a i l y review for disease progression: o T emperature pattern o V ital signs and peripheral perfusion (1-4 this indicates bleeding, the need to crossmatch and transfuse (see above) ! D e creasing WBC o V olume of fluid intake and hourly until patient is out of critical o If HCT was high compared to the baseline value, change to I.V. colloids at ! D e f ervescence losses phase 10-20 ml/kg as a second bolus over to 1 hour; reassess after second bolus ! W a r ning signs (until out of critical o U rine output – volume and o U rine output (4-6 hourly) o If improving reduce the rate to 7-10 ml/kgt/hr for 1-2 hours, then back to period) frequency o H ct (before and after fluid replacement, I.V. crystalloids and reduce rates as above o A d vice for immediate return to o W a r ning signs then 6-12 hourly) o I f condition still unstable, repeat Hct after second bolus hospital if development of any warning o H ct, white blood cell and o B l o o d glucose o If Hct decreases, this indicates bleeding, see above signs platelet counts o O t h er organ functions (renal profile, liver o If Hct increases/ remains high (> 50%), continue colloid infusion at 10-20 o W r i t t e n advice of management (e.g. profile, coagulation profile, as indicated) ml/kg as athird bolus over 1 hr, then reduce to 7-10 ml/kg /hr for 1-2 hours, home care card for dengue) then change back to crystalloid solution and reduce rate as above Treatment of haemorrhagic complications: o G i v e 5-10 ml/kg of fresh packed red cells or 10-20 ml/kg fresh whole blood Discharge criteria: o No fever for 48 hours o I n c r e asing trend of platelet count o S t able haematocrit without intravenous fluids -> all of the following criteria must be o Improvement in clinical o No respiratory distress present picture
