An Atlas of Musculoskeletal Oncology: Volume 4
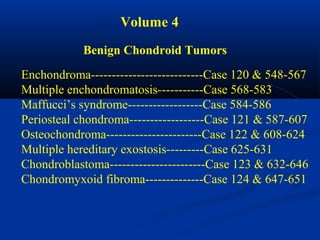
- 1. Volume 4 Benign Chondroid Tumors Enchondroma---------------------------Case 120 & 548-567 Multiple enchondromatosis-----------Case 568-583 Maffucci’s syndrome------------------Case 584-586 Periosteal chondroma------------------Case 121 & 587-607 Osteochondroma-----------------------Case 122 & 608-624 Multiple hereditary exostosis---------Case 625-631 Chondroblastoma-----------------------Case 123 & 632-646 Chondromyxoid fibroma--------------Case 124 & 647-651
- 2. Chondroid forming Tumors
- 3. Enchondroma
- 4. Enchondroma The enchondroma is one of the most common benign tumors seen in the skeletal system. It is centrally located and in 50% of the cases will be found in small tubular bones of hands and feet where it arises as a hamartomatous process and frequently remains un- diagnosed throughout the life of the patient until which time as they develop a pathologic fracture thru the lesion. The lesions have a typical geographic pattern with sharp margination and frequently demonstrate matrix calcification, especially as the patient ages. In the hand or foot, the lesions frequently cause marked thinning of the surrounding cortex and dilatation of the bone, whereas with enchondromas found in larger bones, there is minimal evidence of cortical invasion and little if any evidence of cortical thinning or dilatation. It is rare for an enchondroma to convert into a chondosarcoma in the hand or foot, but in larger bones such as the femur or pelvis a primary enchondroma can
- 5. convert very gradually into a low grade chondrosarcoma. The incidence of conversion is less than 5% of cases and almost always in adults. In most cases, the enchondroma will be discovered as an incidental finding, because it is asymptomatic and non-disabling. There is no particular need to biopsy or bone graft the lesion unless the patient develops an interest in a specific sport or occupational activity that would put him at risk for fracture. If an acute fracture occurs, it is best to wait until the fracture heals and then consider the patient for a bone grafting procedure at a later date.
- 6. CLASSIC Case #120 38 year female enchondroma distal femur
- 7. Bone scan
- 8. Coronal T-1 MRI tumor
- 9. Coronal T-2 MRI tumor
- 11. Tumor seen thru cortical window
- 13. tumor Photomic
- 14. Closer up
- 15. High power
- 16. Curettement completed and ready for cement
- 18. Post op x-ray tumor cavity filled with radiolucent cement
- 19. Case #548 periosteal chondroma 57 year female enchondroma entire femur Smaller periosteal chondroma proximal and posterior femur
- 20. Biopsy photomic
- 21. Post op x-ray following removal of periosteal portion
- 22. 8 year followup with placement of a long stem THA for stress pain symptoms
- 23. Case #549 48 year female enchondroma femur
- 24. Bone scan
- 25. Case #550 59 year female enchondroma distal femur
- 26. Case #550.1 Enchondroma distal femur in a 60 year male
- 27. Bone scan
- 28. Cor T-1 Cor T-2 Cor Gad
- 29. Sag T-1 Sag T-2
- 31. Case #551 62 year male enchondroma proximal humerus
- 32. Coronal T-1 MRI
- 33. CT scan
- 36. Case #552 degenerative arthritis 70 year male with enchondroma proximal humerus
- 37. Coronal T-1 MRI
- 38. Sagittal T-2 MRI
- 39. Case #553 58 year female enchondroma proximal humerus
- 40. Case #554 42 year female enchondroma tumor proximal humerus
- 41. Case #554.1 Enchondroma and ganglion cyst 47 year male with shoulder pain for 6 months
- 42. ganglion enchondroma cyst Coronal T-2 MRI
- 43. Sagittal T-2 enchondroma Sagittal T-2 ganglion
- 44. ganglion Two different T-2 axial cuts showing the enchondroma and the right cut shows the ganglion
- 45. Case #555 55 year male enchondroma tibia
- 46. Bone scan
- 47. Coronal T-1 MRI
- 48. Coronal T-2 MRI tumor
- 49. Biopsy photomic
- 50. Case #556 55 year male with enchondroma tibia
- 51. Lateral view
- 52. Axial T-1 MRI
- 54. Biopsy photomic
- 55. Case #557 40 year female with enchondroma fibula
- 56. Bone scan
- 57. Sagittal T-1 MRI
- 58. Axial T-1 MRI
- 59. Case #558 22 year male with enchondroma proximal phalanx
- 60. Biopsy photomic
- 61. Case #559 Periosteal chondroma enchondroma 33 year female with periosteal chondroma and enchondroma in same ray
- 62. Oblique view
- 63. Case #560 Pathologic fracture enchondroma proximal phalanx thumb 29 year male
- 64. Case #561 23 yr male with path fracture thru enchondroma thumb
- 65. Case #562 31 year female with enchondroma great toe
- 67. Photomic
- 68. Case #564 11 yr boy with enchondroma lst metatarsal
- 69. Case #565 26 year male with enchondroma 5th metatarsal
- 70. Case #566 17 year male with enchondroma os calcis
- 71. Os calcis view
- 72. Case #567 28 year female enchondroma scapula
- 74. Multiple Enchondromatosis (Ollier’s) Multiple enchondromatosis or Ollier’s disease, is a rare non- familial cartilagenous dysplasia that is typically seen on one half of the body and appears similar to fibrous dysplasia. Extensive disease of the metaphyseal areas of long bone can result in bowing and shortening. In the case of the femur a major bowing is seen distally compared to the proximal bowing seen in fibrous dysplasia. The cortical thinning and epiphyseal involvement seen Ollier’s disease is rarely seen in solitary enchondromas. The chance for malignant conversion to a low grade chondrosarcoma in adult life is only about 25%.
- 75. CLASSIC Case #568 3 year male with multiple enchondromatosis
- 76. Extremities
- 77. Macro section
- 78. Photomic
- 79. Case #569 6 year male Ollier’s disease
- 80. Same patient
- 81. Case #570 4.5 year male Ollier’s tibia
- 82. Case #571 71 year female with Ollier’s left lower extremity
- 83. Lateral view of knee
- 84. Photomic
- 85. Failure following resurfacing TKA because of loosening
- 86. Post op x-ray with constrained TKA
- 87. X-ray of cemented stem distal femoral resection prosthesis
- 88. Case #572 15 year female Ollier’s disease
- 89. AP close up knee
- 90. Forearm disease
- 91. Case #573 18 year male Ollier’s pelvis and ribs
- 92. Case #574 2 year male Ollier’s lower extremity
- 93. Case #575 28 year male Ollier’s upper extremity
- 94. Multiple sites in radial half of hand
- 95. AP x-ray
- 96. Case #576 19 year male Ollier’s femur
- 97. Case #577 22 year male with Ollier’s of the hand
- 98. tumor Macro section of amputation specimen
- 99. tumor Close up view of macro section
- 100. Case #578 40 year female with Ollier’s of the hand
- 101. Case #579 10 year male Ollier’s hand
- 102. Case #580 30 year female Ollier’s hand
- 103. Case #581 3 year male Ollier’s hand
- 104. Case #582 19 year male Ollier’s feet
- 105. Case #583 5 year female with Ollier’s of hand ready for surgery
- 106. X-ray of both hands
- 107. Photo of deformed feet after hand surgery
- 108. Close up of deformed foot
- 109. Multiple Enchondromatosis Plus Soft tissue Hemangiomatosis Maffucci’ Disease
- 110. Maffucci’s Syndrome Patients with multiple enchondromatosis or Ollier’s disease will on occasion develop soft tissue hemangiomatosis in the same areas as the enchondromatosis is seen. This combination of both a bony cartilaginous and a soft tissue angiomatosis is known as Maffucci’s syndrome. The clinical appearance of the multiple enchondromatosis is the same as Ollier’s disease but with a higher potential for a malignant conversion to a low grade chondrosarcoma in adult life.
- 111. CLASSIC Case #584 33 year male Maffucci’s disease
- 112. X-ray tibias
- 114. Hand x-ray
- 116. Macrosection thru large enchondroma
- 118. Case #585 36 year female with Muffucci’s syndrome
- 120. Opposite femur
- 122. hemangioma enchondroma Gross specimen
- 123. Case #586 25 year female with Muffucci’s syndrome hands
- 124. Periosteal Chondroma
- 125. Periosteal Chondroma The periosteal chondroma has the same basic pathology as the enchondroma except that it occurs on the surface of a tubular bone. It can occur as a hamartomatous process in growing patients but as with enchondroma it is usually asymptomatic and growth stops at bone maturity. The lesions are found in large bones, such as the humerus and femur, and in the small bones of the hand and foot. Radiographically one sees slight erosion into the adjacent cortex but the lesion will not penetrate into the medullary canal. There will be a sclerotic response at the base that extends around the periphery of the lesion taking on the appearance of a blister on the surface of the bone with matrix calcification seen mainly at the periphery but found also in the central area. The lesions usually stop growing before they reach the upper limit of 3-4 cm in diameter. If growth continues beyond this, one must strongly consider the possibility of a peripheral surface type chondrosarcoma
- 126. that would continue to grow after bone maturity. Periosteal sarcoma is a similar chondroid lesion found typically on large bones. It demonstrates a more aggressive pattern, permeation into surrounding cortical structures and a more aggressive histology with some osteoid formation. Osteo- chondroma also has a similar appearance but would demonstrate a more mature bony base on which a cap of cartilage is typically seen. In the case of the periosteal chondroma, the cartilage extends down into the depths of the tumor. Treatment consists of a simple resection without disturbing the subadjacent cortex so that bone grafting or internal fixation devices are not necessary. The recurrence rate is very low after maturity.
- 127. CLASSIC Case #121 17 year female periosteal chondroma distal femur
- 128. Bone scan
- 129. CT scan
- 130. Axial proton density MRI
- 131. Sagittal proton density MRI
- 132. Sagittal T-2 MRI
- 133. Photomic
- 134. Case #587 42 year male with combined periosteal chondroma and enchondroma next to each other in femur
- 135. enchondroma Bone scan periosteal chondroma
- 136. enchondroma periosteal chondroma Sagittal CT scan
- 137. Axial CT scan at level of enchondroma
- 138. periosteal chondroma enchondroma CT scan
- 139. Coronal T-1 MRI enchondroma
- 140. Axial T-1 MRI
- 141. Case #588 22 year male periosteal chondroma femur
- 142. Case #589 16 year male periosteal chondroma distal femur
- 143. AP view
- 144. Case #590 12 year female periosteal chondroma proximal femur
- 145. Frog leg lateral
- 146. Case #592 11 year female periosteal chondroma proximal tibia
- 147. Another view
- 148. CTscan
- 149. Axial proton density MRI
- 150. Photomic
- 151. Case #593 19 year female with periosteal chondroma tibia
- 152. Case #594 26 year male periosteal chondroma proximal humerus tumor
- 153. CT scan
- 154. small enchondroma Coronal T-1 MRI tumor
- 155. Photomic
- 156. Case #595 46 year female with periosteal chondroma humerus
- 157. CT scan
- 158. Another CT cut
- 159. Coronal T-1 MRI
- 160. Coronal T-2 MRI
- 161. Photomic
- 162. Case #595.1 Periosteal chondroma 17 year old female with slight pain right shoulder for 1 year
- 163. Sag T-1 T-2 Gad
- 164. Axial T-1 T-2 Gad
- 165. Case #596 14 year male periosteal chondroma proximal humerus
- 166. AP view
- 167. Case #598 62 year male with periosteal chondroma thumb
- 168. Axial T-1 MRI
- 169. Coronal proton density MRI
- 170. T-2 MRI
- 171. Photomic
- 172. Case #599 8 year female with periosteal chondroma 4th metacarpal
- 173. Case #600 25 year female with periosteal chondroma 3rd metatarsal
- 174. Case #601 26 year male with periosteal chondroma ring finger
- 175. Case #602 54 year male with periosteal chondroma 5th metatarsal
- 176. Case #603 18 year male periosteal chondroma 3rd toe
- 177. Case #604 33 year male with soft tissue chondroma finger
- 178. Lateral x-ray
- 179. Oblique view
- 180. Surgical excision
- 181. Photomic
- 182. Case #605 19 year male periosteal chondroma C-2
- 183. Bone scan
- 184. CT scan
- 185. Case #606 38 year male with periosteal chondroma ischium
- 186. Case #607 6l year female with periosteal chondroma clavicle
- 187. Osteochondroma
- 188. Osteochondroma The solitaty osteochondroma or exostosis is one of the most common benign bone tumors seen in the skeleton. As in the enchondroma, this condition is developmental, or hamartomatous in nature arising from the outer edge of the growth plate and growing down the metaphyseal side where it tends to point away from the adjacent joint. Because it originates from the growth plate, it continues to grow during the growing years of the patient and then stops at maturity. It is made up of a bony base with a pedunc- ulated stock with fatty marrow extending up inside the stock that has a cartilagenous cap giving it the appearance of a cauliflower. Histologically, the cap has features of a normal growth plate if a biopsy is performed during the growing years. Most of these lesions arise from large bones, especially about the knee joint, proximal femur, and proximal humerus. In the proximal humerus, the osteochondroma is usually sessile-based without a typical pedunc-
- 189. ulated stock and is frequently misdiagnosed for that reason. Multiple hereditary exostosis presents with multiple lesions through- out the skeletal system and is considered to be an autosomal dominant disorder, being one-tenth as common as the solitary osteochondroma which is not inherited. The conversion of a solitary osteochondoma to a chondro- sarcoma can only occur in the adult. It is an extremely rare event compared to the 1% chance of a malignant conversion in multiple hereditary exostosis. It is the cartilaginous cap that converts into a low grade secondary type of peripheral chondrosarcoma with an excellent prognosis for survival compared to a central chondro- sarcoma. These malignant conversions usually arise from large osteochondromas seen in more proximal locations, such as around the hip or pelvis. Because osteochondromata are usually without symptoms, surgical treatment is frequently unnecessary unless the lesions create mechanical problems such as around the knee joint
- 190. where larger lesions can interfere with normal ambulation. Sometimes, a large proximal lesion with a cartilage cap exceeding 2 cm should be prophylactically resected in order to avoid a possible chondrosarcoma. When removing an osteochondroma, it is necessary only to remove the complete cartilaginous cap, leaving most of the bony base intact to avoid a facture.
- 191. CLASSIC Case #122 25 year male osteochondroma tibia
- 192. Lateral view
- 193. cartilage cap fatty marrow Sagittal T-1 MRI
- 194. cartilage cap fatty marrow Macro section
- 195. Case #608 17 year male with osteochondroma humerus
- 196. marrow Axial T-1 MRI cap
- 198. cap Coronal T-2 MRI
- 199. cap Macro section
- 200. Case #609 30 year male sessile based osteochondroma humerus Coronal T-1 MRI
- 201. Coronal proton density MRI cap
- 202. cap Axial T-1 MRI
- 203. cap fatty marrow Axial T-2 MRI
- 204. Case #610 14 year male with sessile based osteochondroma humerus
- 205. Bone scan
- 206. Coronal T-1 MRI
- 207. Cut surgical specimen cap
- 209. Case #611 10 year male sessile based osteochondroma proximal humerus
- 210. Lateral view
- 211. Case #612 25 year male osteochondoma scapula
- 212. Scapular view
- 214. Case #613 32 year male with osteochondroma proximal femur
- 215. Frog leg lateral
- 216. CT scan
- 217. Case #614 12 year female osteochondroma proximal femur
- 218. Case #615 15 year male osteochondroma distal femur
- 219. cap Cut specimen in path lab
- 220. cartilage cap Photomic
- 221. Case #616 23 year male with osteochondroma distal femur
- 222. cap Cut specimen in path lab
- 224. Case #617 26 year male with osteochondroma proximal fibula
- 225. Lateral view
- 226. Case #618 18 year male with sessile based osteochondroma tibia
- 227. Case #619 11 year male sessile based osteochondroma distal tibia
- 228. Case #620 38 year male osteochondroma L-5
- 229. Lateral view
- 230. Bone scan
- 231. CT scan
- 232. cap Coronal T-2 MRI
- 233. Case #621 6 year male with osteochondroma C-6 spinous process
- 234. CT scan
- 235. Case #621 26 year male osteochondroma ilium
- 236. cap Cut specimen in path lab
- 237. Case #621.1 22 year female with painless lump right iliac crest for years
- 238. Axial T-1 Gad
- 239. Cor T-2 Sag T-2
- 240. Case #623 31 year female with osteochondroma ant 3rd rib
- 241. Case #624 16 year male subungual exostosis
- 242. AP x-ray
- 244. CLASSIC Case #625 15 year male with multiple hereditary exostoses
- 245. Tibia and fibula
- 246. Lateral view
- 247. Case #625.1 Multiple hereditary exostoses 50 yr old female with short stature and R hip pain for years
- 248. AP and lateral of right hip
- 249. AP and lat tibia
- 251. AP and lateral of femur
- 253. Case #626 13 year female multiple exostoses forearm
- 254. Distal femur
- 255. Case #627 20 year male multiple exostoses knee
- 256. Lateral view
- 257. Case #628 15 year male with multiple exostoses hips
- 258. Case #629 26 year female with multiple exostoses thorax & arms
- 259. Case #630 31 year male multiple exostoses scapula & humerus
- 260. Scapular view
- 261. CT scan
- 262. Case #631 26 year male multiple exostoses leg
- 263. Chondroblastoma
- 264. Chondroblastoma The chondroblastoma is a benign, cartilage-forming tumor seen in the metaepiphyseal area of bone in children and young adults. The histologic appearance is typical of a giant cell tumor in young adults. The chondroblastoma is one fifth as common as the giant cell tumor and the majority of cases will occur during the second decade of life. It is rare to find the giant cell tumor in patients under the age of 13 years. The most common location for the chondroblastoma is in the epiphysis of the distal femur, proximal tibia, and proximal humerus. These lesions are usually located near a joint and are quite painful because of a secondary inflamm- atory synovitis of the adjacent joint that can masquerade as a pyarthrosis. It is not unusual to find an aneurysmal bone cyst associated with the chondroblastoma, similar to the situation seen with giant cell tumors. Histologically, one sees round polyhedral- shaped stromal cells located in clear cytoplasmic halos that gives
- 265. the appearance of chicken wire under the microscope. Giant cells are frequently associated with the chondroid tissue that gives the appearance of a giant cell tumor. It is very rare for a chondro- blastoma to convert to a malignant tumor, however, as in the case of giant cell tumor, they can metastasize to the lung and still carry an excellent prognosis for survival. Treatment consists of a simple curettement of the lesion followed by packing the defect with either bone graft or bone cement. There is a relatively low (10%) recurrence rate.
- 266. CLASSIC Case #123 12 year female with chondroblastoma proximal tibia
- 267. Coronal post gad MRI
- 268. Sagittal T-2 MRI
- 269. Photomic
- 270. Case #632 26 year male with chondroblastoma prox tibia
- 271. Lateral view
- 272. Sagittal T-1 MRI
- 273. Sagittal T-2 MRI
- 274. Photomic
- 275. Case #632.1 Chondroblastoma pseudotumor (geode) 52 yr female with pain in knee for 1 yr
- 276. Cor T-1 T-2
- 277. Axial T-2 Sag T-1
- 278. Case #633 21 year female with chondroblastoma prox tibia
- 279. Case #634 16 year male with chondroblastoma distal femur
- 280. Lateral view
- 281. Coronal proton density MRI
- 282. Sagittal proton density MRI
- 283. Axial proton density MRI
- 284. Curettement of tumor from window in intercondylar notch tumor
- 285. Photomic
- 286. Higher power
- 287. Case #635 18 year male chondroblastoma distal femur
- 288. CT scan
- 289. Photomic
- 290. Case #636 20 year male with chondroblastoma & ABC prox femur
- 291. tumor Axial T-2 MRI
- 292. Coronal T-2 MRI tumor edema
- 293. Photomic
- 294. Post op x-ray with cement & DHS
- 295. Case #637 12 year female with chondroblastoma prox femoral epiphysis
- 296. CT scan
- 297. Another CT cut
- 298. cartilage giant cells Photomic
- 299. Case #638 13 year female with chondroblastoma prox fem epiphysis
- 300. Case #639 15 year male with chondroblastoma prox humerus
- 301. CT scan
- 302. Axial T-1 MRI
- 303. Coronal T-2 MRI
- 304. tumor Macro section
- 305. Photomic
- 306. Photomic with giant cells
- 307. Case #640 15 year male with chondroblastoma proximal humerus
- 308. Coronal T-1 MRI
- 309. tumor Coronal T-2 MRI
- 310. Photomic with giant cells
- 311. Another photomic
- 312. Case #641 24 year female chondroblastoma pelvis
- 313. CT scan
- 314. Another CT cut
- 315. Photomic
- 316. Case #642 CT scan 21 year male with chondroblastoma ilium
- 317. Another CT cut
- 318. tumor T-2 MRI
- 319. Case #643 43 year female with chondroblastoma distal humerus
- 320. CT scan
- 321. Case #644 11 year male with chondroblastoma lateral malleolus
- 322. Sagittal T-1 MRI
- 323. Axial T-2 MRI
- 324. Photomic
- 325. Case #645 12 year female chondroblastoma distal fibula
- 326. Case #646 18 year male with chondroblastoma talus
- 327. Lateral view
- 328. Chondromyxoid Fibroma
- 329. Chondromyxoid Fibroma Chondromyxoid fibroma is a very rare solitary benign tumor seen in bone. It occurs typically in the second or third decade of life and affects men more than women. By far the more common location for this lesion is in the proximal tibial metaphysis, followed second by the distal femur and the first ray of the foot. This lesion is slow growing and is associated with mild symptoms of pain. Radiographically, there is a lytic lesion of bone with a soap- bubbly appearance secondary to the thin sclerotic peripheral margin giving it a pseudoloculated appearance similar to that of a solitary bone cyst. The adjacent cortex is frequently thinned out and slightly dilated, similar to the pattern that is seen in fibrous dysplasia. Histologically, there will be evidence of benign fibrous tissue with large areas of myxomatous degeneration with reactive macrophage activity seen at the periphery of the lesion that could suggest the diagnosis of a chondrosarcoma.
- 330. Treatment for this lesion consists of a simple curettement and bone grafting. The fairly high recurrence rate of 25% can be reduced by a more aggressive, marginal resection of the tumor. Occasionally, this lesion can convert into a chondrosarcoma.
- 331. CLASSIC Case #124 11 year male chondromyxoid fibroma proximal tibia
- 332. Tomogram cut
- 333. Surgical exposure of tumor
- 334. Low power photomic
- 335. giant cells myxoid Higher power
- 336. Surgical curettement completed ready for bone graft
- 337. Placement of fibular strut and cancellous graft
- 338. Post op x-ray
- 339. Case # 124.1 AP and lat x-ray 50 year male with chondromyxoid fibroma proximal tibia with 6 months of a tender tumor mass anterior tibia
- 340. Coronal T-1 MRI
- 341. Coronal PD FS MRI
- 342. Axial PD FS MRI
- 343. Axial Gad MRI
- 344. Case #647 12 year female with chondromyxoid fibroma tibia
- 345. Case #648 13 year female with chondromyxoid fibroma tibia
- 346. Case #649 25 year female chondromyxoid fibroma 1st metatarsal
- 347. Oblique view
- 348. Photomic
- 349. Photomic
- 350. Case #650 7 year female chondromyxoid fibroma ulna
- 351. Photomic
- 352. Case #651 25 year female with chondromyxoid fibroma rib
- 353. Photomic
- 354. Case #651.1 60 year female with chondromyxoid fibroma distal sacrum
- 355. Sag T-1 Sag T-2
- 356. Axial T-1 Axial T-2
- 357. Coronal T-1
Notes de l'éditeur
- On this lateral radiograph of a 38-year-old female, there is a centrally located distal femoral diaphyseal lesion that was picked up an an incidental finding, The lesion is geographic and shows extensive matrix calcification with rings and arcs typically seen in benign cartilage tumors. There is minimal if any cortical erosion and no evidence of thinning or dilatation of the surrounding cortex which clearly separates it from a malignant chondrosarcoma.
- The bone isotope scan shows focalized pickup of the isotope in the area of the distal femoral metaphysis with no evidence of any inflammatory change seen in surrounding bone. A chondrosarcoma would show significant pickup in the surrounding bone reacting to the tumor infiltration.
- Coronal T1-weighted MRI image shows a typical homogeneous low signal lesion centrally located in the distal diaphysis of the femur with a lobulated sharp margination typical of a chondroid tumor with no evidence of invasion into the surrounding cortex.
- Coronal T2-weighted MRI image showing the high signal features of a water laden chondroid matrix with low signal voids speckled throughout the lesion where calcification is present. There is no evidence of any high signal infiltration into the surrounding cortical bone and no evidence of reactive edema in the surrounding marrow that would be evident in the case of a malignant chondrosarcoma.
- Axial T2-weighted MRI image reveals no evidence of cortical erosion or reactive changes in the surrounding normal tissue. There are central signal voids from matrix calcification typical for a benign enchondroma.
- In this operative photograph of the distal femur, the thin outer cortical covering has been removed to expose the tumor which demonstrates the lobulated calcific pattern of a typical enchondroma.
- Intraoperative photograph showing the surgeon using a curette to remove the cartilaginous enchondroma from the medullary canal of the femur.
- Scanning lens photomicrograph shows the geographic pattern of a benign chondroid tumor directly up against the cortex of the involved bone but without significant invasion or permeation of the chondroid matrix into the surrounding trabecular bone as would be seen in a malignant chondrosarcoma. There is complete absence of trabecular bone passing through the central geographic portion of the tumor.
- Low power photomicrograph on H&E stain shows the blue staining of the chondroid matrix with very small pyknotic nuclei scattered throughout the matrix and no evidence of duplication forms to suggest a more malignant cartilaginous tumor.
- This high power photomicrograph reveals a small pyknotic nuclei in a lacunar pattern surrounded by blue-staining chondroid matrix with no evidence of division figures as would be seen with a low-grade chondrosarcoma. However, it is extremely difficult to separate benign enchondroma from Grade I chondrosarcoma based on histology alone.
- The surgical appearance after the enchondroma has been completely curetted. The technique is similar to the technique used for a benign giant cell tumor. Following curettement either bone graft or methyl methacrylate (as was done here) can be placed into the defect.
- This operative photograph shows the appearance after packing the cavity with radiolucent bone cement.
- Lateral postoperative radiograph shows the surgical defect created by the curettage. The radiolucent cement does not image well compared to barium-impregnated methyl methacrylate. If the patient were more active, internal fixation devices would be used along with the bone graft or methyl methacrylate
- AP and lateral radiographic views of the femur of a 57-year-old female who had no symptoms of pain in the area but had an x-ray obtained for other reasons. The AP projection shows a diffuse, flocculated-type calcification filling the entire medullary canal of the femoral diaphysis with a pattern that would suggest a low-grade, benign cartilaginous lesion. There is no cortical erosion or breakthrough into the subadjacent soft tissue. However, on the lateral projection there is a fairly large, periosteal cartilaginous lesion located on the surface of the posterior cortex proximally that has the appearance of a periosteal chondroma. The concern here was that this might represent a chondrosarcoma that had eroded through the cortex posteriorly into the adjacent soft tissue. But on more careful study, it was found that there were two lesions, one being the large enchondroma of the femur and the other being a separate but associated dysplastic lesion consisting of a periosteal chondroma with no physical connection between the two lesions.
- To prove this theory, the patient was taken to the operating room and the entire posterior periosteal lesion was resected and found to be firmly attached to the posterior cortex of the femur. There was no physical evidence of any cartilaginous connection between the surface lesion and the enchondroma beneath the intact cortex. This low power photomicrograph shows the histological appearance of the periosteal chondroma with a lobulated, benign-appearing pattern with calcification in the central area and very small pyknotic nuclei.. This picture is quite diagnostic of a benign periosteal chondroma. It was assumed that the intramedullary lesion had a similar histology. The patient was observed over a period of years.
- AP radiograph taken at a later date showing no change in the appearance of the medullary lesion.
- Over a period of eight years the patient developed osteoporosis of the entire body and had pain in the right hip for which a total hip arthroplasty was performed. At that time, the medullary canal of the femur was reamed and samples of the reaming showed nothing more than benign enchondroma tissue. The patient's hip pain was relieved by the procedure. She has had no recurrence of her cartilage tumor and no conversion to a sarcoma.
- Lateral radiograph of the distal femur of a 48-year-old female who had this X-ray taken because of trauma shows a heavily calcified, flocculated matrix pattern within the medullary canal of the femur that has characteristic features of a benign enchondroma. There is no endosteal erosion and there are no periosteal changes.
- The bone isotope scan shows mild pickup in the area of the calcifying enchondroma and does not suggest the diagnosis of a chondrosarcoma. In a case like this, the patient should be watched over a period of several years to make sure that the lesion is stable without erosion of the cortical anatomy. A biopsy is not particularly helpful in predicting whether this might convert to a chondrosarcoma at some later date.
- A 59-year-old female who had this X-ray taken because of trauma. This lateral radiograph of the distal femur shows a calcific lesion located in the distal metadiaphyseal portion of the femur that was noted as an incidental finding. It has a calcific pattern characteristic for a benign enchondroma. There is no cortical erosion. This type of lesion should be observed over time to rule out the remote possibility of a low-grade chondrosarcoma. In a differential diagnosis, a bone infarct could be considered.
- This 60 year old male presented with a three month history of vague knee pain for which this x-ray was taken. As an incidental finding we see the typical arcs and rings calcific pattern of a benign enchondroma in the center of the distal femoral metaphysis.
- In this bone scan one can see a slight pick up in the area of the enchondroma with no overflow like one would see in a sarcoma.
- On this MRI study we see the typical lobulated uniform low signal pattern of a benign enchondroma on the T-1 sequence and a bright signal on the T-2 image with signal voids from calcification. The gad contrast shows only rim enhancement. Because there is no cortical contact with the tumor we can be very sure this is not a low grade chondrosarcoma and this is an asymptomatic lesion that does not require biopsy but should be watched with routine x-rays for a period of several years to rule out the remote chance of conversion to a low grade chondrosarcoma.
- On this sagittal T-1 we see the typical lobulated low signal pattern next to the bright signal pattern on the T-2 image.
- The axial T-2 shows a bright signal lesion with calcific signal voids and the Gad contrast shows the typical rim enhancement. The patellar chondromalcia seen here is the most likely cause of this patient’s dull aching knee pain.
- AP radiograph of the proximal humerus of a 62-year-old physician who had been following this benign calcific lesion in his proximal humerus for many years. Although the lesion had not changed over the years, he was concerned about the possibility of a chondrosarcoma and insisted on a conservative surgical resection. This radiograph shows the typical flocculated calcific pattern in the central portion of a benign-appearing enchondroma, with very slight dilatation of the adjacent cortical structures but no obvious erosion or breakthrough into the subperiosteal space.
- Coronal T1-weighted MRI shows the typical lobulated, low signal pattern of a benign-appearing cartilaginous lesion located centrally in the medullary canal. There is very sharp margination with the adjacent medullary fat and no evidence of any invasion into the adjacent cortical structures.
- CT scan shows the typical calcific pattern of a medullary enchondroma. Lack of permeative lytic changes in the adjacent cortical structures tends to rule out the diagnosis of chondrosarcoma.
- The patient was taken to the operating room because of his concern about possible chondrosarcoma. A slot was made in the cortex of the humerus and the entire enchondroma was aggressively curetted. No attempt was made at a wide resection for this obviously benign process. This photograph shows the gritty, cartilaginous nature of the curettement specimen.
- Scanning lens photomicrograph of the curettements shows the lobulated pattern of a benign enchondroma. There is no increased cellular activity to suggest a chondrosarcoma.
- AP radiograph of the right shoulder of a 70-year-old male who had this X-ray taken because of pain secondary to rotator cuff tendonitis. This film shows the typical matrix calcific pattern of a benign cartilaginous tumor located centrally in the canal with no direct contact to adjacent cortical structures.
- Coronal T1-weighted MRI shows the low signal characteristics of a medullary enchondroma with a few small areas of signal void secondary to calcification. There is no contact with adjacent cortical structures which tends to rule out the diagnosis of a chondrosarcoma.
- In this sagittal T-2 MRI image we can see a high signal lesion typical of chondroid tumors.
- AP radiograph of the shoulder of a 58-year-old female who presented with tendonitis symptoms shows a typical flocculated, calcific pattern in the matrix of a benign enchondroma. The lesion is quite sizable and extends out to the cortical margins but without any evidence of permeation that might indicate a chondrosarcoma. This patient was followed with observation over time to make sure this was not a low-grade chondrosarcoma.
- AP radiograph of the proximal humerus of a 42-year-old female who gave a history of low-grade symptoms of pain in the shoulder for a year-and-a-half shows a fairly large, flocculated, calcific lesion filling the entire proximal third of the humerus with no evidence of any cortical erosion. The lesion was curetted and the pathologist read this out as a questionable low-grade chondrosarcoma, however there was no further treatment. The patient was observed over a period of many years without progression of disease, thus the diagnosis was changed to benign enchondroma.
- This 47 year old male presented with a history of shoulder pain six months ago with x-ray evidence of a calcifying enchondroma in the proximal humerus as an asymptomatic incidental finding.
- On this coronal T-2 MRI image we see the bright signal lobulated pattern of the benign enchondroma which shows no evidence of cortical erosion thus ruling out the diagnosis of chondrosarcoma. The most likely cause for the shoulder pain is the bright signal ganglion cyst arising from an area of old injury to the lower edge of the glenohumeral joint capsule and labrum.
- Here we see two separate sagittal T-2 cuts; one at the humeral level showing the bright signal enchondroma with no cortical erosion; and a cut thru the ganglion cyst seen just below the glenoid labrum.
- On this two level axial T-2 MRI we see again the bright signal lobulated pattern of the enchondroma and to the right we see the bright signal ganglion cyst just below the glenoid area of the shoulder. In this case there is no need to biopsy or remove the enchondroma because it is asymptomatic and is very unlikely to convert to a chondrosarcoma in the future. The ganglion cyst is the most likely cause for the minor pain symptoms here which could be treated arthroscopically.
- AP radiograph of the tibia of a 55-year-old male who had this X-ray taken because of trauma. This film shows an asypmptomatic, slightly calcifying, medullary lesion within the upper diaphysis that is difficult to see. There is no evidence of cortical erosion.
- The patient also had a bone scan that shows mild pickup in the lesion located in the central canal of the upper tibia. There is also some arthritic pickup in both medial compartments of the knee.
- Coronal T1-weighted MRI shows a typical low signal, lobulated pattern filling the entire medullary canal of the upper tibial diaphysis. The lesion comes in close contact with the cortex in several areas and is characteristic of a benign enchondroma.
- This T2-weighted MRI shows the very bright appearance of a typical benign enchondroma with a few signal void areas in the central portion representing calcification that was seen on the radiograph. Note that there is no evidence of permeation into the adjacent cortical structures which tends to rule out the diagnosis of chondrosarcoma.
- To be on the safe side, this patient had a biopsy performed and a low power photomicrograph from the specimen shows the typical benign appearance of an enchondroma with chondroid matrix being formed by chondrocytes that have very small pyknotic nuclei. There is nothing here that would suggest the diagnosis of chondrosarcoma.
- AP radiograph of the tibia of a 55-year-old male who had this film taken because of trauma shows an asymptomatic, calcifying, cartilaginous lesion filling the entire upper half of the tibia. It is lobulated, has sharp margination and shows no evidence of cortical erosion or breakthrough into the subadjacent soft tissue.
- Lateral radiograph also shows the lobulated, calcific pattern of a benign enchondroma in the upper tibia.
- Axial T1-weighted MRI shows the low signal features of a benign enchondroma with normal fatty marrow surrounding the lesion and no evidence of cortical erosion.
- Axial T2-weighted MRI shows the high signal characteristics of a typical benign enchondroma with slight erosion into the adjacent cortex but no permeation to suggest chondrosarcoma. This patient needs to be observed over a period of time to make sure there is no progression of disease.
- Scanning lens photomicrograph from a biopsy specimen shows benign cartilaginous tissue with a geographic pattern surrounded by normal bony trabeculae. There is no evidence of permeation into the surrounding bony structure as would be seen with a chondrosarcoma.
- A 40-year-old male had this X-ray taken because of trauma. AP radiograph of the knee joint shows a flocculated, calcific pattern filling the entire upper end of the proximal fibula. Since there is no evidence of any cortical erosion, this picture is typical for a benign enchondroma.
- Technetium bone scan shows slight pickup of the isotope material in the area of the enchondroma but no evidence of overflow into the surrounding tissues, characteristic of a benign cartilaginous lesion.
- Sagittal T1-weighted MRI shows the typical lobulated pattern of a low signal lesion filling the upper end of the fibula but with normal high signal marrow surrounding the lesion which tends to rule out the diagnosis of a chondrosarcoma.
- Axial T1-weighted MRI shows again the low signal features of a benign enchondroma with normal medullary fat surrounding the lesion. There is no need to biopsy this enchondroma but it should be observed over time to make sure that it remains stable and does not progress into the surrounding bony structures.
- Oblique radiograph of the hand of a 22-year-old male who had this film taken because of injury to the hand. It shows a geographic, lytic process involving the proximal third of the ring finger. There is definite cortical thinning and bulging and faint evidence of matrix calcification, quite diagnostic of a benign enchondroma. Cortical erosion and thinning are quite typical for enchondromas of the hand or foot, but not seen in enchondromas of larger bone. It is very rare to see enchondromas in the hand or foot.
- Even though it was a totally asymptomatic, the lesion was curetted. This scanning lens photomicrograph shows the benign cartilaginous appearance of this enchondroma with a geographic erosion of the adjacent bone but no evidence of permeation into the surrounding bony structures. The nuclear pattern appears extremely benign.
- AP radiograph of the hand of a 33-year-old female who presented with trauma to the area. It shows an enchondroma involving the proximal phalanx of the middle finger with thinning of the cortex and matrix calcification in the central diaphysis of the proximal phalanx of the middle finger. At the same time, there is an adjacent cartilaginous lesion on the surface of the middle finger metacarpal with a similar calcific pattern in the matrix and erosion into the subadjacent cortex, quite diagnostic of a periosteal chondroma. There is no physical connection between the two lesions but it is obvious that this is a dysplasia similar to a low-grade Ollier's disease. The histology of the two lesions would be identical. In this case, the lesions were observed over time with no need for surgical treatment.
- Oblique radiograph again shows the benign enchondroma and the associated, but totally separate, periosteal chondroma of the metacarpal in the same ray.
- Oblique radiograph of the hand of a 29-year-old male who had an X-ray after trauma shows an asymptomatic, geographic lytic process involving the proximal third of the proximal phalanx of the thumb. There is cortical thinning and slight dilatation and a vague suggestion of calcification in the matrix of the lesion, typically seen in a benign enchondroma. There was no need for biopsy or surgical treatment.
- AP radiograph of the thumb of a 23-year-old male who had an injury to the area. There is a multi-loculated, geographic lytic lesion involving the entire mid-portion of the first metacarpal with a faint suggestion of matrix calcification and significant cortical erosion that suggests the diagnosis of a benign enchondroma. The lesion was treated by simple observation.
- A 31-year-old female presented with mild symptoms of pain in the tip of her great toe. This lateral radiograph of the great toe shows a geographic lytic process involving the entire distal half of the terminal phalanx of the great toe with a centrally located, flocculated, calcific pattern that is quite diagnostic of a benign enchondroma.
- Because her physician was concerned about the possibility of a malignant chondrosarcoma, the patient was taken to the operating room and the terminal half of her distal phalanx was amputated. This surgical specimen shows the enchondroma located in the distal portion of the phalanx.
- Photomicrograph from the surgical specimen shows the lobulated pattern of a benign enchondroma. The nuclear pattern is a bit worrisome in regards to the possibility of a chondrosarcoma but in the hand or foot it is extremely unlikely that this would be a chondrosarcoma. Even if it were, the surgical treatment is more than adequate.
- When an 11-year-old boy presented for a trauma X-ray of the foot, it was noted that he had a pre-existing, asymptomatic, geographic lytic lesion involving the proximal metadiaphyseal portion of his first metatarsal. This oblique radiograph of the foot shows distinct evidence of flocculated calcification in the central matrix of what appears to be a totally benign enchondroma. This lesion was treated by simple observation.
- Oblique radiograph of the foot of a 26-year-old male who presented with a recent injury to the area shows a geographic lesion involving the mid-portion of the fifth metatarsal. There is evidence of matrix calcification and slight thinning and bulging of the lateral cortex, quite diagnostic of a benign enchondroma. This was treated by simple observation
- Lateral radiograph of the foot of a 17-year-old teenager who had this film taken because of trauma shows a totally asymptomatic, geographic lesion in the tuberosity of the os calcis. It has a sharp, sclerotic edge to it and a faint suggestion of matrix calcification that would strongly suggest the diagnosis of a benign enchondroma.
- Os calcis view of the hindfoot shows in better detail the geographic characteristics of the benign enchondroma which lays directly benign the surface of the tuberosity. The cortex is very thinned out but there were no symptoms of pain. The lesion was observed over time.
- Tangential view of the scapula of a 28-year-old female who presented with a history of injury to the area shows a geographic lesion in the central portion of the scapular wing. There is obvious thinning and dilatation of the surrounding cortex and evidence of matrix calcification that strongly suggests the diagnosis of a benign enchondroma. It was treated by simple observation.
- AP radiograph of the pelvis and hips of a 3-year-old boy who appeared normal at birth but within the first year developed asymmetry of the body with one half being shorter than the other half. The diagnosis of Ollier's disease or multiple enchondromatosis was made based on the radiograph shown here. There are multiple geographic lesions in the supra-acetabular area as well as the proximal femoral metaphyses. In the iliac crest area, the longitudinal streaking patterns like a celery stalk or torn elephant ear are almost diagnostic of Ollier's disease.
- Radiographic views of both the upper and lower extremities show generalized epiphyseal-metaphyseal geographic changes with matrix calcification that strongly suggest the diagnosis of multiple enchondromatosis associated with slight bowing of the long bones. It is asymmetrical, being more severe on one side than the other.
- A macrosection of another case of Ollier's disease from a donor killed in an automobile accident, This surgical specimen of the proximal end of one tibia and fibula shows the dysplastic cartilaginous changes studded throughout the epiphyseal-metaphyseal portion of the upper leg.
- Low power photomicrograph of the cartilaginous tissue obtained from the enchondromata in the proximal tibial area.
- AP radiograph of the femur in a 6-year-old boy with known Ollier's disease shows multiple geographic, lytic changes in both the upper and distal end of the femur, as well as the iliac bone of the pelvis. Note the striated appearance and evidence of matrix calcification in the distal femoral area.
- This AP radiograph of the tibiae shows enchondromatosis involving the tibia on the right side. There is shortening of the extremity and a celery stalk linear, geographic lysis in the metaphyseal areas, quite typical of Ollier's disease. Note the small enchondromatous changes in the opposite proximal fibula.
- Lateral radiograph of the tibia in a 4-1/2-year-old boy with known Ollier's disease shows striated geographic osteolysis at both ends of the tibia, associated with slight shortening on this side. Note also the striated changes in the distal end of the femur above the knee joint.
- A 72-year-old female gave a history of pain in her knee area for two years and prior history of known Ollier's disease. This AP radiograph shows diffuse calcifying cartilaginous changes through the entire distal end of the femur.
- Lateral radiograph shows diffuse and generalized lytic destruction of the distal end of the femur with extensive matrix calcification, characteristic of a cartilaginous dysplasia of the femur. There are similar changes seen in the tibia below the knee joint.
- Photomicrograph from a previous biopsy of the area that proved the diagnosis of enchondromatosis. There is no evidence of conversion to malignant chondrosarcoma.
- Because of knee pain, an arthroplasty surgeon performed a routine cemented total knee replacement, however due to the weakened state of her femoral metaphyseal bone, the device loosened within one year. This radiograph shows the prosthesis in position but with loosening of the femoral component.
- The patient was taken to the operating room and the loose prosthesis was removed and replaced with a larger tumor-type total knee replacement comprised of a large distal femoral intercalary component and an 8" stem extending up to the lesser trochanteric area. Steinman pins were used to reinforce the weak tibia as is shown in this X-ray taken following the surgery.
- AP radiograph of the upper portion of the reconstruction with a long, cemented stem in position through the weakened diaphyseal portion of the upper femur. Following this procedure, the patient was able to ambulate once again.
- AP and lateral radiographic views of the knee joint of a 15-year-old male with known Ollier's disease demonstrate the striated, celery stalk appearance of Ollier's disease involving both the distal femur and proximal tibia with matrix calcification, quite diagnostic of multiple enchondromatosis.
- Close-up radiograph of the same knee shows in better detail the longitudinally oriented, striated appearance of Ollier's of the femur and tibia.
- AP X-ray of the forearm shows the typical radiographic appearance of Ollier's disease involving the distal radius and ulna.
- AP radiograph of the trunk of an 18-year-old male with proven Ollier's disease shows the characteristic striated, longitudinal, geographic lesions in both iliac crests with matrix calcification. There is also evidence of disease in the rib cage on both sides with typical chondroid matrix calcification. The spine is relatively uninvolved.
- AP radiograph of the lower extremities in a 2-year-old boy with known Ollier's disease affecting the left side more than the right. There are typical geographic lytic changes in the metaphyses of the proximal and distal ends of both the tibia and the femur with shortening on the left. The right or so-called normal side exhibits only minor changes.
- AP radiograph of the proximal humerus of a 26-year-old male with known Ollier's disease shows extensive, geographic, lytic changes involving the entire upper third of the humerus. There is cortical thinning and dilatation and a multi-loculated appearance with slight matrix calcification, quite typical of enchondromatosis.
- Oblique radiograph of the hand on the same side that shows extensive involvement of Ollier's disease of the index finger. There are also minor changes seen in the thumb and middle finger.
- AP radiograph of the hand again shows the changes of multiple enchondromatosis involving all the bones of the index finger, along with minor changes seen in the middle finger and thumb. This patient was followed for many years with concern that perhaps one of the larger lesions in the shoulder might convert to a chondrosarcoma, but so far it has not occurred.
- AP radiograph of the femur of a 19-year-old male with shortening of his left lower extremity shows extensive, geograhic lytic changes throughout the entire femur.and also some involvement in the ischium of the pelvis above. There is diffuse matrix calcification seen in this extensive cartilage dysplasia.
- Oblique radiograph of the hand of a 22-year-old male with known Ollier's disease shows extensive, geographic, lytic lesions in nearly every bone of the hand. There is extensive chronic thinning and dilatation of the cortical anatomy of the phalanges and evidence of diffuse matrix calcification, quite typical of severe multiple enchondromatosis. The distal radius is also involved.
- Because of the severe deformity and disability of the involved hand (the patient had essentially no function) and because of concern of possible conversion to a chondrosarcoma, the entire hand was amputated. This macrosection of a surgical specimen shows extensive cartilaginous replacement of the bony anatomy of the metacarpals and phalanges.
- This close-up of the base of the index finger metacarpal shows dysplastic cartilage extending up to and attached to area of the proximal growth plate. There is no microscopic evidence of chondrosarcoma.
- AP radiograph of the hand of a 40-year-old female with known Ollier's disease that shows extensive, geographic, lytic changes in virtually every bone of the hand. There are large dilated areas that have an aneurysmal appearance and matrix calcification, quite diagnostic of enchondromatosis.
- Radiograph of the hand of a 10-year-old male with known Ollier's disease involving most of the bones of the index and middle finger. This film demonstrates both enchondromas and juxta-cortical chondromas as well.
- AP radiograph of the hand of a 30-year-old female with known Ollier's disease involving the entire middle ray of the hand with cortical thinning and dilatation of bone and geographic lytic changes with matrix calcification, quite typical for enchondromatosis.
- AP radiograph of the hand of a 3-year-old boy born with mild deformity of hand shows multiple geographic, lytic changes involving the middle, ring and little finger phalanges. There is chronic cortical thinning and dilatation, as well as matrix calcification, quite diagnostic of multiple enchondromatosis.
- AP radiograph of the feet of a 19-year-old male with Ollier's disease shows bilateral asymmetrical involvement of the phalanges of both feet, being more severe on the right side than on the left. No treatment was necessary for this relatively mild deformity.
- Photograph of the hand of a 5-year-old girl with Ollier's disease being prepared for surgical reconstruction in the operating room. Note the severe deformity of all the fingers with lumpy subcutaneous nodularities, typical for a severe form of Ollier's disease.
- Radiograph of the hands with radiographic changes typical for Ollier's disease involving mostly the phalanges. There are a large number of surface juxta-cortical, periosteal chondromas as well.
- Photograph following completion of the hand reconstruction showing the similar deformity of the feet. The condition is more severe on the left side than the right. There is also deformity of the knee secondary to extensive involvement of the distal femur, typical of Ollier's disease.
- Close-up of the deformed foot and ankle on the left side.
- AP radiograph of the femur of a 33-year-old male with shortening of the left lower extremity and varus deformity. The varus deformity is caused by cartilaginous replacement of the distal meta-epiphyseal portion of the distal femur secondary to Ollier's disease. In this case, the patient has associated soft tissue hemangiomatosis and thus the diagnosis of Maffucci's syndrome was made.
- AP and lateral radiographic views of the leg of the same patient shows extensive enchondromatosis of the upper and lower end of the tibia associated with bony deformity.
- This AP radiograph of the forearm shows extensive changes secondary to multiple enchondromatosis with shortening of the ulna and a dislocation of the proximal radial head. In the soft tissue overlying the wrist area there are phleboliths with punctate calcification, quite diagnostic of hemangiomatosis associated with enchondromatosis thus making the diagnosis of Maffucci's syndrome.
- AP radiograph of the hand of the same patient showing extensive enchondromatosis of all the phalanges of the hand. There is extensive involvement of soft tissue hemangiomatosis with phlebolith formation.
- Because of the extensive deformity and pain associated with the weakened bones in the hand, the patient elected to have an amputation. This pathological specimen from the amputation shows typical diffuse cartilaginous dysplasia of the bones and overlying the distal end of one of the metacarpals, there is a fairly large hemorrhagic hemangioma on top of the Ollier's disease.
- Macrosection obtained from the amputated specimen shows diffuse enchondromatosis displacing almost the entire proximal phalanx of the index ray.
- Because of concern about possible secondary chondrosarcoma, the pathologist looked for this but found only benign-appearing enchondromatosis in all of the phalanges. The instance of secondary chondrosarcoma in Maffucci's syndrome is much higher than in Ollier's disease -- approximately 50-70% of cases.
- AP radiograph of the femur of a 36-year-old female shows multiple enchondromatosis involving the entire femur. There is phlebolith formation In the overlying soft tissues, making the diagnosis of hemangiomatosis that when combined with enchondromatosis confirms the diagnosis of Maffucci's syndrome.
- Oblique view of the same femur with evidence of soft tissue hemangiomas and calcifying enchondromas in the femoral shaft.
- AP radiograph of the opposite femur shows the enchondromas of the femur with sharply defined, calcific phleboliths in the overlying soft tissue.
- On this lateral radiograph of the femur there is extensive evidence of hemangiomatosis in the muscles of the posterior compartment of the thigh.
- Gross specimen of another patient with Maffucci's syndrome who was treated with surgical resection of a large bone that shows enchondromatosis of the bone. A hemangioma can be seen in the adjacent soft tissue overlying the bone.
- AP radiograph of the hands of a 25-year-old female with known Maffucci's syndrome shows generalized multiple enchondromatosis, along with a few areas of phlebolith formation in the adjacent soft tissue.
- Lateral radiograph of the distal femur of a 17-year-old girl who felt an asymptomatic, firm lump in her popliteal space but had no disability. The radiograph revealed a 3 cm periosteal lesion on the back side of the distal femoral metaphysis with a sclerotic base and shell of reactive bone and calcification extending over the top of the lesion taking on the appearance of a large blister on the back side of the femur. There is evidence of matrix calcification in the central portion of the lesion suggesting a low-grade chondroid tumor.
- On this bone scan, there is pickup of the isotope in the exact location of the lesion with no overflow hyperemia or reactive changes seen in the surrounding bone to suggest a malignant process.
- CT scan shows the sclerotic bony base of the cartilaginous lesion with a totally intact posterior cortex which definitely rules out the diagnosis of an osteochondroma and goes against the diagnosis of a periosteal sarcoma. There is matrix calcification in the chondroid portion of the tumor that bulges into the popliteal space.
- On this axial proton density MRI, note the high signal features of the chondroid tissue located on top of the sclerotic bony base with reactive bone attempting to surround the cartilaginous portion of the tumor.
- Sagittal proton density MRI that shows the periosteal chondroma bulging into the popliteal space.
- Sagittal T2-weighted MRI clearly showing the high signal feature of the chondroid portion of the tumor, demonstrating the reactive sclerotic base with no evidence of permeation of the cartilage into the surrounding bone which tends to rule out malignant chondroid tumors. And it certainly does not represent an osteochondroma which typically has a bony base.
- This low power photomicrograph shows a fairly cellular chondroid tumor but without evidence of division figures. The nuclei are fairly pyknotic, similar in appearance to what is seen in a benign enchondroma, This lesion was treated by a simple marginal resection without sacrificing the cortical base and thus no internal fixation was indicated. The chance of recurrence is extremely low.
- AP radiograph of the femur of a 42-year-old male who had no symptoms of any type in his thigh area shows a small, calcifying surface lesion located on the posterior cortex of the femoral diaphysis. Located in the medullary canal just above this lesion, there is a calcifying enchondroma that is not in contact with the surface periosteal chondroma. Because there is no continuity between the two lesions, the diagnosis of chondrosarcoma is ruled out.
- Technetium bone scan shows increased uptake in the area of the medullary enchondroma, and then a smaller lesion on the surface distal to the enchondroma indicates uptake by the periosteal chondroma.
- Sagittal CT scan shows the calcific nature of the enchondroma in the medullary canal, as well as the calcifying surface periosteal chondroma distal to it. There is no evidence of connection between these two lesions.
- Axial CT scan at the level of the enchondroma shows the calcifying nature of the enchondroma in the medullary canal, surrounded by normal medullary fat.
- Axial CT scan at the level of the periosteal chondroma shows the calcification arising from the posterior surface of the femoral diaphysis.
- Coronal T1-weighted MRI at the level of the enchondroma shows the characteristic lobulated low signal features of the benign enchondroma surrounded by high signal fatty marrow.
- Axial T1-weighted MRI at the level of the enchondroma shows the low signal lobulated pattern of the enchondroma surrounded by normal fatty marrow. These are two dysplastic lesions located in the femur that have very little potential to progress to a chondrosarcoma but should be observed over years with routine radiographic studies.
- AP radiograph of the femur of a 22-year-old male who presented with a symptomatic lesion on the surface of the femur which had a calcific shell at the periphery and very little evidence of cortical erosion below. On biopsy it proved to be a periosteal chondroma that was simply excised during the biopsy procedure. There is concern about periosteal chondrosarcoma when these chondroid lesions are larger than 5 cm across.
- Lateral radiograph of the knee of a 16-year-old male shows a totally asymptomatic, calcifying surface lesion on the posterior aspect of the distal femoral diaphysis. The calcification is located mostly on the surface of the lesion, similar to a blister on the surface of bone, with no evidence of cortical erosion. On excisional biopsy, this lesion proved to be a periosteal chondroma.
- AP radiograph shows the surface periosteal chondroma on the medial cortex of the supracondylar area of the distal femur. There is a shell of calcification at the periphery and a slight cortical erosion at the base, characteristic of a periosteal chondroma.
- AP radiograph of the proximal femur of a 12-year-old female shows an asymptomatic, calcifying mass arising from the medial surface of the base of the femoral neck just above the lesser trochanter. It has a calcific pattern that would suggest a cartilaginous tumor and on excisional biopsy it turned out to be a periosteal chondroma.
- Here we see the lesion protruding in an anterior direction on this frog leg lateral.
- AP radiograph of an 11-year-old girl shows a slight cortical irregularity in the proximal tibial diaphyseal area that has a streaking pattern, suggesting the diagnosis of a cartilaginous tumor. This lesion proved to be a periosteal chondroma, perhaps better diagnosed as an intracortical chondroma.
- An oblique radiographic view of the proximal tibia showing the cortical erosions from the cartilaginous tumor.
- CT scan through the level of the periosteal chondroma showing the geographic lesion located in the posteromedial cortex of the upper tibial diaphysis. There is calcification within the chondroid matrix and moderate erosion into the surrounding cortical structures, more like an intracortical chondroma.
- Axial proton density MRI shows the low signal, dense, reactive bone at the base of the periosteal chondroma. The higher signal on the surface represents the cartilaginous matrix with signal voids secondary to calcification.
- The patient was taken to the operating room and had an excisional curettement biopsy of the lesion. This photomicrograph shows cartilaginous matrix with calcification being produced by benign chondrocytes, similar to the appearance of an enchondroma. In the differential diagnosis, periosteal sarcoma must be considered. It has a similar clinical appearance but is far more aggressive microscopically.
- AP radiograph of the knee of a 19-year-old male shows a benign-appearing, totally asymptomatic, surface cartilaginous lesion arising from the medial cortex of the proximal tibial metaphysis. There is evidence of matrix calcification, a peripheral shell of calcification and a cortical erosive base, quite diagnostic of a periosteal chondroma. This lesion was treated by an excisional biopsy and indeed turned out to be a cartilaginous lesion.
- A 26-year-old male presented with symptoms of a firm, asymptomatic lump high in the axillary area attached to his upper humerus. This AP radiograph of the shoulder shows a soft tissue, calcifying lesion attached to the upper medial cortex of the humerus, measuring about 3 cm in diameter. There is calcification at the periphery of the lesion and very slight cortical erosion, characteristic of a benign periosteal chondroma.
- CT scan through the upper humerus shows a 3 cm surface lesion on the medial cortex of the humerus with slight erosion into the bone and evidence of surface matrix calcification, characteristic of a benign periosteal chondroma.
- Coronal T1-weighted MRI shows the low signal characteristics of the periosteal chondroma attached to the medial cortex of the upper humerus with a small and related enchondroma measuring about 8 mm in diameter located in the humeral head. This picture suggests a benign dysplastic process rather than a malignant chondrosarcoma.
- The patient was taken to the operating room and an excisional biopsy of the entire surface lesion was carried out. Here is microscopic evidence of a benign chondroid tumor with features similar to an enchondroma.
- A 46-year-old female noted a palpable lump on the outer aspect of her shoulder. This AP radiograph of the shoulder shows a surface lesion arising from the area of the bicipital groove with calcification extending out into the soft tissue, characteristic of a periosteal chondroma.
- CT scan through the level of the lesion that is arising from the anterior surface of the humeral neck. There is matrix calcification in the adjacent soft tissue and a slightly sclerotic base where it is attached to the upper humerus.
- Another cut through the base of the lesion with changes seen in the lateral ridge to the bicipital groove that represents the base of the periosteal chondroma.
- Coronal T1-weighted MRI shows the low signal features of the surface lesion arising from the anterior cortex of the proximal humeral metaphysis where it is attached to the bicipital groove.
- Coronal T2-weighted MRI shows the high signal characteristics of the periosteal chondroma attached to the area of the bicipital groove of the upper humerus.
- The patient was taken to the operating room and an excisional biopsy was carried out, removing the entire periosteal chondroma. This photomicrograph shows a benign chondroid tumor, similar to an enchondroma.
- This 17 year old female gave a one year history of slight pain in the right shoulder which on this x-ray reveals a sclerotic lesion arising from the medial cortex of the proximal humoral metaphysis.
- This sagittal MRI study shows the lesion to be arising from the medial cortex of the upper humoral metaphysis and is low signal on T-1, bright on T-2 and shows rim enhancement on gad contrast suggesting the diagnosis of a periosteal chondroma.
- The same thing is seen on the axial images. This lesion was surgically curetted and the histology proved the diagnosis of a periosteal chondroma.
- A 14-year-old boy presented with a painless lump in the proximal arm. This AP radiograph of the upper humerus shows a geographic lysis eroding into the lateral surface of the proximal humeral metaphysis with a smoky, bulgy, soft tissue lesion extending out under the deltoid muscle shield. It has a sclerotic, reactive base characteristic of a benign chondroid tumor. This lesion was treated by an excisional curettement biopsy and histologically proved to be a benign periosteal chondroma.
- AP x-ray of the same lesion.
- A 62-year-old male presented with physical evidence of a painless, firm, non-tender lump in his first web space attached to the thumb. This oblique radiograph of the hand shows a surface lesion arising from the ulnar cortex of the first metacarpal with slight cortical erosion at its base and a calcific shell at the periphery of the dilated portion of the lesion that on excisional biopsy proved to be a benign periosteal chondroma
- Axial T1-weighted MRI through the level of the tumor shows the low signal, lobulated pattern of a benign periosteal chondroma filling the web space between the first and second metatarsal bones and bulging dorsally beneath the skin where the tumor could be palpated.
- Coronal proton density MRI shows the higher signal characteristics of the periosteal chondroma. There are signal voids secondary to calcification within the musculature of the first web space.
- T2-weighted MRI shows the high signal lobulated pattern of the periosteal chondroma in the first web space between the thumb and index finger.
- This patient was taken to the operating room and excisional biopsy of the periosteal chondroma was carried out through a dorsal incision. Here is microscopic evidence of benign chondroid tissue, similar to that of a benign enchondroma.
- An 8-year-old girl presented with a firm, asymptomatic nodule on the dorsum of her fourth metacarpal. This radiograph of the hand shows a calcifying surface lesion arising from the dorsal and ulnar aspect of the fourth metacarpal with slight erosion into the subadjacent cortical bone that has the appearance of a periosteal chondroma. It was treated by an excisional biopsy and proved to be a benign chondroid tumor.
- AP radiograph of the foot of a 25-year-old female who presented with an asymptomatic lump on the dorsal aspect of the third metatarsal shows a calcifying circumferential surface lesion arising from the distal half of the third metatarsal with very slight cortical erosion. On excisional biopsy, this proved to be a periosteal chondroma.
- A 26-year-old male presented with an asymptomatic, firm lump beneath the skin of his ring finger. This oblique radiograph of the finger shows a calcifying surface lesion with lobulated calcific pattern creating slight cortical erosions in the distal portion of the proximal phalanx of the ring finger. It was treated by an excisional biopsy and proved to be a periosteal chondroma.
- A 54-year-old male presented with a non-tender lump over the dorsal aspect of his distal fifth metatarsal. This oblique radiograph of the foot shows a surface lesion arising from the dorsal cortex of the distal fifth metatarsal with calcification in the matrix that suggests the diagnosis of a periosteal chondroma versus the possible diagnosis of a synovial sarcoma which can also calcify in soft tissue in the foot. This lesion was treated by an excisional biopsy and histologically proved to be a benign periosteal chondroma.
- AP radiograph of the foot of an 18-year-old male who presented with a non-tender lump in the second web space between the second and third toes shows a surface lesion arising from the medial aspect of the proximal phalanx of the third toe. There is a soft tissue mass bulging into the second web space and smoky calcification within the lesion suggesting the diagnosis of a periosteal chondroma. The lesion was treated by an excisional biopsy and turned out to be a benign chondroid tumor. The differential diagnosis of a synovial sarcoma could be considered in this case.
- Photograph of the hand of a 33-year-old male who gave a history of an asymptomatic, firm, subcutaneous nodular lump at the base of his ring finger that had been present for many years without progressive growth.
- Lateral radiograph of the hand shows the calcifying pattern of a benign, soft tissue cartilaginous tumor. It is similar to a periosteal chondroma but is not attached to the subadjacent bone. The calcification is amplified at the periphery of the lesion, suggesting a benign diagnosis rather than a malignant soft tissue osteosarcoma.
- Oblique radiograph of the hand again shows the calcifying chondroid tumor with condensation of calcification at the periphery and radiolucency in the central area of the benign chondroma.
- The patient was taken to the operating room and this photograph shows the soft tissue chondroma being excised from the surrounding soft tissue. Note the characteristic lobulated pattern of a benign chondroma.
- Photomicrograph taken from the surgical specimen shows the classic appearance of a benign chondroma, similar to what would be seen with a benign enchondroma.
- Lateral radiograph of the cervical spine of a 19-year-old male who presented with mild symptoms of neck pain shows a calcifying surface lesion between the posterior elements of C1 and C2 that seems to be attached to the posterolateral body of C2. This picture suggests the diagnosis of a surface periosteal chondroma.
- Technetium scan shows pickup of the isotope in the area of the lesion at the C2 level.
- CT scan through the body of C2 with calcification arising mostly from the outer surface of the condylar portion of C2. Some of the tumor has extruded into the floor of the vertebral canal but did not cause cord compression. This lesion was treated by an excisional biopsy and proved to be a benign periosteal chondroma.
- A 38-year-old male presented with a slight, non-tender lump over his ischial tuberosity. This AP radiograph of the lower portion of the pelvis shows a calcifying surface lesion with minimal cortical erosion at the base that on excisional biopsy proved to be a periosteal chondroma.
- A 61-year-old female noted a lump at the mid-portion of her collarbone. This laminagram radiographic cut through the clavicle shows a calcifying surface lesion arising from the infraclavicular portion of her mid-shaft clavicle that on excisional biopsy proved to be a benign periosteal chondroma.
- On this AP radiograph of a 25-year-old male, there is an exophytic mass arising from the posterior aspect of the proximal tibia with a pedunculated cauliflower appearance quite typical for a solitary osteochondroma.
- Lateral radiograph shows an exophytic pedunculated cauliflower mass arising from the posterior cortex of the proximal tibia with a small cartilaginous cap extending into the posterior compartment.
- Sagittal T1-weighted MRI image shows the high signal features of fatty marrow extending from the medullary canal of the tibia up into the bony stock of the pedunculated osteochondroma. At the posterior tip there is a 1x2 cm low signal cartilaginous cap that gives the clinician the exact ratio of cartilage to bone, which in this case is favorable and not likely to convert into a chondrosarcoma. When lesions get up over 2 cm in thickness there is concern about the possibility of a chondrosarcoma.
- Gross macrosection shows the resected specimen with an osteoporotic fatty bony base arising from the posterior cortex of the tibia. At the very top of the lesion, note the small cartilaginous cap that is sharply defined from the exophytic bony base, In this case, the tumor was resected because irritation of the muscles in the posterior compartment of the leg made walking painful. There was no concern about the possibility of a secondary chondrosarcoma.
- A 17-year-old male presented with an obvious, asymptomatic bony lump in his left shoulder that had been present for ten years. This AP radiograph of the shoulder shows a heavily calcified lesion arising from the proximal humeral metaphysis with evidence of chronic dilatation of the bone at the base of the lesion.
- Axial T1-weighted MRI showing the high signal fat extending up into the base of the lesion, diagnostic of an osteochondroma, with multiple lobulated, cartilaginous caps in the periphery beneath the surrounding muscle of the upper arm.
- Sagittal T1-weighted MRI again shows the enlarged fatty marrow space dilating the upper humerus and extending out into the base of the osteochondroma. There are multiple areas of fatty marrow in the central portion of the cap of the osteochondroma with low signal cartilaginous areas seen on the surface of the lesion.
- T2-weighted MRI cut through the epicenter of the osteochondroma shows the low signal central portion of the cartilaginous lesion which is heavily calcified. The bright signal at the periphery represents the uncalcified cartilaginous portion of the multi-loculated, cauliflower-appearing periphery of the osteochondroma.
- The patient was taken to the operating room and the osteochondroma was resected. This photomicrograph of the surgical specimen shows that most of the lesion represents osteoporotic cancellous bone (left) with a small cap of heavily calcified cartilage (right). Because of the low cartilage volume, the chance of this lesion converting to a chondrosarcoma is extremely low.
- Sagittal T1-weighted MRI of the proximal humerus of a 30-year-old male shows a large surface lesion arising from the mid-diaphysis of the humerus. It has an elongated, sessile base where there is fatty marrow extending up into the bony center of the osteochondroma (diagnostic of this condition), with small, low signal cartilaginous caps on the surface beneath the muscle.
- Coronal proton density MRI shows again the high signal fatty marrow extending up into the base of the osteochondroma with an intermediate signal cartilaginous cap, measuring about 1 cm in thickness, at the top of the bulging osteochondroma beneath the adjacent muscle tissue.
- Axial T1-weighted MRI shows the large amount of fatty marrow extending out into the central portion of the peripheral osteochondroma with low signal cartilaginous caps measuring about 1-1/2 cm in thickness on the surface of the lesion.
- This axial T2-weighted MRI shows the low signal features of the fatty marrow extending up into the pedunculated osteochondroma with a very bright 1 cm cartilaginous cap laying on the surface of the osteochondroma. For mainly cosmetic reasons, the lesion was surgically excised without difficulty.
- A 14-year-old boy gave a history of a firm, bony, asymptomatic lump in the upper portion of his right arm that had been present for ten years. This AP radiograph of his humerus shows a sessile-based expansile lesion arising from the upper cortex of the humerus. There is thinning of the cortex and bulging of the fatty marrow out into the base of the sessile originating osteochondroma with a very small cartilaginous cap.
- Technetium bone scan shows very little uptake in the area of the osteochondroma because of the very low metabolic activity seen within a dysplastic osteochondroma. This tends to rule out a periosteal sarcoma that might have similar appearance.
- Coronal T1-weighted MRI shows the low signal fatty tissue extending out into the base of the osteochondroma over a large area. This is quite different in appearance from the pedunculated osteochondromas with the narrow stalk at the base. At the outer periphery there is a very small, low signal, cartilaginous cap on top of the exostosis.
- The patient was taken to the operating room and a conservative resection of the osteochondroma was carried out, A small portion of the sessile base was removed that is quite elongated. Most of the specimen is fatty cancellous bone extending up into the cap of the exostosis with a very small (8 mm) thick cartilaginous cap arising from the surface. This lesion has a very low potential for conversion to chondrosarcoma.
- Photomicrograph taken from the surgical specimen shows the benign-appearing cartilaginous cap on top of the bony base of the exostosis. The histological pattern is quite similar to what would be seen in a normal growth plate at the end of a long bone.
- A 10-year-old boy presented with an asymptomatic lump on the upper portion of his right arm of several years duration. This AP radiograph of the proximal humerus shows a sessile-based osteochondroma arising from the inner cortex of the upper humerus with a very small cartilaginous cap on the surface. The lesion was treated by simple observation.
- This lateral radiograph again shows the dilated appearance of this sessile-based osteochondroma that in this view takes on the appearance of a parosteal osteosarcoma.
- A 25-year-old male presented with symptoms of a grating sensation under his shoulder blade on the left side with elevation activity. This tangential radiographic view of the scapula shows an osteochondroma arising from the underside of the scapular blade. It is causing pressure erosion into the subadjacent ribcage.
- Another tangential view showing the pendunculated osteochondroma arising from the underside of the scapular blade, rubbing against the ribcage beneath.
- The patient was taken to the operating room and the solitary osteochondroma was resected from the underside of the scapula. This photograph shows the osteochondroma with the cartilaginous cap at the top of the lesion
- A 32-year-old male presented with an obvious, tender lump arising from the upper end of his femur that caused pain with flexion-extension activity. This AP radiograph of the proximal femur shows an exophytic mass arising from the intertrochanteric portion of his proximal femur with a calcifying cartilaginous cap that strongly suggests the diagnosis of a solitary osteochondroma.
- Lateral radiograph of the upper femur shows the solitary lesion arising from the lesser trochanter, which is a common location for these lesions in the upper femur, with a heavily calcified cartilaginous cap that created mechanical problems with motion at the hip joint. A lesion of this size might be of concern for possible conversion to a chondrosarcoma at a later date. This happens in about 0.5% of cases.
- CT scan through the epicenter of the tumor shows the lobulated osteochondroma arising from the lesser trochanter and bulging posteriorly. This makes the lesion more accessible by means of a posterior approach with the leg in a position of internal rotation. This lesion was resected surgically because of mechanical problems. The patient did well with total relief of his previous disability.
- A 12-year-old girl presented with a slightly painful lump on the inner aspect of her proximal thigh that caused problems with rotatory motion of the hip. This AP radiograph of the hip joint shows a cauliflower-appearing, calcific exostosis arising from the lesser trochanter and bulging into the adductor compartment of the proximal thigh. This lesion was treated by a partial resection to relieve the mechanical problems related to the exostosis.
- AP radiograph of the distal femur of a 15-year-old boy shows a solitary osteochondroma arising from the medial aspect of the distal femoral metaphysis with a small pedunculated base and a small cauliflower peripheral lesion with a relatively small cartilaginous cap.
- Because of discomfort in the knee area, this patient elected to have this lesion removed. The surgical specimen cut in the pathology lab shows the central, fatty marrow portion of the exostosis lined on the surface by a thin cartilaginous cap. It has very little potential of converting to a chondrosarcoma.
- Photomicrograph through the exostosis with a benign-appearing cartilaginous cap sitting on top of cancellous bone filled with fatty marrow.
- A 23-year-old male presented with a slightly tender, bony mass beneath the quadriceps muscle just above the knee cap. This lateral radiograph of the distal femur shows the typical, calcifying, cartilaginous cap laying on top of a small pendunculated base that is quite diagnostic for a solitary osteochondroma
- The patient was taken to the operating room and the solitary osteochondroma was resected conservatively at its base. The lesion was cut with a band saw in the pathology lab and shows the bony base of the lesion and a multi-lobulated cartilaginous cap at the periphery that gives it the appearance of a cauliflower.
- This scanning lens photomicrograph through the cap of the lesion shows the benign cartilaginous tissue arising from the cancellous fatty marrow base, typical of an osteochondroma.
- AP radiograph of the knee joint of a 26-year-old male who presented with a bony lump over the posterior aspect of his knee shows a calcifying lesion arising from the proximal end of the fibula that could suggest the diagnosis of a malignant bone tumor.
- Oblique radiograph showing the proximal fibular head in relief. There is an obvious dilated, exophytic lesion arising from the upper fibular metaphysis with a lobulated outer cap lined with a thin portion of cartilage that could be misconstrued as an aneurysmal bone cyst. This lesion was treated by a simple surgical resection, being careful not to damage the adjacent peroneal nerve.
- AP radiograph of the distal tibia of an 18-year-old male shows a chronic deformation of the distal tibial metaphysis with dilatation out against the adjacent fibular causing chronic erosive changes in the fibula and suggesting a longstanding relationship that was causing minimal, if any, disability to the patient. In most cases, these sessile-based osteochondromata are best left alone.
- AP radiograph of an 11-year-old girl shows a sessile-based osteochondroma arising from the distal tibial metaphysis. It bulges out and into the substance of the distal fibula and appears to have been present for many years, causing the patient no disability. It is best treated with simple observation.
- A 38-year-old male gave a history of a firm but non-tender mass in the flank area that had been present for many years. This AP radiograph of the lumbosacral spine shows a cauliflower-shaped exophytic mass arising from the lower portion of the lumbar spine, bulging out into the paraspinous musculature.
- Lateral radiograph shows again shows the multilobulated osteochondroma bulging laterally from the lower lumbar spine into the paraspinous gutter.
- Technetium bone scan shows slight pickup in the area of the benign-appearing osteochondroma at the L5 level.
- CT scan cut across the L5 level shows a large, pedunculated, exophytic mass arising from the posterolateral elements of L5. The mass is bulging into the paraspinous musculature peripherally.
- Coronal T2-weighted MRI shows the high signal fatty marrow extending up into the base of the osteochondroma with a few, small, low signal cartilaginous caps seen at the periphery. None of the caps is larger than 1 cm in girth suggesting a benign process without associated chondrosarsoma. Because of the large, bulky nature of the lesion, the patient elected to have this lesion debulked surgically just to make sure that it would not convert into a chondrosarcoma at a later date.
- On this lateral radiograph of the cervical spine of a 6-year-old boy there is an asymptomatic exophytic mass arising from the tip of the spinous process at the C6 level. It was originally thought to be an aneurysmal bone cyst but on surgical excision proved to be an osteochondroma.
- CT scan through the same lesion shows the typical pedunculated appearance of an osteochondroma with fatty marrow extending up into the base of the lesion and a small cartilaginous cap.
- On this lateral radiograph of the cervical spine of a 6-year-old boy there is an asymptomatic exophytic mass arising from the tip of the spinous process at the C6 level. It was originally thought to be an aneurysmal bone cyst but on surgical excision proved to be an osteochondroma.
- CT scan through the same lesion shows the typical pedunculated appearance of an osteochondroma with fatty marrow extending up into the base of the lesion and a small cartilaginous cap.
- This 22 year old female presented with a long history of a painless lump over her right iliac crest. This x-ray shows the typical appearance of a benign osteochondroma protruding from the anterior portion of the iliac crest.
- On these axial MRI images one can see the high dignal fatty marrow extending into the main body of the osteochondroma in the T-1 image to the left.
- When looking for the thickness of the cartilage cap, these T-2 images point out the high signal cartilage which only becomes worrisome when it is over three cm. In girth to suggest a possible secondary peripheral chondrosarcoma.
- A 31-year-old female presented with a bony lump arising from her ribcage posteriorly on the right side. This radiograph of the ribcage shows an exophytic, heavily calcified, lobulated mass arising from the posterior aspect of one of the ribs on the right side. The mass was bulging into the thoracic cavity and the clinicians were concerned about the possiblity of a chondrosarcoma. For that reason, the lesion and the adjacent rib were totally excised. It proved to be a solitary osteochondroma and not a chondrosarcoma.
- A 16-year-old male presented with painful symptoms in his great toenail bed. On physical examination there was a bulging mass arising from the nail bed causing deformation of the adjacent nail secondary to a small exostosis arising from the distal phalanx.
- This radiograph shows the exostosis arising from the distal phalanx. It was treated surgically by a simple excision to relieve pressure symptoms.
- AP radiograph of the pelvis of a 15-year-old male who came from a family with autosomal-dominant multiple hereditary exostosis shows evidence of chronic, dysplastic dilatation of both proximal femoral metaphyses with small surface lobulated lesions, characteristic of multiple hereditary exostosis.
- AP radiograph at the knee level in the same patient showing multiple exostoses arising from the upper metaphyseal areas of both tibiae.
- Lateral radiograph of the knee shows the typical dilated metaphyses of both the distal femur and the proximal tibia with small exophytic nodularities at the surface of the cortical anatomy. This patient had no physical disability related to his problem and did not require surgical treatment.
- This 50 year old female presented with a family history of multiple hereditary exostoses with associated short stature because of a universal growth plate abnormality that has resulted in marked widening of the proximal femoral metaphyses as seen on this AP x-ray of the pelvis and hips. One can see a fairly large osteochondroma arising from the right greater trochanter that limits rotatory and abduction motion and is the cause of mild pain symptoms. The hip point cartilage is well preserved with no signs of osteoarthritis and far from being a candidate for a total hip replacement.
- On this AP and lateral of the right hip one can see in better detail the widening the the proximal femoral metaphysis with multiple exophytic protrusions located around the entire proximal femur with largest one located on the greater trochanter. It would be very difficult for a surgeon to remove these masses without serious loss of function.
- Here we see the metaphyseal abnormalities at both ends of the tibia and fibula with the typical valgus deformity at the ankle second to shortening of the fibula.
- Here we see the x-rays of both humeri with exophytic spurs arising from the widened proximal humeral metaphyses which are short in stature.
- Here we see the defects in the femur which are also short in stature with spurs seen arising from the distal femoral metaphyses.
- Here we see the abnormalities about the foot and ankle in multiple hereditary exostoses.
- AP radiograph of the forearm of a 13-year-old girl who parents had multiple hereditary exostoses. This film demonstrates the typical dysplastic shortening of the distal ulna, causing slight bowing deformity of the distal radius, characteristic of multiple hereditary exostosis.
- AP radiograph of the same patient showing dilated distal metaphyseal cortices in the femur with several small exophytic spurs pointing proximally.
- AP radiograph of the knee of a 20-year-old male with multiple hereditary exostoses. There are dilated cortices in both the distal femur and the proximal tibia and small exostoses pointing away from the knee in both the distal femur and proximal tibia.
- Lateral radiograph again showing the dilated metaphyseal cortices, both above and below the knee.
- AP radiograph of the pelvis of a 15-year-old boy shows dysplastic dilatation of the proximal femoral metaphyses, bilaterally. In this case, an arthrogram was performed that showed slight subluxation of the left hip because of the deformation of the upper femur. No surgical treatment was necessary.
- AP radiograph of the chest of a 26-year-old female with known multiple hereditary exostoses shows a large calcifying lesion arising from the proximal end of the left clavicle. The lesion bulged anteriorly beneath the skin to such an extent that the patient requested surgical removal. Note other small lesions on the ribs, both clavicles, and a sessile-based lesion on the left proximal humerus.
- AP radiograph of the right shoulder of a 31-year-old male with known multiple hereditary exostoses shows a large, sessile-based lesion arising from the proximal humerus. There is also a large, lobulated lesion arising from the scapula on the same side.
- This tangential view shows in better detail the lobulated pattern of a large osteochondroma arising from the posterior aspect of the scapula. The lesion was resected because of discomfort to the patient.
- CT scan through the scapular lesion showing the characteristic multilobulated pattern of the osteochondroma before it was excised.
- This lateral radiograph of the leg of a 26-year-old male with multiple hereditary exostoses shows chronic deformation of the metaphyseal portion of both the tibia and fibula, with one lesion on the proximal fibular eroding into the posteriolateral aspect of the tibia. It was asymptomatic and there was no need for surgical treatment.
- A 12-year-old girl developed symptoms of pain about the knee that resulted in this AP radiograph of the upper tibia. A geographic lytic lesion arises in the upper tibial epiphysis and extends across the thin growth plate into the proximal metaphysis. There is faint evidence of matrix calcification seen in the central area and a thin sclerotic margin between the lytic tumor and the surrounding bone.
- Coronal gadolinium contrast MRI image shows the lytic process in the epiphyseal-metaphyseal portion of the upper tibia with a signal void in the central area due to a lack of pickup of gadolinium in the avascular chondroid portion of the tumor. There is definite halo enhancement at the outer edge of the tumor where there is perfusion and a likelihood of giant cell activity.
- Sagittal T2-weighted MRI shows the high signal features of a chondroid lesion in the proximal tibial epiphyseal-metaphyseal area. It is clearly a chondroblastoma eroding through the posterior cortex but not bulging into the surrounding soft tissue.
- Low power photomicrograph shows the typical polyhedral-shaped stromal chondroblastic cells with distinct clear halos surrounding them giving it a chicken wire appearance. There is chondroid matrix formation and a few scattered multi-nucleated giant cells, quite diagnostic of a benign chondroblastoma, The treatment consisted of aggressive local curettement and packing of the defect with methyl methacrylate. The chance of local recurrence is about 10% but minimal chance of conversion to a higher grade tumor.
- A 26-year-old male presented with symptoms of pain in the knee for two months. This AP radiograph of the knee shows a calcifying epiphyseal lesion just beneath the tibial spine measuring about 2 cm in diameter that has the classic appearance of a epiphyseal chondroblastoma.
- Lateral radiograph again shows the lesion with matrix calcification located in the posterior aspect of the proximal tibial epiphysis. It is bulging posteriorly into the adjacent soft tissue.
- Sagittal T1-weighted MRI shows the signal abnormality arising from the chondroblastoma that is bulging out the posterior cortex of the proximal tibial epiphyseal-metaphyseal area. It has a mixed intermediate and low signal secondary to calcification within the chondroid lesion and a reactive shell of bone on the outer periphery.
- Sagittal T2-weighted MRI shows the high signal characteristics of the chondroblastoma eroding out through the posterior cortex of the proximal tibia with signal voids in the central area created by the calcification within the chondroid matrix.
- Low power photomicrograph taken from the curettement tissue shows the typical clear cell appearance of the chondroblasts forming chondroid matrix with a few reactive giant cells but no evidence of mitotic activity. This picture is quite diagnostic of a benign chondroblastoma. The patient was treated by aggressive curettement of the lesion through a posterior approach and the area was packed with methyl methacrylate to reduce the chance of local recurrence (about 5-10%).
- This fifty two year old female presented with a one year history of pain in the knee which by x-ray shows early degenerative changes in the lateral compartment and a cytic lesion beneath the lateral plateau that could be mistaken for chondroblastoma. In this case, however, we are seeing a degenerative granuloma or geode pointed out by the arrows.
- In the coronal MRI we see the low signal T-1 weighted granuloma (geode) just beneath the lateral plateau which turns bright on the T-2 image. Note the many changes in the knee joint to go along with the diagnosis of early osteoarthritis.
- Here we see the sagittal T-1 and axial T-2 which shows the similar characteristics of a chondroblastoma. The treatment for this pseudotumor would be a total knee joint replacement at which time the geode could be easily curetted and packed with bone cement.
- A 21-year-old female had symptoms of pain and swelling about the knee for four months. AP and lateral radiographic views of the knee show a geographic lytic lesion measuring about 3 cm in diameter directly beneath the proximal tibial spine with a sclerotic outer edge and matrix calcification in the central area. This proved to be a chondroblastoma which was treated by curettage and packing with bone cement.
- A 16-year-old boy gave a history of dull, aching pain in this knee for the past two months. This AP radiograph shows vague evidence of lytic changes within the distal femoral epiphysis just off the intercondylar notch.
- On this lateral radiograph it is very difficult to see the lytic lesion in the condylar area. An MRI was ordered for better definition of the lesion.
- Coronal proton density MRI shows a signal abnormality in the distal femoral epiphysis, laying directly on the subchondral area of the knee joint. The lesion measures about 2 cm in diameter and has a very thin, sclerotic, bony edge.
- Sagittal proton density MRI shows the well-circumscribed signal abnormality in the distal femoral epiphysis on the subchondral area of the joint, in a location typical for a chondroblastoma.
- Axial proton density MRI shows the chondroblastoma located just in front of the notch area of the distal femoral epiphysis.
- The patient was taken to the operating room and, through a standard arthrotomy approach to the knee, the surgeon was able to visualize the tumor bulging into the intercondylar notch area. This operative photograph shows curettements removed from the tumor just within the medial femoral condyle. Following a thorough debriedement, the defect was packed with methyl methacrylate.
- Low power photomicrograph of the surgical specimen shows the typical histological appearance of a chondroblastoma with multiple, large giant cells scattered throughout a field of mononuclear chondroblasts and mononuclear macrophages. The chondroblasts have the typical clear halo seen around the nuclei, giving the cells a clear cell appearance. This is the classic picture for a chondroblastoma.
- High power photomicrograph showing the clear cell chondroblasts with halos around the nuclear patterns that are fairly large and hyperchromatic appearing. One giant cell is seen in this field.
- An 18-year-old male presented with symptoms of pain and swelling about the knee of four months duration. This lateral radiograph shows a geographic lytic lesion located in the distal femoral epiphysis with matrix calcification, quite diagnostic for a chondroblastoma.
- CT scan through the epicenter of the lesion shows in better detail the matrix calcification in the geographic lytic process. There is a slight sclerotic edge to the lesion, located directly beneath the articular surface of the patellofemoral joint.
- The patient was taken to the operating room and the lesion was explored through an anterior arthrotomy. A surgical specimen microscopically shows numerous chondroblasts with a clear cell appearance and evidence of chondroid matrix being produced.
- A 20-year-old male presented with symptoms of pain and limp in his left hip. This AP radiograph shows a multiloculated, geographic, lytic destructive process involving the base of the femoral neck and the greater trochanteric area. There is a vague suggestion of matrix calcification that might represent a bone cyst, giant cell tumor or, in this case, a biopsy revealed a chondroblastoma with an associated aneurysmal bone cyst.
- Axial T2-weighted MRI through the level of the greater trochanter shows a very large, high signal abnormality displacing most of the intertrochanteric tissues, as well as a large aneurysmal component bulging out into the surrounding soft tissue, especially in a posterior direction. It suggests an aneurysmal bone cyst associated with the chondroblastoma. The initial radiologist was very concerned about the diagnosis of a hemorrhagic osteosarcoma.
- Sagittal T2-weighted MRI shows a very large, high signal abnormality involving the entire upper third of the femur with a large aneurysmal component outside, suggesting extensive hemorrhagic response to the underlying chondroblastoma.
- During the curettage procedure, the surgeon noted a very large hemorrhagic cyst that had the appearance of a aneurysmal bone cyst. However, curetting deep into intertrochanteric portion of the upper femur, he found solid, fleshy tissue that had the appearance of a giant cell tumor. Histologically the specimen showed giant cell activity but with typical chondroblastic cells with halos around them in the background, suggesting the diagnosis of a benign chondroblastoma.
- AP radiograph of the hip following the surgery shows the the tumor was successfully removed and the hip stabilized with a DHS sliding hip device. Methyl methacrylate was also used to reduce the chance of local recurrence and prevent pathological fracture. The patient did well and five years later showed no signs of recurrence or disability.
- A 12-year-old girl presented with a painful left-sided limp of two months duration. This AP radiograph of the hip shows a 2 cm lytic lesion located in the center of the proximal femoral epiphysis with evidence of diffuse matrix calcification that strongly suggests the diagnosis of a benign epiphyseal chondroblastoma.
- CT scan through the femoral head shows the calcifying matrix of the epiphyseal lesion in the femoral head that displaces approximately 80% of the epiphysis.
- Close-up CT scan of the left hip showing evidence of classic matrix calcification suggesting a chondroid lesion of a benign nature.
- The patient was taken to the operating room and through a posterior approach, a small window was made in the upper portion of the neck of the femur. The lesion was curetted and packed with cancellous bone, taken from the patient's own iliac crest on the same side, to avoid possible fracture through the lesion at a later date. This photomicrograph from the surgical specimen shows benign chondroid tissue with macrophage activity surrounding the cartilage, and clear cell chondroblasts as well.
- A 13-year-old boy presented with a painful limp of three months duration. This AP radiograph of the hip joint shows a well-defined, lytic lesion of a geographic nature in the femoral epiphysis with sclerotic edges and the suggestion of a smoky calcific matrix, quite characteristic for a benign chondroblastoma. This lesion was treated by simple curettage through an anterior approach, following which the defect was packed with autogenous bone graft taken from the patient's iliac crest.
- A 15-year-old boy presented with symptoms of pain the in shoulder for two months. This AP radiograph of the shoulder shows a geographic, lytic process in the proximal humeral epiphysis with definite evidence of matrix calcification. The lesion stops at the arrested growth plate.
- CT scan through the humeral epiphysis shows the geographic lesion located just lateral to the bicipital groove, bulging anteriorly into the soft tissue with evidence of matrix calcification.
- Axial T1-weighted MRI shows through the humeral epiphysis shows the low signal features of a chondroblastic tumor arising from the humeral head and bulging out beneath the anterior portion of the deltoid muscle.
- Coronal T2-weighted MRI shows the high signal features of the chondroblastoma bulging laterally from the proximal humeral epiphysis with low signal areas secondary to the calcification within the tumor.
- Gross macrosection taken from another patient with a chondroblastoma of the proximal humerus that was overtreated with a wide resection. This gives a wonderful picture of what the chondroblastoma looks like in the upper humerus, eroding into the subadjacent bone with a lobulated pattern characteristic of the epiphyseal chondroblastoma.
- Biopsy specimen from the original case showing the typical clear cell pattern of a benign chondroblastoma with matrix calcification.
- Another low power photomicrograph showing a few scattered giant cells with a multitude of clear cells in the background, representing benigh chondroblasts. There is one small area of cartilage matrix formation in the upper right hand corner.
- A 15-year-old boy had pain and swelling about his shoulder for four months. This AP radiograph of the shoulder shows an extensive multiloculated, geographic lysis of the proximal and lateral aspects of the epiphyseal-metaphyseal portion of the upper humerus with evidence of matrix calcification. This picture suggests an aneurysmal bone cyst associated with a chondroblastoma.
- Coronal T1-weighted MRI shows a large geographic signal abnormality replacing much of the lateral upper meta-epiphyseal portion of the proximal humerus with soft tissue bulging laterally underneath the deltoid muscle.
- This coronal T2-weighted MRI shows a large, bright signal abnormality in the lower portion of the tumor that represents the aneurysmal component of the tumor. Above this is the bright signal mixed with lower signal where the chondroid portion of the tumor is partially calcified.
- Low power photomicrograph from the surgical specimen after aggressive curettement of the tumor and packing with bone cement shows multiple large giant cells surrounded by clear cell chondroblasts.
- Another photomicrograph showing a monotonous field of clear cell chondroblasts and one giant cell in the lower right hand corner. Following the curettage and cementation of this lesion, the patient did well without local recurrence.
- A 24-year-old female presented with symptoms of pain in her ischium with sitting for the past three months. This AP radiograph of the hip shows a motheaten, lytic process within the entire ischial portion of her lower pelvis with matrix calcification suggesting the diagnosis of either chondrosarcoma or chondroblastoma. In this case, a biopsy proved the diagnosis of chondroblastoma.
- CT scan through the lower portion of the pelvis shows lytic changes throughout the entire inferior pubic ramus, extending down into and including the entire ischium. There is evidence of matrix calcification in the ischium, characteristic of chondroblastoma.
- CT scan cut at a higher level showing lytic changes extending up into the posterior column of the acetabulum as well.
- The patient was taken to the operating room and in a lithotomy position the entire ischial area and the posterior column of the acetabulum was curetted free of tumor. Microscopically, the tumor has a monotonous field of clear cell chondroblasts and a few scattered giant cells.
- A 21-year-old male had symptoms of pain in the pelvic area for six months. This CT scan through the pelvis shows a geographic lytic lesion located in the ilium of the pelvis. It is sharply marginated with a sclerotic edge, has evidence of matrix calcification and bulges laterally through the cortex. This picture is very characteristic for a chondroblastoma, which was proven on biopsy. Other conditions of concern might include a chondrosarcoma.
- CT scan at a different level shows again the motheaten appearance of the chondroblastoma with evidence of matrix calcification.
- Axial T2-weighted MRI shows a large signal abnormality arising from the body of the ilium. It has a lobulated pattern expanding through the cortex with evidence of inflammatory activity in the soft tissue surrounding the lesion, both inside and outside the pelvic wall. This lesion was treated aggressively by curettage and packing with methyl methacrylate
- A 43-year-old female developed symptoms of pain and swelling about the elbow three months before these films were taken. AP and lateral radiographic views of the elbow show a lytic tumor with matrix calcification arising from the capitellar area of the distal humerus and extending proximally a distance of 5 cm. On biopsy this lesion proved to be a chondroblastoma, It was curetted aggressively and packed with bone cement, The patient had a good clinical outcome.
- CT scan through the distal portion of the humerus that shows the lytic process in the capitellar area of the distal humeral epiphysis.
- An 11-year-old boy presented with symptoms of pain in his lateral ankle of two months duration. This mortice view of the ankle shows a geographic lytic process within the distal fibular epiphysis with a vague, smoky suggestion of matrix calcification. On biopsy, this lesion proved to be a chondroblastoma.
- Sagittal T1-weighted MRI of the ankle shows a low signal abnormality located in the distal fibular epiphysis, characteristic of chondroblastoma.
- Axial T2-weighted MRI shows a bright signal abnormality replacing most of the bone within the distal fibular epiphysis.
- The patient was taken to the operating room and the epiphyseal chondroblastoma was curetted through an anterior approach. This photomicrograph of the surgical specimen shows histology typical for chondroblastoma with a few giant cells scattered throughout. The surgical defect was packed with methyl methacrylate and there was no recurrence.
- AP radiograph of the ankle of a 12-year-old girl shows a lytic lesion in the distal fibular epiphysis with extensive matrix calcification that on curettage and biopsy revealed the diagnosis of a chondroblastoma. The surgical defect was packed with bone graft.
- An 18-year-old male presented with symptoms of pain and swelling about the ankle for three months. This mortice view of the ankle shows a geographic lysis in the dome of the talus laterally that had a smoky appearance secondary to diffuse matrix calcification, characteristic of a chondroblastoma.
- Lateral radiograph again showing the geographic lytic appearance of a chondroblastoma in the body of the talus. This lesion was aggressively curetted and packed with autogenous bone graft with an excellent surgical result.
- This AP radiograph of the tibia of an 11-year-old boy shows a large soap-bubbly lytic lesion involving a large portion of the proximal tibial metaphysis. The margins are well-defined and sclerotic with pseudoseptation going across the lesion that gives the soap-bubbly appearance sometimes seen with solitary bone cysts and fibrous dysplasia. The cortex is thinned out and slightly dilated medially to the point where it is nonexistent in several areas. The central portion of the lesion has a smoky appearance suggesting a solid lesion as opposed to a bone cyst which would have a dark appearance in the center.
- Planogram radiographic image that shows in better detail the pseudoloculated appearance of this soap-bubbly lesion.
- Photograph at the time of surgery shows the lobulated appearance of a solid chondroid tumor such as a large enchondroma with the succulent bluish white appearance of a cartilaginous tumor but with other areas that have a more fibrotic appearance similar to fibrous dysplasia.
- On this scanning lens photomicrograph note the lobulated pattern of a chondroid tumor interdigitated with fibrotic tissue with giant cell activity.
- Low power photomicrograph showing a benign myxoid pattern to one side and on the other side there is fibrous tissue speckled with multinucleated giant cells, which is almost diagnostic of a chondromyxoid fibroma.
- The appearance of the outer edge of the lesion after a careful debriedement with curettes and a high speed burr. This technique is also used for a giant cell tumor in the same location.
- Intraoperative photograph following packing of the curetted defect with cancellous bone graft with a fibular strut placed into the defect before closure of the wound.
- Postoperative radiograph shows the defect packed with autogenous bone graft taken from the patient's iliac crest and fibula on the same side. The lesion went on to heal nicely without recurrence and the patient was able to return to normal physical activity.
- This 50 year male presented with a 6 month history of a slow growing mass over the anterior and proximal tibia which on x-ray shows a well marginated lytic lesion in the anterior tibial metaphyseal cortex with sclerotic edges suggesting benign disease such as a non ossifing fibroma. The soft tissue mass bulging beneath the skin was biopsied and the diagnosis of chondromyxoid chondroma was made. This soft tissue mass with streaking calcification in it is unusual for this condition
- This coronal T-1 MRI shows a low signal pattern for this lesion.
- The coronal proton density MRI shows a bright signal to the lesion.
- The axial PD MRI is also bright and shows considerable erosion of the anterior tibial cortex similar to a periosteal chondroma.
- The axial Gad contrast MRI shows excellent perfusion of the tumor. This tumor was treated with local debriedment and cortical curettement.
- A 12-year-old girl presented with symptoms of pain below the knee of six months duration. AP and lateral radiographic views of the proximal tibia show a geographic lytic process involving the medial aspect of the proximal tibial metaphysis with a faint suggestion of matrix calcification, suggesting a low-grade chondroid tumor. This lesion was curetted and biopsy revealed the diagnosis of a chondroid myxoid fibroma. The cavity was packed with bone graft and there was no recurrence.
- A 13-year-old female developed pain and swelling about her proximal tibia eight months before these films were taken. AP and lateral radiographic views show a motheaten appearance to the proximal tibial metaphysis with cortical breakthrough laterally and evidence of matrix calcification in the proximal end of the tumor. The process looks very much like monostotic fibrous dysplasia but in this case a biopsy proved the lesion to be a chondromyxoid fibroma which is a similar clinical condition. It was treated by aggressive curettage and bone grafting.
- Radiographic evidence of a destructive lytic lesion involving the proximal half of the first metatarsal. There is cortical breakthrough laterally, bulging out into the surrounding soft tissue and slight matrix calcification suggesting a monostotic fibrous dysplasia or, as was biopsy proven in this case, a chondromyxoid fibroma.
- Oblique radiograph of the forefoot area showing the lytic lesion within the first metatarsal with slight cortical dilatation and a suggestion of breakout anteriorly.
- Photomicrograph of the surgical specimen shows a lobulated chondroid pattern with cartilage matrix formation surrounded by macrophage activity and large giant cells and fibrous tissue, suggestive of the diagnosis of a chondromyxoid fibroma.
- This photomicrograph shows definite chondroid matrix being formed in the center of the field with a few scattered giant cells and fibrous tissue at the outer edge, and a faint suggestion of a myxoid pattern as well, characteristic of chondromyxoid fibroma.
- AP radiograph of the distal forearm of a 7-year-old female who presented with a painful, swollen lesion in her distal ulna shows a lytic destructive lesion breaking through the cortex circumferentially. It involves the entire distal metaphysis and suggests the diagnosis of an aneurysmal bone cyst. However, on biopsy this lesion turned out to be a chondromyxoid fibroma.
- This photomicrograph from the biopsy specimen shows a fair amount of chondroid tissue being formed by the tumor, along with scattered giant cells and benign-appearing fibroblastic tissue. The lesion was treated by aggressive curettement of the tumor and packing with bone graft. There was no recurrence of the tumor.
- A special rib detail radiograph of a 25-year-old female who presented with pain in the left ribcage with coughing shows an expansile, motheaten lesion that is dilating the mid portion of one of her ribs. There is evidence of matrix calcification that might suggest the diagnosis of a chondroblastoma but, in this case, the tumor turned out to be a chondromyxoid fibroma.
- Low power photomicrograph resulting from curettement of the lesion reveals evidence of chondroid tissue as well as myxoid areas at the edge of the cartilage and giant cell activity with fibrous tissue seen in the upper lefthand corner.
- This 60 year old female presented with sacro-coccygeal pain for three months with this x-ray that shows a small benign appearing lytic lesion in the disstal sacrum that could be a chordoma. On biopsy, however, it turned out to be a chondromyxoid fibroma.
- On the sagittal T-1 image the lesion is low signal and is located in the S-4 and 5 segments. It is bright on the T-2 image with evidence of anterior cortical breakthru and posterior invasion of the thecal canal similar to the appearance of a sacral chordoma.
- Here we see the axial T-1 image which is low signal and the T-2 is bright. It is located in one half of the distal sacrum.
- This coronal T-1 image shows the lesion to be low signal and unilateral. Because the patient experienced pain in the area and for fear this might progress like a chordoma, a simple marginal resection was carried out with minimal neurologic deficiency. This is a very rare location for a chondromyxoid fibroma and has been reported in less than three cases in this location.
