Chronic Exertional Rhabdomyolysis in Horses
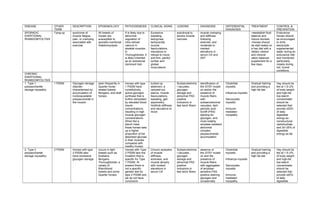
- 1. DISEASE OTHER TERM DESCRIPTION EPIDEMIOLOGY PATHOGENESIS CLINICAL SIGNS LESIONS DIAGNOSIS DIFFERENTIAL DIAGNOSIS TREATMENT CONTROL & PREVENTION SPORADIC EXERTIONAL RHABDOMYOLYSIS Tying-up syndrome of muscle fatigue, pain, or cramping associated with exercise. All breeds of horses are susceptible to sporadic exertional rhabdomyolysis. It is likely due to abnormal regulation of intra-cellular calcium in skeletal muscles. In Thoroughbreds, it is likely inherited as an autosomal dominant trait. Excessive sweating, tachypnea, tachycardia, muscle fasciculations, reluctance or refusal to move, and firm, painful lumbar and gluteal musculature. subclinical to severe muscle necrosis muscle cramping and stiffness following exercise, and moderate to marked elevations in serum CK and AST -reestablish fluid balance and induce diuresis -Horses should be stall rested on a hay diet with a dietary vitamin and mineral ration balancer supplement for a few days. Endurance horses should be encouraged to drink electrolyte- supplemented water during an endurance ride and monitored particularly closely during hot, humid conditions. CHRONIC EXERTIONAL RHABDOMYOLYSIS 1. Type 1 polysaccharide storage myopathy 1 PSSM Glycogen storage disorder characterized by accumulation of nonbioavailable polysaccharide in the muscle seen frequently in Quarter horse- related breeds Morgans, and draft horses Horses with type 1 PSSM have constitutively active glycogen synthase that is further stimulated by elevated blood insulin concentrations, resulting in high muscle glycogen concentrations. When fed a starch meal, these horses take up a higher proportion of the absorbed glucose in their muscles compared with healthy horses. tucked-up abdomen, a camped-out stance, muscle fasciculations, sweating, gait asymmetry, hindlimb stiffness, and reluctance to move Subsarcolemma l vacuoles, glycogen storage and abnormal PAS positive inclusions in fast twich fibers identification of the GYS1 mutati on and/or the presence of muscle fibers with subsarcolemmal vacuoles, dark periodic acid- Schiff (PAS) staining for glycogen, and most notably, amylase-resistant abnormal complex polysaccharide accumulation Clostridial myositis Influenza myositis Sarcocystis myositis Immune- mediated myopathy Gradual training and providing a high fat diet Hay should be fed at 1.5–2% of body weight and high-fat, low-starch concentrates should be selected that provide ≤20% of daily digestible energy as nonstructural carbohydrate and 20–25% of digestible energy as fat. 2. Type 2 polysaccharide storage myopathy 2 PSSM Horses with type 2 PSSM also have excessive glycogen storage. occurs in light breeds such as Arabians, Morgans, Thoroughbreds, a variety of Warmblood breeds and some Quarter horses Horses with Type 2 PSSM lack the mutation that is specific for Type 1 PSSM. At present there is not a specific genetic test for type 2 PSSM and we do not have conclusive Chronic episodes of muscle stiffness, soreness, and muscle atrophy with modest elevations in serum CK Subsarcolemma l vacuoles, glycogen storage and abnormal PAS positive inclusions in fast twich fibers absence of the GYS1 mutati on and the presence of muscle fibers with aggregates of amylase- sensitive PAS positive staining glycogen and occasionally Clostridial myositis Influenza myositis Sarcocystis myositis Immune- mediated myopathy Gradual training and providing a high fat diet Hay should be fed at 1.5–2% of body weight and high-fat, low-starch concentrates should be selected that provide ≤20% of daily digestible
- 2. evidence that it is inherited. small amounts of amylase-resistant PAS positive material. energy as nonstructural carbohydrate and 20–25% of digestible energy as fat 3. Recurrent exertional rhabdomyolysis RER Recurrent exertional rhabdomyolysis (RER) is caused by an abnormality in intracellular calcium regulation It is seen frequently in Thoroughbreds, Standardbreds, and Arabian horses. It appears there is intermittent disruption of muscle contraction, particularly when horses susceptible to the condition are fit and have a nervous temperament. horses sweat profusely, breathe rapidly and become stiff and reluctant to move. The cells from the affected horse have nuclei located toward the center of mature muscle fibers rather than underneath the cell membrane as they are in the healthy muscle cells. history, clinical signs, elevations in serum CK and AST, and muscle biopsy. Clostridial myositis Influenza myositis Sarcocystis myositis Immune- mediated myopathy Phenytoin (1.4– 2.7 mg/kg, PO, bid) decreasing the triggering factors for excitement and pharmacologic alteration of intracellular calcium flux with contraction SARCOCYSTIS MYOSITIS Cysts of the sporozoan parasite Sarcocystis are present in 90% of esophageal muscles from horses >8 yr of age and in 6% of gluteal muscle biopsies from healthy horses Occasionally, heavy infestations occur through contamination of feed with canine feces After ingestion of sporocysts by a suitable intermediate host, sporozoites are liberated and initiate development of schizonts Merozoites are liberated from the mature schizonts and produce a second generation of endothelial schizonts in capillaries from several organs. Merozoites from this second generation subsequently invade the muscle fibers and develop into the typical sarcocysts. fever, anorexia, stiffness, weight loss, muscle fasciculations, and weakness. Muscle atrophy history, clinical signs, laboratory evaluation, and the demonstration of an inflammatory reaction to immature cysts in muscle biopsies. NSAID and drugs such as trimethoprim sulfa and pyrimethamine or ponazuril. Supplies of grain and feed should be kept covered; dogs and cats should not be allowed in buildings used to store feed or house animals STREPTOCOCCUS Severe It is not clear A stiff gait is the At postmortem, hematologic vitamin IV penicillin
- 3. EQUI RHABDOMYOLYSIS rhabdomyolysis can occur in horses with Streptococcus equi equi submandibular lymphadenopathy and/or guttural pouch empyema. whether myonecrosis is a direct toxic effect of S equi on muscle cells or is due to profound nonspecific T cell stimulation by streptococcal superantigens and the release of high levels of inflammatory cytokines. initial clinical sign, which progresses rapidly to severely painful, firm, swollen, epaxial and gluteal muscles. large, pale areas of necrotic muscle are evident in hindlimb and lumbar muscles. histopathologic lesions are characterized by severe acute myonecrosis with a degree of macrophage infiltration. Sublumbar muscles often show the most severe and chronic necrosis as indicated by greater macrophage infiltration of myofibers. abnormalities typical of S equi infection, marked elevations in CK (>100,000 U/L), and PCR or bacterial culture. E/selenium deficiency ionophore toxicity PSSM combined with an antimicrobial that inhibits protein synthesis, such as rifampin. Flushing infected guttural pouches and draining abscessed lymph nodes NSAID and possibly high doses of short- acting corticosteroids CLOSTRIDIAL MYOSITIS myonecrosi s A variety of clostridial bacteria can sporulate at the site of an injection or deep wound causing focal muscle swelling and systemic toxemia in horses Clostridium septicum, Clostridium chauvoei, Clostridium sporogenes, and mixed infections are associated with a high fatality rate, whereas Clostridium perfringens type A has a mortality rate of 20% with early and aggressive treatment. Clostridial spores may lie dormant in skeletal muscle, or spore deposition directly into the tissue may occur in association with penetration. If suitable necrotic conditions exist, the spores convert to the vegetative form releasing powerful exotoxins. Within 48 hr, horses show depression, fever, toxemia, tachypnea, and swelling and variable crepitus at the injection site. Tremors, ataxia, dyspnea, recumbency, coma, and death may occur in the next 12–24 hr. At postmortem, swelling, crepitus, and autolysis are rapid, and bloodstained fluid is often observed discharging from body orifices. Ultrasonographic evaluation Aspirates of affected tissues examined via direct smears or fluorescent antibody staining Anaerobic bacterial culture Wound fenestration and aggressive surgical debridement over the entire affected area Additional treatment includes high doses of IV potassium penicillin every 2–4 hr until the animal is stable (1 to 5 days), combined with or followed by oral metronidazole along with supportive fluid therapy and anti- inflammatory agents MUSCLE Staphylococcus develops following Initially there is an depends on its There may be Ultrasonography poulticing,
- 4. ABSCESSES aureus, Streptococcus equi, and Corynebacterium pseudotuberculos is are common causes of skeletal muscle abscessation penetrating injuries or by hematogenous or local spread of infection ill-defined cellulitis, which may heal or progress to a well-defined abscess. An abscess may heal, expand, or fistulate, usually to the skin surface with potential for a chronic granuloma with intermittent discharge location and can vary from mild stiffness to severe lameness. an elevated fibrinogen and nucleated WBC. and culture of aspirated fluid lancing, flushing, and draining IMMUNE MEDIATED MYOPATHIES 1. INFARCTIVE HEMORRHAGIC PURPURA Purpura hemorrhagica is a noncontagious, type III immune- mediated vasculitis of horses that is characterized by subcutaneous edema of the head, ventral abdomen, and limbs and by petechial hemorrhages of the mucous membranes. most commonly affects young adult horses, although the disease has been identified in yearlings as well as geriatric horse. There appears to be no breed or sex predilection. most often occurs as a rare complication of Streptococcus equi infection but can also develop after infection with other bacterial and viral organisms, particularly those that cause formation of purulent or necrotic foci. mild elevations in serum CK activity unilateral lameness variable edema, acute colic, firm swellings within muscle and under the skin based on clinical signs, a leukocytoclastic vasculitis in skin and affected tissues, and very high S equi M protein titer early detection, penicillin for 14 days, and prolonged high doses of dexamethasone (0.12–0.2 mg/kg) for at least 10 days, followed by tapering doses of prednisolone at an initial dosage of 2 mg/kg. 2. IMMUNE- MEDIATED MYOSITIS It occurs in Quarter Horses, although other breeds may be affected. The condition shows a bimodal age distribution affecting horses <8 yr or >16 yr of age In approximately one-third of affected horses, a triggering factor appears to have been exposure to S equi or a respiratory disease. Rapid onset of atrophy of the back and croup muscles is accompanied by stiffness and croup stiffness and malaise mild to moderate elevations in serum CK and AST Muscle biopsy of epaxial and gluteal muscles shows lymphocytic vasculitis, anguloid atrophy, myofiber infiltration with lymphocytes, fiber necrosis with macrophage biopsy antibiotic therapy for horses with concurrent signs of infection and administration of dexamethasone (0.05 mg/kg for 3 days), followed by prednisolone (1 mg/kg for 7–10 days) tapered by 100 mg/wk over 1 mo
- 5. malaises. infiltration, and regeneration in acute stages. NUTRITIONAL MYODEGENERATI ON White muscle disease nutritional myodegeneration of foals is a peracute to subacute myodegenerative disease affecting skeletal and cardiac muscle Young, rapidly growing foals born to dams that consumed selenium deficient diets during gestation can develop nutritional myodegeneration Selenium is an essential component of 5 antioxidant selenoproteins and vitamin E acts as an antioxidant within lipid bilayers. Muscle degeneration is the result of oxidant damage to cell membranes and proteins leading to a loss of cellular integrity. Clinical signs in foals include dyspnea; a rapid, irregular heartbeat; and sudden death in those with myocardial involvement. Dysphagia, muscle stiffness, trembling, firm muscles, difficulty rising, and myoglobinuria may also be seen. moderate to marked elevated serum CK and AST, combined with low whole blood selenium concentrations (<0.07 ppm) or vitamin E (<2 ppm). severe rhabdomyolysis spinal cord compression, cerebellar disease, suppurative and nonsuppurative meningitis/myeliti s, polyarthritis, neurotoxins such as organophosphate s, tetanus, pelvic fractures, parasitic myositis, clostridial myositis, and traumatic injuries M injection of selenium (0.055– 0.067 mg/kg) and either injectable or oral vitamin E (0.5–1.5 IU/kg) administration of antibiotics to combat secondary pneumonia and feeding via nasogastric tube, provision of adequate energy intake, and attention to the fluid and electrolyte balance. PLANTS CAUSING MYOPATHIES 1. TREMATONE CONTAINING PLANTS Horses ingesting 0.5–2% body weight of trematone- containing plants are likely to die from skeletal muscle and cardiac muscle necrosis Trematone is hypothesized to interfere with glucose metabolism marked depression, weakness, low head posture, and increased cardiac and respiratory rate Serum AST and CK are often markedly elevated, and serum electrolyte abnormalities such as hypocalcemia, hyponatremia, hypochloremia, hyperkalemia, and hyperphospha- temia may be present skeletal muscle and cardiac muscle necrosis Supplemental feeding with high quality forage, fluid therapy with glucose as needed, and rest. Trematone remains active in the hay and in the stalks of the dead plants on pasture, so both the fresh and the dried form of the plants should be kept from horses. 2. ATYPICAL MYOGLOBINURIA Pasture myopathy Atypical myoglobinuria occurs sporadically in horses kept on pasture, usually It occurs most often in spring and autumn and is often associated with a sudden deterioration in The cause is unknown but appears to involve disruption in lipid metabolism due Affected horses are reluctant to move, have muscle weakness and fasciculations, pulmonary edema may be present Necropsy reveals clinical signs and a blood test The disease can look similar to a severe case of colic. Supportive therapy including antioxidants (eg, vitamin C, vitamin E, riboflavin) and IV fluids Provision of supplementary feeding, especially during periods of inclement
- 6. with no supplemental feeding. weather conditions. to exposure to a toxin in well grazed, cool, wet pastures. and may become recumbent. Choke may be present, and gut sounds may be reduced, with reduction in feces production, although appetite may be unaffected. widespread myodegeneratio n in postural and respiratory skeletal muscles and the myocardium. containing dextrose are recommended weather Clean, fresh water supply Traumatic and Anesthetic Myopathies 1. POST- ANESTHETIC MYOPATHY Following anesthesia, horses may develop severe muscle pain and weakness in one or more muscle groups. Generalized myopathies may develop in horses that were hypotensive during anesthesia. Hypoperfusion of compressed muscle groups with resultant high intracompartment al pressure is the most important causative factor for focal muscle involvement Horses may appear distressed, with profuse sweating, tachycardia, and tachypnea. A dropped elbow stance typical of radial nerve paralysis characterizes triceps myopathy. Gluteal myopathy results in unwillingness to bear weight on the hindlimbs. Affected muscles may feel very hard and show localized swelling. History and clinical signs Pain relief is provided by sedation with detomidine, combined with opiate analgesics and NSAID. Fluid therapy helps maintain renal perfusion and urine output and ensure adequate muscle perfusion. minimizing the time under general anesthesia, careful positioning of the horse on the operating table, and maintenance of arterial blood pressure above 60 mm Hg using fluid therapy and inotropic agents such as dobutamine 2. FIBROTIC MYOPATHY Fibrotic myopathy describes a classic gait abnormality that develops when horses injure their semitendinosus and semimembranosu s muscles at the point of a tendinous insertion during exercise that requires abrupt turns and sliding stops Trauma (eg, catching a foot in a fence), IM injections, and a congenital form are other potential causes of fibrotic myopathy. develops when horses injure their semitendinosus and semimembranosu s muscles at the point of a tendinous insertion during exercise that requires abrupt turns and sliding stops characterized by an abrupt cessation of the anterior phase of the stride of the affected limb, causing the leg to jerk suddenly to the ground rather than continue its forward motion. The stride has a short anterior phase with a characteristic hoof-slapping gait. Chronically, hardened areas within the muscle may represent fibrosis and ossification. ultrasonography, thermography, or scintigraphy palpation acute cases may benefit from rest and cold therapy followed by deep heating ultrasound and controlled stretching. Chronic cases may require surgical excision or transection of the fibrotic part of the muscle or tenotomy of the tibial insertion of the semimembra- nosus tendon. MUSCLE CRAMPING
- 7. 1. ELECTROLYTE DISTURBANCES Muscle cramps can be induced by forceful contraction of a shortened muscle, by changes in the electrolyte composition of extracellular fluid, and by ear tick infestations in horses. most frequent in hot, humid weather. Horses may lose up to 15 L/hr of fluids in the form of sweat and develop remarkable deficits in sodium, potassium, chloride magnesium, and calcium. exhausted horses are often dull, depressed, and clinically dehydrated with elevated heart and respiratory rates and persistently elevated body temperature. muscle stiffness and periodic spasms of muscle groups. Mild muscle cramping is self- limiting, and the signs abate with rest or light exercise. Exhausted horses with metabolic derangements, however, require immediate treatment including plasma volume expansion with oral or IV isotonic polyionic fluids and cooling (using water and fans). Daily direct addition of 2 oz of sodium chloride and 1 oz of potassium chloride to the feed is recommended for horses with recurrent cramping, in addition to electrolyte supplementatio n before and after endurance rides. 2. HYPOCALCEMIA Transport tetany, Lactation tetany, Eclampsia an uncommon condition associated with acute depletion of serum ionized calcium and sometimes with alterations in serum concentrations of magnesium and phosphate. It occurs after prolonged physical exertion or transport (transport tetany) and in lactating mares (lactation tetany). . Corticosteroids inhibit vitamin D activity, which leads to decreased intestinal absorption and skeletal mobilization of calcium. Stress and lack of calcium intake have been associated with transport tetany. synchronous diaphragmatic flutter ,anxious appearance, and signs of tetany, including increased muscle tone, stiffness of gait, muscle tremors, prolapse of the third eyelid, inability to chew, trismus, salivation, recumbency, convulsions, and cardiac arrhythmias. signs, history, and response to treatment tetanus, endotoxemia, colic, exertional rhabdomyolysis or other muscle disorder, seizure disorder, laminitis, and botulism IV administration of calcium solutions, such as 20% calcium borogluconate A balanced feed ration should be provided to supply adequate amounts and ratios of calcium and phosphorus throughout gestation. Stress and fasting during transport should be minimized 3. SYNCHRONOUS DIAPHRAGMATIC FLUTTER Thumps Synchronous diaphragmatic flutter is due to firing of the phrenic nerve in synchrony with atrial depolarization, causing the Inciting causes include endurance exercise, hypocalcemia, hypoparathyroidis m, digestive disturbances, and repeated administration of The most consistently reported metabolic derangement is low serum ionized calcium concentrations usually rhythmic twitching or "thumping' in the flank area, in time with the beating of the heart Clinical signs calcium solutions IV For horses with chronic diaphragmatic flutter, provision of chloride, potassium, Limiting alfalfa hay, which has a relatively high calcium concentration, may be indicated in chronically affected
- 8. diaphragm to contract with each heartbeat. calcium-containing fluids to performance horses. associated with hypochloremic metabolic alkalosis. Metabolic alkalosis may alter the ratio of free to bound calcium which possibly induces diaphragmatic flutter. sodium, calcium, and magnesium during prolonged exercise may help reduce fluid losses and the metabolic alkalosis horses. 4. EAR TICK- ASSOCIATED MUSCLE CRAMPING Otobius megnini infestations in the ear canal can produce remarkably painful intermittent muscle cramps O megnini is found in the southwestern USA Otobius megnini infestations in the ear canal can produce remarkably painful intermittent muscle cramps not associated with exercise that last from minutes to a few hours and often resemble colic. Horses may fall over when stimulated. Percussion of triceps, pectoral, or semi- tendinosus muscles results in a typical myotonic cramp. Horses have elevated serum CK ranging from 4,000– 170,000 IU/L. Tick bites Numerous ear ticks can be identified in the external ear canal of affected horses. local treatment of the ear ticks using pyrethrins and piperonyl butoxide results in recovery within 12–36 hr. Acepromazine may be helpful to relieve painful cramping. Keeping animals away from tick-prone areas SHIVERS “Shivers” is a spastic condition of the hind- and occasionally forelimbs of horses that is usually only evident when horses are backing or having their feet picked up It is most common in adult draft horse breeds, Warmbloods, Warmblood crosses, and Thoroughbreds The condition is characterized by periodic, involuntary spasms of the muscles in the pelvic region, pelvic limbs, and tail that are exacerbated by backing or picking up the hindlimbs. The affected limb is elevated, abducted, and may actually shake and shiver; the tail head is usually elevated concurrently and trembles. Clinical signs There are no known treatments, but avoiding stall rest and keeping horses fit appears helpful. Myotonic Disorders 1. MYOTONIA CONGENITA AND DYSTROPHICA The initial signs of myotonia in foals are well- developed musculature and mild pelvic limb stiffness. Bilateral bulging (dimpling) of the thigh and Myotonia congenita usually does not show progression of clinical signs beyond 6–12 mo of age, and muscle stiffness may improve with Percussion of affected muscles exacerbates the muscle dimpling below a large area of tight contraction that can persist for a minute or more Foals with myotonia dystrophica show a progression of signs in the first 1–2 yr of life to include areas of muscle atrophy fibrosis and ringed fibers, numerous centrally displaced myonuclei, sarcoplasmic masses, and an increase in endomysial and tentative diagnosis of myotonia can be made on the basis of age and clinical signs of stiff gait, muscle bulging, and prolonged dystrophic foals usually require euthanasia due to the severity of stiffness and atrophy that develop over time
- 9. rump muscles is often obvious and gives the impression that the animal is very well developed. exercise. with subsequent slow relaxation. stiffness that worsens with exercise perimysial connective tissue contractions following muscle stimulation. Definitive requires electromyogra- phic exam. 2. HYPERKALEMIC PERIODIC PARALYSIS HyPP Hyperkalemic periodic paralysis (HYPP) is an inherited disease of the muscle which is caused by a genetic defect. In the muscle of affected horses, a point mutation exists in the sodium channel gene and is passed on to offspring. HyPP is an autosomal dominant trait affecting Quarter horses, American Paint horses, Appaloosas, and Quarter horse crossbreeds worldwide. When the defective sodium channel gene is present, the channel becomes "leaky" and makes the muscle overly excitable and contract involuntarily. The channel becomes "leaky" when potassium levels fluctuate in the blood. This may occur with fasting followed by consumption of a high potassium feed such as alfalfa. asymptomatic to intermittent muscle fasciculations and weakness with swaying, staggering, dogsitting, or recumbency may be seen, with severe attacks lasting 15–60 min or longer. Heart and respiratory rates may be elevated, but horses remain relatively bright and alert DNA testing of mane or tail hair delay before serum centrifugation, hemolysis, chronic renal failure, and severe rhabdomyolysis. low-grade exercise or feeding grain or corn syrup to stimulate insulin- mediated movement of potassium across cell membranes. In severe cases, administration of calcium gluconate or IV dextrose, alone or combined with sodium bicarbonate (1–2 mEq/kg), often provides immediate improvement. Prevention requires decreasing dietary potassium to 0.6–1.1% total potassium concentration and increasing renal losses of potassium. GLYCOGEN BRANCHING ENZYME DEFICIENCY GBED GBED is found in Quarter Horse or related bloodlines that causes late- term abortion or death of foals by a few months of age. Nine percent of Quarter horses and Paint horses carry the mutation and at least 3% of abortions are attributed to this disease in Quarter horses. Glycogen branching enzyme deficiency (GBED) is a glycogen storage disorder causing abortion, seizures, and muscle weakness in Quarter horse- related breeds caused by an autosomal recessive mutation in the glycogen branching enzyme (GBE1) gene. Most foals diagnosed with GBED present with hypothermia, weakness, and flexural deformities of all limbs at 1 day of age. Persistent leukopenia, intermittent hypoglycemia, and high serum CK (1,000–15,000 U/L), AST, and γ- glutamyltransferas e activities are features of affected foals. Gross lesions are not evident, and routine H & E stains of tissues may be normal or show basophilic inclusions in skeletal muscle and cardiac tissues. A diagnosis is best obtained by confirming the presence of the genetic mutation in tissue samples or by identifying typical PAS positive inclusions in muscle or cardiac samples. no successful treatment for GBED.
- 10. rump muscles is often obvious and gives the impression that the animal is very well developed. exercise. with subsequent slow relaxation. stiffness that worsens with exercise perimysial connective tissue contractions following muscle stimulation. Definitive requires electromyogra- phic exam. 2. HYPERKALEMIC PERIODIC PARALYSIS HyPP Hyperkalemic periodic paralysis (HYPP) is an inherited disease of the muscle which is caused by a genetic defect. In the muscle of affected horses, a point mutation exists in the sodium channel gene and is passed on to offspring. HyPP is an autosomal dominant trait affecting Quarter horses, American Paint horses, Appaloosas, and Quarter horse crossbreeds worldwide. When the defective sodium channel gene is present, the channel becomes "leaky" and makes the muscle overly excitable and contract involuntarily. The channel becomes "leaky" when potassium levels fluctuate in the blood. This may occur with fasting followed by consumption of a high potassium feed such as alfalfa. asymptomatic to intermittent muscle fasciculations and weakness with swaying, staggering, dogsitting, or recumbency may be seen, with severe attacks lasting 15–60 min or longer. Heart and respiratory rates may be elevated, but horses remain relatively bright and alert DNA testing of mane or tail hair delay before serum centrifugation, hemolysis, chronic renal failure, and severe rhabdomyolysis. low-grade exercise or feeding grain or corn syrup to stimulate insulin- mediated movement of potassium across cell membranes. In severe cases, administration of calcium gluconate or IV dextrose, alone or combined with sodium bicarbonate (1–2 mEq/kg), often provides immediate improvement. Prevention requires decreasing dietary potassium to 0.6–1.1% total potassium concentration and increasing renal losses of potassium. GLYCOGEN BRANCHING ENZYME DEFICIENCY GBED GBED is found in Quarter Horse or related bloodlines that causes late- term abortion or death of foals by a few months of age. Nine percent of Quarter horses and Paint horses carry the mutation and at least 3% of abortions are attributed to this disease in Quarter horses. Glycogen branching enzyme deficiency (GBED) is a glycogen storage disorder causing abortion, seizures, and muscle weakness in Quarter horse- related breeds caused by an autosomal recessive mutation in the glycogen branching enzyme (GBE1) gene. Most foals diagnosed with GBED present with hypothermia, weakness, and flexural deformities of all limbs at 1 day of age. Persistent leukopenia, intermittent hypoglycemia, and high serum CK (1,000–15,000 U/L), AST, and γ- glutamyltransferas e activities are features of affected foals. Gross lesions are not evident, and routine H & E stains of tissues may be normal or show basophilic inclusions in skeletal muscle and cardiac tissues. A diagnosis is best obtained by confirming the presence of the genetic mutation in tissue samples or by identifying typical PAS positive inclusions in muscle or cardiac samples. no successful treatment for GBED.
