Ncp Osteomyelytis
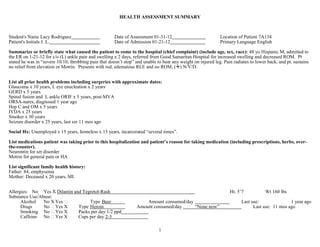
- 1. HEALTH ASSESSMENT SUMMARY Student's Name Lacy Rodriguez Date of Assessment 01-31-12 Location of Patient 7A134 Patient's Initials J. L. Date of Admission 01-21-12 Primary Language English Summarize or briefly state what caused the patient to come to the hospital (chief complaint) (include age, sex, race): 48 yo Hispanic M, admitted to the ER on 1-21-12 for c/o (L) ankle pain and swelling x 2 days, referred from Good Samaritan Hospital for increased swelling and decreased ROM. Pt stated he was in “severe 10/10, throbbing pain that doesn’t stop” and unable to bear any weight on injured leg. Pain radiates to lower back, and pt. sustains no relief from elevation or Motrin. Presents with red, edematous RLE and no ROM, () N/V/D. List all prior health problems including surgeries with approximate dates: Glaucoma x 10 years, L eye enucleation x 2 years GERD x 5 years Spinal fusion and L ankle ORIF x 5 years, post-MVA ORSA-nares, diagnosed 1 year ago Hep C and OM x 5 years IVDA x 25 years Smoker x 30 years Seizure disorder x 25 years, last szr 11 mos ago Social Hx: Unemployed x 15 years, homeless x 15 years, incarcerated “several times”. List medications patient was taking prior to this hospitalization and patient’s reason for taking medication (including prescriptions, herbs, over- the-counter). Neurontin for szr disorder Motrin for general pain or HA List significant family health history: Father: 84, emphysema Mother: Deceased x 20 years, MI. Allergies: No Yes X Dilantin and Tegretol-Rash Ht. 5’7 Wt 160 lbs Substance Use/Abuse: Alcohol No X Yes Type Beer Amount consumed/day Last use: 1 year ago Drugs No Yes X Type Heroin Amount consumed/day “None now” Last use: 11 mos ago Smoking No Yes X Packs per day 1/2 ppd Caffeine No Yes X Cups per day 2-3 1
- 2. Admitting Diagnosis (discuss briefly): Osteomyelitis: An inflammation of the bone caused by an infecting organism. May be related to vascular insufficiency related to IVDA. This is a local bone infection, which causes progressive destruction of the bone (Lewis, 2011). Current Diagnosis (including pathophysiology): Septic Arthritis: Develops when bacteria or fungi spread through the bloodstream to a joint, and into the normally aseptic synovial fluid. Septic arthritis is a joint infection and resulting inflammatory process, causing destruction of the synovial membrane. Results in cartilage damage and causes it to become yellow, dull and granular. Continued hanges in collagen structure may lead to fissures & erosion. The most common sites for this type of infection are the knee and hip. Most cases of acute septic arthritis are caused by bacteria such as staphylococcus or streptococcus. (Lewis, 2011). Labs: Increased WBCs (shift to the left, ESR and CRP. Decreased H & H. Positive BC. (Lewis, 2011). Risk Factors: IVDA, nutritional deficiency, joint implants, immunosuppressants, chronic illness, recent injury or trauma. More common in men before 45 yo. (Lewis, 2011). Signs and Symptoms: Tachycardia, fever, joint warmth, redness, swelling, stiffness, pain, fatigue, decreased ROM, irritability, fatigue, HA, decreased appetite, purulent drainage, nausea and vomiting. (Lewis, 2011) Summarize what has happened to this patient since being admitted to the hospital (include all diagnostic tests): Since being admitted to the hospital the pt has undergone an X ray to eval LLE that suggested infection and inflammation. He is on a regular diet after being NPO prior to I & D surgery, and eats 75%-95% of his meals, depending on his level of pain. The patient underwent surgery to remove old hardware from the L ankle, and drainage of purulent fluid from the joint. Dr. ordered PT after surgery, pt refused PT 3 times after surgery due to pain. Patient has been given several pain medications since being admitted, and requests pain medication about every 2 hours. He voids spontaneously and freely and has regular BMs. He is continuing to receive IV vanco via PICC to the LUE. He is awaiting placement through Social Services. All medications are as follows: Vanco for infection, Benadryl for itching/insomnia, Tylenol for fever, Vicodin for pain, Norco, Morphine and MS Contin for pain, Keppra and Neurontin for szr disorder, Fragmin to prevent thrombosis, MOM, Dulcolax and Colace to prevent and treat constipation. Multi-vitamin, zinc and Vitamin C for wound healing, Iron Sulfate to treat anemia. Zofran for treatment and prevention of nausea and vomiting. Protonix for GERD. DR ORDERS: 02-01-12 -AM labs: CBC c diff, BMP, The labs are drawn to monitor the patient. 01-31-12 -Morphine sulfate 2mg IV q 4 hrs PRN for pain x 72 hours, Morphine/morphine H.P/ IV/ 4-10mg q 3-4hr/opiod/ severe pain, Morphine is ordered every 72 hours. 01-30-12 -PFS for Medi-cal, The patient is to meet with financial services -SW for placement, social work for placement and insurance. 2
- 3. 01-29-12 -Vancomycin, Vancomycin/vancocin/IV/500mg q6hr or 1g q 12 hr/anti-infective/tx of potentially life-threatening sepsis -Discontinue Foley, pt can get OOB to BR 1-27-12 -Discontinue IVF, discontinue NPO status, change to reg diet, pt no longer NPO -AM labs: CBC c diff, BMP, The labs are drawn for monitoring purposes. -Add AM labs: prealbumin and CRP, The labs are drawn for monitoring purposes (inflammation process). -I&D Surgery ordered for incision and drainage with hardware removal of L ankle to assist in infection prevention and healing (EBL: 20ml) -SCD to RLE ordered post-surgery to prevent thrombosis and decubitis -PT, ordered for gait training and to promote increased L foot ROM and perform ADL’s. -AM labs c diff, CMP, The labs are drawn to monitor the patient -Morphine sulfate 2mg IV q 4 hrs PRN pain x 72 hrs, Morphine/morphine H.P/ IV/ 4-10mg q 3-4hr/opiod/ severe pain, The morphine is to be ordered every 72 hours. 01-26-12 -Hold vanco trough 23.4, The vanco level is high and too much for the kidneys. It should be held until it returns to the therapeutic range. -Please reposition pt q 2 hrs, The orders for repositioning are due to the patients decubitis ulcers -AML: CBC c diff, BMP, Mg, Phos, PT/PTT/INR -X Ray to LLE, to check results of surgery, healing process. -Renew MS Contin 30mg PO q 12 hours x 72 hours, Opioid to treat pain 01-25-12 -AML: CBC-d, BMP, Mg, Phos, Ca, The labs are necessary to monitor the patient’s blood, electrolyte and fluid levels. 01-24-12 -Change diet to NPO except meds for I & D and surgery for removal of hardware in LLE. --Pre-Op check list -Start D5NS @100cc per hour, used for maintenance of body fluid and electrolyte balance or fluid therapy before surgery. -Protonix 01-23-12 -MVI 1 tab PO q day -Vitamin C 500mg PO BID, Ascorbic acid/Mega-C,vitamin c/500 mg q day for at least 14days/vitamins/tx and prevention of vitamin deficiency. Promotes collagen synthesis -Zinc sulfate 220mg PO Q day, Zinc sulfate/zincate, zinc 220/PO/15-19mgday/mineral and electrolyte replacement/replacement and supplementation therapy. -Foley Catheter Placement: Ordered due to pt unable to ambulate, impending surgery, and to check for a ruptured bladder. -Fragmin 5000 units SubQ Daily, Anticoagulant to prevent DVT. -Zofran Inj 4mg q 8hrs, give 2 ml prn for nausea and vomiting -Morphine Sulfate 2mg IV qhs, Opioid to treat pain -MS Contin 30mg PO q 12 hours x 72 hours, Opioid to treat pain 1-22-12: -Xray CXR eval, The x-ray is performed for evaluation purposes, specifically TB, which was ruled out -AML: BMP, which is given to determine complete Ca+, Cl, Na+, CO2 levels, body electrolytes (K+), blood sugar, kidney/liver function (BUN/Cr) and hydration status, usually in patients with acute or chronic htn, DM, Vanco tx, and kidney dysfunction. CBC w/diff ordered to determine if anemia, infection, and blood loss are present. The blood CBC is standard, PT and APTT is to determine clot time. -Urinalysis and U-tox given to r/o hematuria, determine bacterial count, pH and SG. Opioids, benzos and cocaine found in pt’s system -X ray for eval of LLE, rule out fx -EKG, to r/o MI or other heart-related issues, & to determine sinus rhythm. Also a pre-op requirement to r/o cardiopulmonary dysfunction, no abnormality -Type & Screen, needed to cross-match blood products prior to surgery, in case of excessive blood loss during surgery, O-. 3
- 4. -Neurontin 300mg PO tid Anti-convulsant for tx of szr disorder. -Keppra 500mg PO q 12 hours to prevent szrs. -Colace 100mg PO prn, to prevent straining and constipation -MOM 30ml PO q 8 hrs prn, to treat and prevent constipation -Norco 10mg-325mg q 6hrs for BTP, 2 tabs -NWB LLE 1-21-12 -Vitals=PR -Activity= strict bed rest -Diet= Reg -Strict I&O per protocol -+indwelling Foley -Contact precautions, ORSA-nares -Szr precautions -Start labs: CBC c diff, CMP, PT/PTT/INR, BC, CRP, ESR -Urine culture, to detect bacteria in the urine -Urine tox, to detect drugs or alcohol in the body -Vanco 1 gm IV q 12h, Vancomycin/vancocin/IV/500mg q6hr or 1g q 12 hr/anti-infectives/tx of potentially life-threatening infection -Check Peak & Trough q 3rd dose, to prevent vanco toxicity -Protonix 40mg IV q 24 hr, Pantoprazole/protonix/IV?/ 40mg once daily for 7-10 days/proton pump for GERD inhibitors/erosive esophagitis associated w gerd -Tylenol 650mg PO q 6hr PRN pain, temp >100.4, Acetaminophen/tylenol/PO/ 325-650mg q 4-6 hr/antipyretics,non opiod analgesic/ mild pain or fever -Benedryl 25mg PO or IV q 6hrs prn for itching or insomnia Other pertinent patient information: a. Predominant stressor: (intra-, inter, extrapersonal) Intrapersonal: Worried about eventually losing his foot and future ROM. Anxiety r/t future surgery, and scared of more pain. Current continuous pain, not relieved by narcotic pain medication. Pain level was never below 6 during my care for him. Possibly drug-seeking behavior evidenced by IVDA hx, constant complaints of pain that does not match the severity of injury and asking for pain meds every time I entered his room. Interpersonal: Expressed worry and fear regarding future job prospects if his “foot doesn’t work”, and questions, “who will take care of me”. Worried about who will change his foot dressing after he gets discharged from the hospital. Expressed fear with regard to whom will administer IV anti-biotic and take care of his PICC line post-discharge. States he has a grown daughter, but only speaks with her “every couple of years. I don’t really want to talk about that.” IVDA, ETOH hx, smoker. Extrapersonal: 4
- 5. Lives “on the street” or in a hotel “sometimes, when I have enough money.” Expressed worry about stability, how long he will be in the hospital and where he will go upon discharge, as Rancho Los Amigos denied acceptance of him because he did not qualify. Verbalized fear of leaving the hospital without a wheelchair, as he “can’t afford one.” b. Variables: (physiological, psychological, spiritual, Sociocultural, developmental) Physiological Gait: Unsteady and slow d/t long leg splint and administered pain medication. Able to get OOB to wheelchair without assistance. Range of motion: active in RUE-5/5, except for LLE ROM 1/5, with limited movement. Muscle tone: Symmetrical. BLE hand grasps are strong, pulses 2+, strong and equal on all extremities, except L foot-unable to palpate d/t cast. (-) paralysis, (-) parasthesia, (-) pressure, and positive adequate perfusion, except L foot, pt states he feels moderate pressure, and some numbness. Able to wiggle fingers and toes bilaterally. Psychological: Patient is feeling groggy and in pain today d/t ATC opioid pain medication intake (as per MD), and “Kept getting woken up” and as a result, he got very little sleep. Expressed worry over at-home anti-biotic IV therapy, and who will help with his foot dressing changes after hospital d/c. Spiritual: Patient stated he was brought up Catholic and he sees the Chaplain often, satisfying his spiritual needs. Sociocultural: Patient smokes ½ ppd, and claims he quit drinking in 2008. Stated that his diet is unpredictable because he is homeless, and sometimes doesn’t know when or where he will eat. Divorced since 2000, he is unemployed and supports himself with social assistance checks. Lives on the street and/or in a hotel since his divorce. Developmental: Client is 48 years old and in Middle Adulthood according to Erikson’s developmental stages. In this stage the individual is in the stage of Generativity vs. Stagnation. If an individual has too little of Generativity (e.g. contributing to family or society) they risk stagnation. The client has been NPO intermittently, and in the hospital for 10 days, with no family contact. According to Erikson the client is most likely feeling isolated and unfulfilled, therefore leaning toward stagnation. He feels unable to be “productive or feel as if he can contribute to my own well-being with my foot the way it is.” A person that is more in the Stagnation stage has a tendency to become bored, and have a feeling of purposelessness. I have observed the patient undergoing a daily routine of showering independently, combing his hair, and brushing his teeth, which seems to bring a bit of self worth. I also observed Mr. Lopez getting himself getting to his wheelchair from bed and socializing with staff and other patients, perhaps helping him cope with isolation and establishing a sense of independence. I encouraged him to practice with his ROM exercises, showering, and fixing his hair to make him feel more purposeful. I also encouraged him to participate fully in PT to increase his chances of gaining back full ROM in his foot. I suggested he may want to practice his own dressing changes if he has a problem finding someone to do it for him, and educated him that the MD, RN and I would fully educate him prior to d/c about his anti-biotic IV therapy, and he expressed relief. Source: Lewis, Dirksen, Heitkemper, Bucher, Camera. (2011). Inflammation and wound healing. Medical-Surgical Nursing: Assessment and management of clinical problems, Volume 6 (pp. 187-203). St Louis, MO: Elsevier. Kee, J.L. (2009). Laboratory and diagnostic tests with nursing implications, Volume 6 (pp 27-400). Saddle River, NJ: Pearson. 5
- 6. Medications Med, Dose, Rte, Freq, Time Class Indication Action O, P, D Pt Teaching Labs Side Effects Fragmin LMW DVT Enhances Onset unk, Peak: 4 hrs Watch for S/S of >AST & Bleeding-epistaxis, 5000 units SQ, give Heparin/Anti- prophyla inhibition of bleeding, & avoid ALT, < Plt ecchymosis, 0.2ml Daily coag xis factor Xa & NSAIDs petechiae, bleeding thrombin by BBW: Spinal gums, anti-thrombin. hematoma & thrombocyopenia, Reduces risk neuroaxial rash, & fever. of DVT. dysfunction. BBW: Paralysis, spinal 1000 hematoma Antidote: Protamine Sulfate Keppra/Levetiracetam Anti- Szr, Slows 15-30 mins, 1.5 hrs, 7 hrs 3000 mg max >BUN/Cr, HA, infection, pain, 500mg Q 12 hrs Over Convulsant epilepsy, abnormal daily, report <H & H Anxiety, depression, 60 Mins neuropat impulses in suicidal thoughts Amnesia, increase hy the brain In szrs, cough, 0600/1800 Rhinitis, cough Protonix PPI, gastric GERD Suppresses Onset: 15-30 mins, Peak: unk, St John’s Wart >glucose HA, insomnia, 40mg IV Daily acid gastric acid Dur: 24hrs increases risk of dizziness, flu-like suppressant secretion by sunburn, don’t sndrome, inhibiting PP take with food. gastroenteritis, 1000 activity at the Report signs of vomiting, UTI & gastric bleeding arthralgia. parietal cells Morphine Sulfate Opioid, Severe Binds with Onset: < 5 mins, Peak: 20 Report continued <Plts Szrs, sedation, euphoria, 2mg IV qhs analgesic pain opioid mins, Dur: 4-5 hrs pain and hypotension, bradycardia, shick, receptors in constipation. constipation, ileus, 2200 CNS, altering Withhold if <12 thrombocytopenia, resp perception of BPM depression. Antidote: Narcan pain. 6
- 7. Gabapentin Synthetic Epilepsy Prevents & Onset: Unk, Peak: 2-4 hrs, Stop gradually due <WBCs Dizziness, ataxia, 300mg PO tid inhibitory CNS and treats szrs Dur: Unk to risk of szr, tremor, amnesia, transmitter/Ant neuralgia (unk) morphine may impotence, 1000/1400/1800 i-convulsant increase levels LEUKOPENIA, vasodilation MS Contin Opioid ModerateBinds with Onset: 10-15 mins, Peak: <1 Do not crush, take >Amylase Resp depression, 30mg PO q12hrs x 72 analgesic to severe opioid hr, Dur: 3-6 hrs with food and lipase hypotension, hrs pain receptors in sedation, urinary CNS , altering retention, vomiting. response to 2200 pain via unk mechanism Vancomycin Glycopeptide Severe Hinders Onset: Unk, Peak: Chk peak & >BUN & Red man syndrome, 30mg PO q12hrs x 72 Antibiotic Staph & bacterial cell Immediately, Dur: Unk trough, teach signs Cr, <WBCs hypotension, hrs Strep wall of infection superinfection, infections synthesis, ototoxicity, damaging the nephrotoxicity, 2200 plasma leukopenia, & membrane, thrombophlebitis killing susceptible bacteria. Zofran Inj Anti- Prevents Blocks action Unk Report HA >AST/ALT Hypotension, HA, 4mg Q 8 hrs, give 2 ml emetic/Selectiv N/V at CNS arrhythmias, rash, PRN e serotonin chemorecepto diarrhea Inhibitor r trigger zone & PNS Colace Surfactant/Em Prevents Reduces Duration of 24 to 72 hrs Teach about None Fainting, throat 100 mg PO PRN for oll-ient bowel surface dietary bulk Reported irritation, bitter taste, Constipation laxative strain tension of including bran, abd cramping, & liquid fuits & veggies. diarrhea. contents in the D/C if sever bowel. The cramping occurs. incorporation Monitor I & O. 7
- 8. of additional liquid into stool, forming a softer mass. MOM Stimulant Treats Stimulates Onset: 15-30 mins, Peak: 2-3 Monitor I & O for <K, 30ml PO q 8hrs prn Laxative and peristalsis hrs, Dur: 4-6 hrs BM & urinary < H & H, for constipation prevents retention, Monitor > Mg con- VS Q 2 hours stipation Norco Opiate/Analge Prevents Blocks action Onset: 10- Monitor RR >AST/ALT Bradychypnia 2 tabs Q6 hrs prn for sic N/V at CNS 20 mins, before & after BTP chemorecepto Dur: 3-6 administration, r trigger zone hrs monitor pain & PNS level, St. John’s Wart increases sedation, take with food Benedryl Anti- Insomnia, H1 blocker, Onset: 15 Avoid alcohol, < H & H, Plts Drowsiness, HA, insomnia, 225mg PO or IV q 6 histamine, itching prevents mins, use sunblock, tachycardia, hypotension, hrs Prn insomnia sedative histamine Peak: 1-4 increase fluids to THROMBOCYTOPENIA, related hrs, Dur: relieve dry AGRANULOCYTOSIS, anemia, responses. 6-8 hrs mouth. dry mouth, N/V, dysuria, SZR, Prevents tremor, vertigo, sedation, transmission epigastric pain & rash of nerve impulses. Relieves allergy symptoms, moton sickness & promotes sleep. Tylenol/Analgesic, Analgesic <BUN, >WBCs, Hepatic failure/toxicity, renal Anti-pyretic 650 mg Anti-pyretic monitor skin signs failure, neutropenia, leukopenia, PO p No alcohol, monitor skin Q2 hours, monitor rash, uticaria. Normal Dose: 4g signs Q2 hours, monitor I & I & O. daily. Fever NSAID O. 8
- 9. Date: 1-31-12 Vital Signs T: 98.0 BP: 126/68 HR: 88 RR: 18 SPO2: 97%- Pain: 10/10 RA Height: 5’7 Weight: 160 lbs I&O: Strict BRP Date:1-22-12 Date:1-31-12 Lab Values: Admission Current Significance of Findings Lab Test Normal Values Labs Results Specific to Patient WNL, though trending higher, possibly due to continuous IV NS administration, and intermittent NPO status. Monitor for S/S of Na 135-145 mmo/L 139 141 hypernatremia including polydipsia, edema, tachycardia, confusion, restlessness, dehydration, rough tongue, sticky mucous membranes, N/V/D,& flushed skin. Monitor I&O and daily weights x 1 and prn Trending low. Risk for low, may be r/t low vomiting. Monitor for S/S of hypochloremia including hyperreflexia, Cl 100-110 mmo/L 102 100 tetany, slow/shallow breathing & hypotension. Monitor I&O and daily weights x 1 & prn. High, monitor for S/S of alkalosis including shallow respirations, CO2 20-30 mmo/L 30 34 H apnea, cyanosis, N/V/D, irritability & muscle weakness x 1 & prn. May be caused by cocaine and heroin intake. Low upon admission, though now WNL. Indicates adequate dietary intake and kidney tissue function. At risk for high d/t, IVDA, Hep C hx. K 3.5-5.1 mmo/L 3.4 L 4.5 Monitor for S/S of hyperkalemia including oliguria, anuria, metabolic acidosis, N/V/D, & anorexia. Monitor K+ intake, I&O, blood sugar, & pH. Assess VS, I&O, K intake, plts, and daily weights x 1 & prn. High upon admission, which correlates with pt’s szr disorder & hospital- Glu 65-99 mg/dL 122 H 85 Related stress. Now WNL, Monitor for S/S of hyperglycemia including poly polyuria, polyphagia, weight-loss & Kussmaul’s breathing x 1 & prn. High, trending lower, risk for high due to Keppra & vanco intake. Test BUN 7-20 mg/dL 32 H 18 used to determine renal function & hydration status. Monitor I & O x1 & prn. Not tested Lactate 0.5-2.2 mmo/L 1.1 again WNL, test used to determine if pt has lactic acidosis. LD 90-220 U/L Not Tested WNL, indicating adequate nephron glomular function, & muscle mass. Monitor for decreased urinary output, monitor elevation in BUN/Cr labs Creatinine 0.5-1.4 mg/dL 0.80 0.81 for increase, as HCV can cause proteinuria. Also, risk for increase due to abx & Keppra intake. WNL, suggesting adequate pancreatic and kidney function, though Amylase 30-130 U/L 99 95 monitor for increase due to high AST and BUN upon admission and IVDA hx. WNL, suggesting adequate pancreatic fand kidney function, though Lipase 7-60 U/L 44 42 monitor for increase due to high AST and BUN upon admission and IVDA hx. Low, indicating low O2 in RBCs, possibly r/t Hep C, Keppra intake, Hgb 11.8-14.7 g/dL 11.8 L 11.2 L low B12 intake, low flic acid & low Fe. Monitor for S/S of anemia inclusing dizziness, weakness, dyspnea, & tachycardia Low, may be related to infection and wound surgery or antibiotics. Hct 36-44% 35.0 L 32.9 L Monitor for fatigue, pallor, tachycardia, decreased BP, and blood loss in every orifice-petecchiae, ecchymosis, hematoma, and erythema. RBC 3.7-5.2 m/cumm 3.2 3.62 Test monitors RBC count, which is low due to anemia. Low coagulation time and indicates high blood viscosity & Protime 12.2-14.1 sec potential for clotting. Monitor for S/S of thrombosis. High upon admission, though trending down to WNL. Test INR 0.92-1.1 1.22 1.18 measures blood coagulation time. Elevation may be r/t 9
- 10. anemia, inflammatory process, and antibiotic therapy. Monitor for bleeding gums, bruising, epistaxis, and hematuria High upon admission, though trending down to WNL. Test measures blood coagulation time. Elevation may be r/t APTT 24-36 42 40 anemia, cirrhosis dx, and antibiotic therapy. Monitor for bleeding gums, bruising, epistaxis, and hematuria Mg 1.7-2.3 1.8 2.0 WNL, at risk for low due to Dulcolax intake. Low upon admission, possibly d/t electrolyte increase or low protein. Anion Gap 10-17mEq/L 9L 14 S/S of decreased AG Levels are the same as alkalosis-cyanosis, N/V/D, tachycardia, <BP & confusion x 1 & prn. WNL, at risk for low due to diagnosis, and high Phos. S/S of Ca 8.5-10.3 mg/dL 9.0 9.5 hypercalcemia including lethargy, HA, weakness, muscle flaccidity, N/V/D & anorexia x 1 & prn. WNL, though rising, which occurs with normal bone healing. Monitor Phos 2.5-4.5 3.2 3.9 for S/S of hyperphosphatemia, including tetany, decreased UOP, assess for low calcium x 1 & prn. Low, possibly d/t prolonged immobilization, decreased protein intake Total Protein 6-8 g/DL 5 6 & ASA intake. S/S of low albumin include peripheral edema & ascites. Albumin 3.5-5.0 g/dL 3.7 3.8 WNL, though moni Test measures liver enzymes. An elevation can indicate liver damage. 10-40 U/L & 10-55 AST/ALT 45 H/30 23/17 AST increase may have been high d/t Hep C or Fragmin & abx U/L intake per MD order. High upon admission due to infection, now WNL with abx therapy. WBC 3.7-10.3 k/cumm 13.2 H 6.9 Monitor for S/S of infection-fever, tachycardia, increased RR, & leukocytosis). Plt 145-340 k/cumm 267 287 WNL, risk for low related to Fragmin intake. S/S of thrombocytopenia Including bleeding x 1 & prn. Vanco 5-15 20.6 HP 22.5 HP High Panic, monitor peak & trough levels q 3 rd dose to avoid toxicity. CRP Not tested >10 24 High, test detects inflammatory process, due to septic arthritis. again Urinalysis pH WNL- Adequate Metabolic acid base balance. Monitor for electrolyte 5.5-7.5 6.0 6.2 imbalance, loss or gain of acid or base, dyspnea, and decreased kidney function. Spec. Gravity WNL, indicates adequate hydration and renal function, though monitor 1.005-1.035 1.051 N/A as pt is post-surgery, which nay increase urinary retention, resulting in increased SG. Monitor I&O for dysuria & anuria. Clarity Clear Indicates pt is well-hydrated Blood WNL- No blood in urine. Monitor for hematuria, dysuria, labs for blood Neg. Neg loss, abd distension/ascities, and urine discoloration. Keytone Neg. Neg WNL, indicating adequate blood sugar levels and acid-base. Protein WNL, indicates good kidney function. Monitor for S/S of proteinutria Neg. Neg Including edema and foamy urine output. Bacteria Neg. WNL, indicating no bacteria in the urine. ABG 10
- 11. pO2 N/A O2 Sat (pulse 100% ox) pH 6.0 pCO2 N/A HCO3 N/A 11
- 12. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical N233L - ASSESSMENT Pt. Initials: J.L. Date of Assessment: 1-31-12 Vital Signs: BP 126/63 T 98.0 P 88 R 18_______Pain Level 10/10__O2 Sat 97% Neurological: Alert and oriented X 4. PRRLA. Speech status: clear and appropriate. Head: (-) lumps, (-) nodules, (-) lesions, (-) tenderness. Facial features: symmetrical, (-) facial drooping or sagging. Nose: Symmetrical. Ear assessment: auricles without deformity or tenderness, lumps or lesions, no cerumen. Eye assessment: L eye enucleation present with mild ptosis. White sclera, conjunctiva is pink/moist/intact, (-) excessive tearing, (-) swelling, (-) pain (+) prescription lenses: nearsighted. Neck/Throat: Symmetrical and has no difficulty swallowing and denies pain when swallowing, (-) palpable neck lymph nodes, no JVD. No tremors or dizziness. Cardiovascular: Skin: Warm and dry to the touch. (-) Homan’s Sign to RLE. Sensations intact, MAE except LLE. Pulse rate is 2+ in all extremities except LLE-unable to palpate due to splint. Capillary refill is less than 3 seconds on all extremities. 2+ edema noted on LLE phalanges. Apical pulse is 88 and regular, S1 and S2 heard. PICC is patent and saline-locked to L upper extremity-no drainage, redness, or swelling-PICC clean, dressing dry and intact. Respiratory: O2 Sat: 97%-room air, RR: 18-unlabored regular. Breath sounds are clear bilaterally/AP upon auscultation. Symmetrical bilateral chest expansion. Nose: Nares bilaterally patent (+)ORSA. Mucosa pink and moist, external structure without deformity, and pt can identify the smell of coffee. Oral assessment: Pink, moist and tongue is midline, no cyanosis present. (-) cough, (-) sinus tenderness. (-) Cough, sputum is clear. Gastrointestinal: Absence of N/V/D/C. Abdomen: soft with absence of tenderness or pain in all 4 abd quadrants. BS normoactive in all 4 quadrants. Reg diet: consumes between 75-100% of his meals, depending on his pain level. No chewing or swallowing problems. No masses or nodules felt, no abd distension. All teeth are present, white and healthy looking. Last BM: yesterday (1/31/12), “normal”, brown, hard consistency. Genitourinary: Voiding: Urinates spontaneously and regularly, without difficulty or pain. Into urinal. Urine is yellow in color and clear, with no odor. No pain or burning with voiding. (-) bladder distention. (-) penile discharge, per patient. Integumentary: Double lumen PICC to LUE, site and dsg clean, dry and intact, no redness, no tenderness. Nail shape WNL and smooth texture, (-) clubbing. Hair distribution: appropriate, hair pattern normal, little hair loss. Mucous membranes intact, moist and pink. Skin turgor: <2 seconds on clavicle. Skin is warm, dry, and intact all over, except. L lower anterior/posterior leg ecchymosis present and mild swelling noted on the toes. Multiple tattoos present throughout the body, (-) rash. Thick, peeling skin to dorsal bilateral feet present. Several small circular scars present throughout arms and legs. 10 incision scar present along the spine. 2 inch scar present to posterior L FA. Musculoskeletal: Gait: Unsteady and slow d/t long leg splint and administered pain medication. Able to get OOB to wheelchair without assistance. Range of motion: active in RUE-5/5, except for LLE ROM 1/5, with limited movement. Muscle tone: Symmetrical. L Bilateral hand grasps are strong, pulses 2+, strong and equal on all extremities, except L foot-unable to palpate d/t cast. (-) paralysis, (-) paresthesia, (-) pressure, with adequate perfusion, except L foot, pt states he feels moderate pressure, and some numbness. Able to wiggle fingers and toes bilaterally. Behavioral: Calm, interactive, cooperative, though mildly anxious in relation to pain and future surgery. Exhibits fear and anxiety related to where he will go upon discharge and who will take care of him. Main language is English, but speaks Spanish as well. NURSING 233L 12
- 13. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical List ALL nursing diagnosis for your patient (PRS format), and collaborative problems. Rank in order the priority problems identified. Nursing Diagnoses: 1. Ineffective bone tissue perfusion r/t the inflammation & destruction of tissue, and continuation of infectious process/delayed wound healing as manifested by Pt having elevated WBCs, tenderness & pain, 2/2 septic arthritis. 2. Risk for Peripheral neurovascular dysfunction r/t vascular insufficiency evidenced by decreased ROM and LLE edema 3. Impaired mobility r/t pain and weakness evidenced by verbal complaints of pain (when moving) and NWB status 4. Fear r/t homelessness and isolation evidenced by verbalizing “I have no where to go when I get out of here and don’t know who will take care of me.” 5. Impaired comfort r/t decreased mobility evidenced by complaints of 10/10 pain Potential Complications: -Hemorrhage and hypovolemia -Shock and CVA -Sepsis -MRSA -Cellulitis -Compartment Syndrome -Kidney failure -Falls and injury -Hemorrhage and hypovolemia -Avascular necrosis -Amputation -Loss of joint function -Neuropathy -Joint deformity -Chronic pain 13
- 14. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical 14
- 15. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION EVALUATION Subjective: P: Risk for Peripheral Goal: Pt will verbalize the 6 P’s neurovascular dysfunction of neurovascular dysfunction Goal: Met. Pt experienced no *Patient complains of pain in during my shift on 2-01-12. *Assessed pt’s knowledge new neurovascular LLE, “The pain is 10/10, Interventions: regarding neurovascular dysfunction and verbalized throbbing, and I can’t move R: R/t vascular *Assess patient’s knowledge dysfunction to LLE, which the 6 P’s. my toes”. insufficiency about neurovascular status and were WNL, except for pain *Referred from Good Sam S/S of skin irritation. and pressure. Rationale: Evaluation of pt Hospital on 1/21/12 for S: knowledge determines what to increased swelling and *Performed head to toe teach. decreased ROM. assessment. Bathed pt, & *Instruct pt to and move his changed linens. ROM of LLE *Patient has consistent complaints of pain from toes, check his skin temp & is 1/5 S/P I&D surgery. ranging from 4/10 to 9/10 pulse to his L foot tid. Rationale: To determine * Evaluated patient’s level of pain. patient’s level of ROM, improve knowledge r/t his type of *S/P L ankle joint implant tissue perfusion & circulation, disease process, pain hardware and ORIF x 5 years and prevent increased management, infection, and ago. dysfunction. possible complications. *Hx of IVDA, states, “I quit *Teach patient 6 P’s (Pain, *Taught pt the 6 P’s of drinking in 2008.” pallor, paresthesia, Objective: pulselessness, pressure, neurovascular dysfunction paralysis) related to neuro with flash cards, he dysfunction. verbalized them back. *Displays decreased ROM Rationale: Patient needs to know and weight-bearing status how to prevent and identify *Documented Assessments, *Asks for Morphine before neurovascular dysfunction. teachings and interventions the scheduled time. into Affinity. *Skin on L foot appears red, *Document assessment, teachings and interventions with 1 + edema, ROM: 1/5 Chart Assessment in Affinity in *Smoker, delayed wound the computer. healing & vasoconstriction Rationale: This is done to ensure Related Labs 01/31/12: communication with other healthcare providers, informing --Glu: 122 H them of interventions, to assist --Hct: 32.9 L in further care of patient. Also, done in compliance with --Hgb: 12.2 L hospital protocol and state law. --WBCs: 6.7 N --CRP: 24 15
- 16. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical -VS on 01/31/12 BP: 126/68 HR: 88 O2 Sat: 97 % room air ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION EVALUATION 16
- 17. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical Goal: SUBJECTIVE: P: Fear Patient will identify & *Assessed level of anxiety (8 Goal: Met. Patient verbalized demonstrate 1 guided out of 10) and provided reduced anxiety, and *Pt stated “I have no where R: R/t homelessness and imagery technique reassurance that the social worker would do her best to find practiced guided imagery, via to go when I get out of here isolation (visualization with other “walking on the beach” placement for him. and don’t know who will take sensory attributes) by 1500 Pt Response: Stated that he was during an episode of anxiety. care of me.” on 8/22/12. relieved. Outcome met. S: Evidenced by verbalizing “I have no where to go when INTERVENTION: I get out of here and don’t *Assess level of knowledge *Identified current coping know who will take care of regarding guided imagery & behaviors (smoking and Identify current coping diversionary), gave him a me.” smoking cessation pamphlet and behaviors. Rationale: To establish a taught adaptive coping baseline and level of care mechanism-guided imagery. Pt Response: Has smoked for needed. over 30 years, ahs tried to quit * Rationale: To learn how to twice “cold turkey”, but OBJECTIVE: better manage stress and fear. eventually started again. *Absence of love ones at Also enhances personal bedside confidence. *Taught pt to shut his eyes, * Teach adaptive coping breathe deeply and practiced mechanism-guided imagery. guided imagery techniques *Displays facial grimacing Rationale: To promote self- Pt Response: Pt imagined he intermittently control and independence was lying on the beach and *Provide a safe, calm, quiet breathing deeply while he imagined waves. He stated that *Homeless, divorced and environment, keep lights low. it was calming, but he didn’t unemployed Restrict caffeine. know if it was enough to make Rationale: To reduce anxiety. him not want to smoke, but it did * Document assessments, help with the anxiety he was *Denied placement from teachings and interventions feeling Rancho into Chart Assessment in Affinity . *Provided a safe, calm, quiet Rationale: To ensure environment, with low lighting *Goes off ward to smoke and a soft voice. Restrict communication with other caffeine. Fall and szr healthcare providers, precautions were enforced. informing them of further care of patient. *Documented assessments, teachings and interventions Chart Assessment in Affinity R: This is done to ensure communication with other healthcare providers, informing them of interventions, to assist in further care of patient. Also, 17
- 18. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical done in compliance with hospital protocol and state law ASSESSMENT DIAGNOSIS PLANNING IMPLEMENTATION EVALUATION 18
- 19. LAC School of Nursing N233L – Intermediate Medical Surgical & Psychiatric Nursing Clinical Objective: PC : Septicemia r/t infection in Intervention with rationale Goal: Including patient response *Osteomyelitis and IVDA hx the left foot * Assess knowledge of signs and Met. The patient was able to symptoms of Septicemia (fever, * Pt Response: “I just know about the bone infection, and correctly verbalize greater chills rapid heart rate, malaise, understanding of sepsis and *Smoker half ppd altered mental status), and that if it gets worse, they might more that two S/S. determine pt’s preferred learning cut off my foot”, “I just have style. pain and pressure.” *Male in his 40’s Rationale: So I will know what “I learn best with pictures or to teach regarding septicemia reading.” and teach in pt’s preferred *Status post L ankle ORIF learning style so he may better with hardware x 5 yrs ago learn. *Pt Response: Verbalized that septicemia was “an infection Goal: * Educate the patient the S/S of that spreads to the blood” and *Increased WBCs upon Will monitor, along with other Sepsis and express the stated that s/s are fever chills admission healthcare providers, the S/S of importance of early and confusion. septicemia. identification and intervention. Rationale: Pt will be able to *Increased CRP @ 24 quickly identify the early S/S * Pt Response: “I will sing the and report them to prevent this Happy Birthday song twice *HR: 88 complication. when I wash my hands.” * Educate on infection * Pt Response: “I will call you Subjective: prevention techniques including when my pain is more than 4 out *”I came in because I was in proper hand-washing, & keeping dsg clean and dry @ all times. of 10.” pain and swollen” *Teach to use pain scale and to *”I’ve had Osteomyelitis call for pain meds before pain before” reaches 4/10, as ordered. Taught S/S of infection, and encouraged using PT for long-term pain reduction & increased ROM. Pt verbalized signs of infection. * Document teachings into Affinity Rationale: To ensure communication with other healthcare providers. 19
