17 gi
- 1. GI
- 2. GI • ESOPHAGUS • STOMACH • SMALL/LARGE BOWEL • APPENDIX, PERITONEUM
- 3. ESOPHAGUS • Congenital Anomalies • Achalasia • Hiatal Hernia • Diverticula • Laceration • Varices • Reflux • Barretts • Esophagitis • Neoplasm: Benign, Sq. Cell Ca., Adenoca.
- 4. ANATOMY • 25 cm. • UES/LES • Mucosa/Submucosa/Muscularis/Adventitia
- 5. Inf. Thyroid Arts. R. Bronch. Art. Thoracic. Aor. Left Gastric Art. Variations: Inf, Phrenic Celiac Splenic Short Gast.
- 7. DEFINITIONS • Heartburn (GERD/Reflux) • Dysphagia • Hematemesis • Esophagospasm (Achalasia)
- 8. CONGENITAL ANOMALIES • ECTOPIC TISSUE (gastric, sebaceous, pancreatic) • Atresia/Fistula/Stenosis/”Webs” • Schiatzke “Ring” MOST COMMON
- 9. MOTOR DISORDERS • Achalasia • Hiatal Hernia (sliding [95%], paraesophageal) • “ZENKER” diverticulum • Esophagophrenic diverticulum • Mallory-Weiss tear
- 11. ACHALASIA • “Failure to relax” – Aperistalsis – Incomplete relaxation of the LES – Increased LES tone • INCREASE: Gastrin, serotonin, acetylcholine, Prostaglandin F2α, motulin, Substance P, histamine, pancreatic polypeptide • DECREASE: NO, VIP – Progressive dysphagia starting in teens –Mostly UNCERTAIN etiology
- 12. HIATAL HERNIA • Diaphragmatic muscular defect • WIDENING of the space which the lower esophagus passes through • IN ALL cases, STOMACH above diaphragm • Usually associated with reflux • Very common Increases with age • Ulceration, bleeding, perforation, strangulation
- 15. DIVERTICULA •ZENKER (HIGH) •TRACTION (MID) •EPIPHRENIC (LOW) •TRUE vs. FALSE?
- 16. DIVERTICULUM
- 17. LACERATION • Tears are LONGITUDINAL • Usually secondary to severe VOMITING • Usually in ALCOHOLICS • Usually MUCOSAL tears • By convention, they are all called: MALLORY-WEISS
- 19. VARICES • THREE common areas of portal/caval anastomoses –Esophageal – Umbilical – Hemorrhoidal • 100% related to portal hypertension • Found in 90% of cirrhotics • MASSIVE, SUDDEN, FATAL hemorrhage is the most feared consequence
- 20. VARICES
- 21. VARICES
- 22. ESOPHAGITIS •GERD/Reflux Barrett’s • Barrett’s •Chemical •Infectious
- 23. REFLUX/GERD • DECREASED LES tone • Hiatal Hernia • Slowed reflux clearing • Delayed gastric emptying • REDUCED reparative ability of gastric mucosa
- 24. REFLUX/GERD • Inflammatory Cells –Eosinophils –Neutrophils –Lymphocytes • Basal zone hyperplasia • Lamina Propria papillae elongated and congested
- 25. REFLUX/GERD
- 26. BARRETT’S ESOPHAGUS • Can be defined as intestinal metaplasia of a normally SQUAMOUS esophageal mucosa. The presence of GOBLET CELLS in the esophageal mucosa is DIAGNOSTIC. • SINGLE most common RISK FACTOR for esophageal adenocarcinoma • 10% of GERD patients get it • “BREACHED” G-E junction
- 29. BARRETT’S ESOPHAGUS • INTESTINALIZED (GASTRICIZED) mucosa is AT RISK for glandular dysplasia. • Searching for dysplasia when BARRETT’s is present is of utmost importance • MOST/ALL adenocarcinomas arising in the esophagus arise from previously existing BARRETT’s
- 31. ESOPHAGITIS • CHEMICAL – LYE (suicide attempts) with strictures – Alcohol – Extremely HOT drinks –CHEMO • INFECTIOUS – HSV, CMV, Fungal (especially CANDIDA)
- 32. ESOPHAGITIS
- 33. ESOPHAGITIS
- 34. TUMORS • BENIGN • MALIGNANT –Squamous cell carcinoma –Adenocarcinoma
- 35. BENIGN TUMORS • LEIOMYOMAS • FIBROVASCULAR POLYPS • CONDYLOMAS (HPV) • LIPOMAS • “GRANULATION” TISSUE (PSEUDOTUMOR)
- 36. SQUAMOUS CARCINOMA • Nitrites/Nitrosamines • Betel • Fungi in food • Tobacco • Alcohol • Esophagitis?
- 37. SQUAMOUS CARCINOMA • DYSPLASIAIN-SITUINFILTRATION
- 41. ADENOCARCINOMA • BARRETT’s • BARRETT’s • BARRETT’s • BARRETT’s • BARRETT’s • BARRETT’s • BARRETT’s • (heterotopic gastric or submucal glands)
- 42. ADENOCARCINOMA
- 44. STOMACH NORMAL: Anat., Histo, Physio. PATHOLOGY CONGENITAL GASTRITIS PEPTIC ULCER “HYPERTROPHIC” GASTRITIS VARICES TUMORS BENIGN ADENOCARCINOMA OTHERS
- 45. ANATOMY Cardia, Fundus, Body, Antrum, Pylorus Greater/Lesser Curvatures 1500-3000 ml Rugae INNERVATION: VAGUS, Sympathetic VEINS: Portal Blood Supply: RG, LG, RGE(O), LGE(O), SG, ALL 3 branches of the celiac
- 51. CELLS MUCOUS: MUCUS, PEPSINOGEN II CHIEF: PEPSINOGEN I, II PARIETAL: ACID ENTEROENDOCRINE: HISTAMINE, SOMATOSTATIN, ENDOTHELIN
- 52. PHYSIOLOGY PHASES CEPHALIC (VAGAL) GASTRIC (STRETCH) INTESTINAL (DUOD)
- 53. ACID PROTECTION MUCUS HCO3- EPITHELIAL BARRIERS BLOOD FLOW PROSTAGLANDIN E, I
- 54. CONGENITAL • ECTOPIC PANCREAS (ectopic pancreas tissue stomach), very common • ECTOPIC GASTRIC (ectopic gastric tissue pancreas), not rare • Diaphragmatic HERNIA Failure of diaphragm to close, not rare • PULMONARY SEQUESTER (rare) • …..and the #1 congenitnal gastric disease
- 55. PYLORIC STENOSIS • CONGENITAL: (1/500), Neonatal obstruction symptoms, pyloric splitting curative • ACQUIRED: Secondary to extensive scarring such as advanced peptic ulcer disease
- 56. GASTRITIS • ACUTE • CHRONIC • AUTOIMMUNE • OTHER – EOSINOPHILIC – ALLERGIC – LYMPHOCYTIC –GRANULOMATOUS –GVH
- 57. GASTRITIS • ACUTE, HEMORRHAGIC • (NSAIDs), particularly aspirin • Excessive alcohol consumption • Heavy smoking • CHEMO • Uremia • Salmonella, CMV • Severe stress (e.g., trauma, burns, surgery) • Ischemia and shock • Suicidal attempts, as with acids and alkali • Gastric irradiation or freezing • Mechanical (e.g., nasogastric intubation) • Distal gastrectomy
- 58. GASTRITIS • ACUTE, HEMORRHAGIC • HISTOLOGY: Erosion, Hemorrage, NEUTROPHILS
- 59. GASTRITIS • CHRONIC, NO EROSIONS, NO HEMORRHAGE • Chronic infection by H. pylori • Immunologic (autoimmune), e.g., PA • Toxic, as with alcohol and cigarette smoking • Postsurgical, reflux of bile • Motor and mechanical, including obstruction, bezoars (luminal concretions), and gastric atony • Radiation • Granulomatous conditions (e.g., Crohn disease) • GVH, uremia
- 60. GASTRITIS • CHRONIC, NO EROSIONS, NO HEMORRHAGE • Perhaps some neutrophils • Lymphocytes, lymphoid follicles • REGENERATIVE CHANGES – METAPLASIA, intestinal – ATROPHY, mucosal hypoplasia, “thinning” – DYS-PLASIA
- 62. GASTRITIS •AUTOIMMUNE (10%) • ANTIBODIES AGAINST –acidproducing enzyme H+ –K+ -ATPase –gastrin receptor –and intrinsic factor
- 63. GASTRITIS • OTHER – EOSINOPHILIC, middle aged women – ALLERGIC, children (also eosinophils) – LYMPHOCYTIC, T-Cells, body, DIFFUSE – GRANULOMATOUS, Crohn’s, other granulomas – GVH, in bone marrow transplants
- 65. “PEPTIC” ULCERS • “PEPTIC” implies acid cause/aggravation • ULCER vs. EROSION (muscularis mucosa intact) • MUCSUBMUCMUSCULARISSEROSA • Chronic, solitary (usually), adults • 80% caused by H. pylori • 100% caused by H. pylori in duodenum • NSAIDS “STRESS”
- 66. Helicobacter pylori • Causes 80% of gastric peptic ulcers • Causes 100% of duodenal peptic ulcers • Causes chronic gastritis • Causes gastric carcinomas • Causes MALT lymphomas
- 67. “PEPTIC” ULCERS • Gnawing, burning, aching pain • Fe deficiency anemia • Acute hemorrhage • Penetration, perforation: – Pain in BACK – Pain in CHEST – Pain in LUQ •NOTfelt to develop into malignancy
- 68. • Bleeding “PEPTIC” ULCERS – Occurs in 15% to 20% of patients – Most frequent complication – May be life-threatening – Accounts for 25% of ulcer deaths – May be the first indication of an ulcer • Perforation – Occurs in about 5% of patients – Accounts for two thirds of ulcer deaths – Rarely, is the first indication of an ulcer • Obstruction from edema or scarring – Occurs in about 2% of patients – Most often due to pyloric channel ulcers – May also occur with duodenal ulcers – Causes incapacitating, crampy abdominal pain – Rarely, may lead to total obstruction with intractable vomiting
- 69. “ACUTE” ULCERS • NSAIDS • “STRESS” ULCERS –ENDOGENOUS STEROIDS • SHOCK • BURNS • MASSIVE TRAUMA • Intracranial trauma, Intracranial surgery • SEPSIS – EXOGENOUS STEROIDS • CUSHING ULCER
- 70. “ACUTE” ULCERS • Usually small (<1cm), superficial, MULTIPLE
- 71. GASTRIC DILATATION • PYLORIC STENOSIS • PERITONITIS ( pyloric stenosis) • 1.5-3.0 liters NORMAL • 10 liters can be present • ACUTE RUPTURE is associated with an immediate HIGH mortality rate
- 72. BEZOARS • PHYTO-bezoar (plant material) • TRICHO-bezoar (hairball) • NON-food material in PSYCH patients – pins – nails – razor blades – coins – gloves – leather wallets
- 74. “HYPERTROPHIC” GASTROPATHY RUGAL PROMINENCE (cerebriform) NO INFLAMMATION HYPERPLASIA of MUCOSA
- 75. “HYPERTROPHIC” GASTROPATHY • Inaccurate name “hypertrophic gastritis” • Ménétrier disease, resulting from profound hyperplasia of the surface mucous cells with accompanying glandular atrophy • Hypertrophic-hypersecretory gastropathy, associated with hyperplasia of the parietal and chief cells within gastric glands • Gastric gland hyperplasia secondary to excessive gastrin secretion, in the setting of a gastrinoma (Zollinger-Ellison syndrome)
- 77. GASTRIC “VARICES” • SAME SETTING AND ETIOLOGY AS ESOPHAGEAL VARICES, i.e., PORTAL HYPERTENSION • NOT AS COMMON AS ESOPHAGEAL VARICES • MAY LOOK LIKE RUGAE • IF A PATIENT HAS GASTRIC VARICES, HE ALSO PROBABLY HAS ESOPHAGEAL
- 78. GASTRIC TUMORS • BENIGN: – POLYPS (HYPERPLASTIC vs. ADENOMATOUS) – LEIOMYOMAS (Same gross and micro as sm. muscle) – LIPOMAS (Same gross and micro as adipose tissue) • MALIGNANT – (ADENO)Carcinoma – LYMPHOMA • POTENTIALLY MALIGNANT – G.I.S.T. (Gastro-Intestinal Stromal Tumor) – CARCINOID (NEUROENDOCRINE)
- 79. BENIGN TUMORS BEBNIBGNB MUCOSA (POLYPS) ---HYPERPLASTIC ---Fundic ---Peutz-Jaeger ---Juvenile ---ADENOMATOUS MUSCLE FAT
- 80. MBAEBLNIIBGG.N BTUMORS MUCOSA LYMPHS (MUSCLE) (FAT)
- 81. WHO GASTRIC NEOPLASMS • Epithelial Tumors: Adenomatous polyps, Adenocarcinoma (papillary, tubular, mucinous, signet ring, adenosquamous, unclassified), Small cell, Carcinoid (neuroendocrine) • Nonepithelial Tumors: Leiomyo(sarc)oma, Schwannoma, GIST, Granular Cell Tumor, Kaposi sarcoma • Malignant Lymphomas:
- 82. ADENOCARCINOMA • H. pylori associated, MASSIVELY!!! • Japan, Chile, Costa Rica, Colombia, China, Portugal, Russia, and Bulgaria • M>>F • Socioeconomically related
- 83. ADENOCARCINOMA RISK FACTORS • H. pylori • H. pylori • H. Pylori • Nitrites, smoked meats, pickled, salted, chili peppers, socioeconomic, tobacco • Chronic gastritis, Barrett’s, adenomas • Family history
- 86. PAPILLARY
- 87. TUBULAR
- 88. MUCINOUS
- 89. SIGNET RING
- 90. ADENOSQUAMOUS
- 91. G.I.S.T. TUMORS • Can behave and/or look benign or malignant • Usually look like smooth muscle, i.e., “stroma” • Are usually POSITIVE for c-KIT (CD117), i.e., express this antigen on immunochemical staining, the tumor cells are derived from the interstitial cells, of Cajal, a “neural” type of cell.
- 92. SMALL/LARGE INTESTINE • NORMAL: Anat., Vasc., Mucosa, Endocr., Immune, Neuromuscular. • PATHOLOGY: – CONGENITAL – ENTEROCOLITIS: DIARRHEA, INFECTIOUS, OTHER – MALABSORPTION: INTRALUMINAL, CELL SURFACE, INTRACELL. – (I)IBD: CROHN DISEASE and ULCERATIVE COLITIS – VASCULAR: ISCHEMIC, ANGIODYSPLASIA, HEMORRHAGIC – DIVERTICULOSIS/-IT IS – OBSTRUCTION: MECHANICAL, PARALYTIC (ILEUS) (PSEUDO) – TUMORS: BENIGN, MALIGNANT, EPITHELIAL, STROMAL
- 93. ANATOMY • SI = 6 meters, LI = 1.5 meters • Mucosa, submucosa, muscularis, serosa/adv.
- 94. BLOOD SUPPLY • SI: SMA Jejunal, Ileal • LI: SMA, IMA Ileocolic, R, M, L, colic, Sup. Rect • RECTUM: Superior, Middle, Inferior • SMA has anastomoses with CELIAC (pancreatoduodenal), IMA (marginal)
- 95. MUCOSA • SI: ABSORPTIVE, MUCUS, PANETH (apical granules) – VILLI • LI: MUCUS, ABSORPTIVE, ENTEROENDOCRINE (basal granules) – CRYPTS
- 97. ENTEROENDOCRINE • SECRETORY PEPTIDES • Endocrine, Paracrine, Neurocrine • Chemical messengers • Regulate digestive functions • Serotonin, somatostatin, motilin, cholecystokinin, gastric inhibitory peptide, neurotensin, vasoactive inhibitory peptide (VIP), neuropeptide, enteroglucagon
- 98. IMMUNE SYSTEM • MALT • PEYER PATCHES, mucosa, submucosa, 1˚, 2 ˚ • IgGAMDE
- 99. NEUROMUSCULAR • AUTONOMIC (VAGUS, Symp.)-----extrinsic • INTRINSIC – Meissner (submucosa) – Auerbach (between circular and longitudinal)
- 100. CONGENITAL • DUPLICATION • MALROTATION • OMPHALOCELE • GASTROSCHISIS • ATRESIA/STENOSIS SPECTRUM • MECKEL (terminal ileum, “vitelline” duct) • AGANGLIONIC MEGACOLON (HIRSCHSPRUNG DISEASE)
- 102. ENTEROCOLITIS • DEFINITION of diarrhea: INCREASE in MASS, FLUIDITY, FREQUENCY • DIARRHEA: SECRETORY, OSMOTIC, EXUDATIVE, MALABSORPTION, MOTILITY – INFECTIOUS (Viral, Bacterial, Parasitic) – NECROTIZING – COLLAGENOUS – LYMPHOCYTIC – AIDS – After BMT – DRUG INDUCED – RADIATION – “SOLITARY” RECTAL ULCER
- 103. SECRETORY DIARRHEA • Viral damage to mucosal epithelium • Entero toxins, bacterial • Tumors secreting GI hormones • Excessive laxatives
- 104. OSMOTIC DIARRHEA • Disaccharidase deficiencies • Bowel preps • Antacids, e.g., MgSO4
- 105. EXUDATIVE DIARRHEA • BACTERIAL DAMAGE to GI MUCOSA • IBD • TYPHLITIS (immunosuppression colitis)
- 106. MALABSORPTION DIARRHEA • INTRALUMINAL • MUCOSAL CELL SURFACE • MUCOSAL CELL FUNCTION • LYMPHATIC OBSTRUCTION • REDUCED FUNCTIONING BOWEL SURFACE AREA
- 107. MOTILITY DIARRHEA • DECREASED TRANSIT TIME – Reduced gut length – Neural, hyperthyroid, diabetic – Carcinoid syndrome • INCREASED TRANSIT TIME – Diverticula – Blind loops – Bacterial overgrowth
- 108. INFECTIOUS enterocolitis • VIRAL – Rotavirus (69%), Calciviruses, Norwalk-like, Sapporo-like, Enteric adenoviruses, Astroviruses • BACTERIAL – E. coli, Salmonella, Shigella, Campylobacter, Yersinia, Vibrio, Clostridium difficile, Clostridium perfringens, TB – Bacterial “overgrowth” • PARASITIC – Ascaris, Strongyloides, Necator, Enterobius, Tricuris – Diphyllobothrium, Taenia, Hymenolepsis – Amebiasis (Entamoeba histolytica) – Giardia
- 109. VIRAL enterocolitis • Rotavirus most common, by far –Selectively infects and destroys mature enterocytes in the small intestine –Crypts spared • Most have a 3-5 day course • Person to person, food, water
- 110. BACTERIAL enterocolitis • Ingestion of bacterial toxins – Staph – Vibrio – Clostridium • Ingestion of bacteria which produce toxins – Montezuma’s revenge (traveller’s diarrhea), E.coli • Infection by enteroinvasive bacteria – Enteroinvasive E. coli (EIEC) – Shigella – Clostridium difficile
- 111. E. coli • Toxin, invasion, many subtypes • Food, water, person-to-person • Usually watery, some hemorrhagic • INFANTS often
- 112. SALMONELLA Food, not hemorrhagic SHIGELLA (person-to-person, invasive, i.e., often hemorrhagic)
- 113. CAMPLYOBACTER • Toxins, Invasion • Food spread
- 114. YERSINIA (enterocolitica) • Food • Invasion • LYMPHOID REACTION
- 115. VIBRIO cholerae • Water, fish, person-to-person • Cholera epidemics • NO invasion (watery) • ENTEROTOXIN
- 116. CLOSTRIDIUM DIFFICILE • CYTOTOXIN (lab test readily available) • NOSOCOMIAL • PSEUDOMEMBRANOUS (ANTIBIOTIC ASSOCIATED) COLITIS
- 117. BACTERIAL OVERGROWTH SYNDROME • One of the main reasons why “normal” gut flora is NOT usually pathogenic, is because, they are constantly cleared by a NORMAL transit time • BLIND LOOPS • DIVERTICULA • OBSTRUCTION • Bowel PARALYSIS
- 118. PARASITES • NEMATODES (ROUNDWORMS) – Ascaris, Strongyloides, Hookworms (Necator & Anklyostoma), Enterobius, Trichuris • CESTODES (TAPEWORMS) – FISH (DIPHYLLOBOTHRIUM latum) – PORK (TAENIA solium) – DWARF (HYMENOLEPSIS nana) • AMOEBA (ENTAMOEBA histolytica), Giardia lamblia
- 120. GIARDIA LAMBLIA
- 121. MISC. COLITIS (OTHER) • NECROTIZING ENTEROCOLITIS (neonate) (Cause unclear) • COLLAGENOUS (Cause unclear) • LYMPHOCYTIC (Cause unclear) • AIDS • GVHD after BMT, as in stomach • DRUGS (NSAIDS, etc., etc., etc.) • RADIATION • NEUTROPENIC (TYPHLITIS), (cecal) • DIVERSION (like overgrowth) • “SOLITARY” RECTAL ULCER (anterior, motor dysfunction)
- 122. MALABSORPTION • INTRALUMINAL • BRUSH BORDER • (TRANS)EPITHELIAL • OTHER – REDUCED MUCOSAL AREA: Celiac, CD – LYMPHATIC OBSTRUCTION: Lymphoma, TB – INFECTION – IATROGENIC: Surgical
- 123. INTRALUMINAL • PANCREATIC • DEFECTIVE/REDUCED BILE • BACTERIAL OVERGROWTH
- 124. BRUSH BORDER • DISACCHARIDASE DEFICIENCY • BRUSH BORDER DAMAGE, e.g., by bacteria
- 125. (Trans)EPITHELIAL • ABETALIPOPROTEINEMIA • BILE ACID TRANSPORTATION DEFECTS
- 126. CELIAC DISEASE • Also called SPRUE • Also called NON-tropical SPRUE • Also called GLUTEN-SENSITIVE ENTEROPATHY – Sensitivity to GLUTEN, a wheat protein, gliadin – Immobilizes T-cells – Also in oat, barley, rye – Progressive mucosal “atrophy”, i.e. villous flattening – Relieved by gluten withdrawal
- 127. CELIAC DISEASE
- 128. “TROPICAL” SPRUE • Epidemic forms • NOT related to gluten • RECOVERY with antibiotics
- 129. WHIPPLE’s DISEASE • DISTENDED MACROPHAGES in the LAMINA PROPRIA • PAS positive • ROD SHAPED BACILLI
- 130. WHIPPLE’s DISEASE
- 131. DISACCHARIDASE DEFICIENCY • LACTASE by far MOST COMMON • ACQUIRED, NOT CONGENITAL • LACTOSE GLUCOSE + GALACTOSE • LACTOSE (fermented)XXXXXXXXX • OSMOTIC DIARRHEA
- 132. ABETALIPOPROTEINEMIA • Autosomal recessive • Rare • Inability to make chylomicrons from FFAs and MONOGLYCERIDES • Infant failure to thrive, diarrhea, steatorrhea
- 133. (I) IBD • CROHN DISEASE (granulomatous colitis) • ULCERATIVE COLITIS
- 134. (I) IBD • COMMON FEATURES –IDIOPATHIC –DEVELOPED COUNTRIES –COLONIC INFLAMMATION –SIMILAR Rx –BOTH have CANCER RISK
- 135. (I) IBD DIFFERENCES • CROHN (CD) – TRANSMURAL, THICK WALL – NOT LIMITED to COLON – GRANULOMAS – FISTULAE COMMON – TERMINAL ILEUM OFTEN – SKIP AREAS – “CRYPT” ABSCESSES NOT COMMON – NO PSEUDOPOLYPS – MALABSORPTION • ULCERATIVE (UC) – MUCOSAL, THICK MUCOSA – LIMITED to COLON – NO GRANULOMAS – FISTULAE RARE – TERMINAL ILEUM NEVER – NO SKIP AREAS – “CRYPT” ABSCESSES COMMON – PSEUDOPOLYPS – NO MALABSORPTION
- 136. CROHN vs. UC
- 137. UC or CD?
- 138. VASCULAR DISEASES • ISCHEMIA/INFARCTION • ANGIO-”DYSPLASIA”* •HEMORRHOIDS
- 139. ISCHEMIA/INFARCTION • HEMORRHAGE is the main HALLMARK of ischemic bowel disease – ARTERIAL THROMBUS – ARTERIAL EMBOLISM – VENOUS THROMBUS – CHF, SHOCK – INFILTRATIVE, MECHANICAL MUCOSAL TRANSMURAL
- 141. ANGIODYSPLASIA • NOT really “dysplasia” • NOT neoplastic • TWISTED, DILATED SUBMUCOSAL VESSELS, can rupture! • Common X-ray finding
- 142. HEMORRHOIDS • INCREASED INTRABDOMINAL PRESSURE • i.e., VALSALVA • INTERNAL vs. EXTERNAL
- 143. DIVERTICULOSIS/-ITIS • FULL THICKNESS BOWEL OUTPOCKETING • Assoc. w.: – INCREASED LUMINAL PRESSURE –AGE – LR – FIBER – Weakening of wall
- 144. DIVERTICULOSIS/-IT IS (CLINICAL) • IMPACT • INFLAME (“appendicitis” syndrome) • PERFORATE Peritonitis, local, diffuse • BLEED, silently, even fatally • OBSTRUCT • EXTREMELY EXTREMELY COMMON • NOT assoc w. neoplasm
- 145. Formation of colonic diverticuli • The most commonly known colonic diverticuli are pseudo diverticuli – composed of only mucosa on the luminal side and serosa externally. Why are these called “pseudo” or false? • Diverticuli resemble hernias of the colonic wall in that they occur @ sites of entry of mucosal arteries as they pass through the muscularis – this represents a weak spot that leads to a diverticulum if the individual generates high colonic intraluminal pressure (low fiber diet)
- 146. DIVERTICULOSIS
- 147. DIVERTICULITIS
- 148. DIVERTICULITIS
- 149. OBSTRUCTION • ANATOMY – ADHESIONS (post-surgical) – IMPACTION – HERNIAS – VOLVULUS – INTUSSUSCEPTION – TUMORS – INFLAMMATION, such as IBD (Crohn) or divertics – STRICTURES/ATRESIAS – STONES, FECALITHS, FOREIGN BODIES – CONGENITAL BANDS, MECOMIUM, INPERF. ANUS
- 150. OBSTRUCTION
- 151. OBSTRUCTION • PHYSIOLOGY – ILEUS, esp. postsurgical – INFARCTION – MOTILITY DISEASES, esp., HIRSCHSPRUNG DISEASE
- 152. TUMORS • NON-NEOPLASTIC (POLYPS) • EPITHELIAL • MESENCHYMAL (STROMAL) • LYMPHOID • BENIGN • MALIGNANT
- 154. POLYPS • ANY mucosal bulging, blebbing, or bump •HYPERPLASTIC(NON-NEOPLASTIC) • HAMARTOMATOUS (NON-NEOPLASTIC) •ADENOMATOUS(TRUE NEOPLASM, and regarded by many as PRE-MALIGNANT as well) • SESSILE vs. PEDUNCULATED • TUBULAR vs. VILLOUS
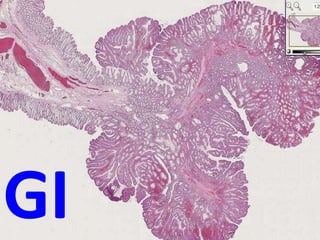
- 155. POLYPS
- 156. PEDUNCULATED vs VILLOUS vs SESSILE
- 157. BENIGN vs. MALIGNANT • Usual, atypia, pleo-, hyper-, mitoses, etc. • Stalk Invasion
- 158. HPERPLASTIC POLYP
- 161. “FAMILIAL” NEOPLASMS • POLYPOSIS (NON-NEOPLASTIC, hamartomatous) • POLYPOSIS (NEOPLASTIC, i.e., cancer risk) • HNPCC: (Hereditary Non Polyposis Colorectal Cancer)
- 162. CANCER GENETICS • Loss of APC gene • Mutation of K-RAS • Loss of SMADs (regulate transcription) • Loss of p53 • Activation of TELOMERASE
- 163. CANCER RISK FACTORS • Family history • Age (rare <50) • LOW fiber, HIGH meat, LOW transit time, refined carbs
- 164. PATHOGENESIS • From existing ADENOMATOUS POLYPS • DE-NOVO • DYSPLASIAINFILTRATIONMETASTASIS
- 165. GROWTH PATTERNS • POLYPOID • ANNULAR, CONSTRICTING • DIFFUSE
- 167. PAPILLARY
- 168. TUBULAR
- 169. MUCINOUS
- 170. SIGNET RING
- 171. ADENOSQUAMOUS
- 172. Tumor Stage Histologic Features of the Neoplasm Tis Carcinoma in situ (high-grade dysplasia) or intramucosal carcinoma (lamina propria invasion) T1 Tumor invades submucosa T2 Extending into the muscularis propria but not penetrating through it T3 Penetrating through the muscularis propria into subserosa T4 Tumor directly invades other organs or structures Nx Regional lymph nodes cannot be assessed N0 No regional lymph node metastasis N1 Metastasis in 1 to 3 lymph nodes N2 Metastasis in 4 or more lymph nodes Mx Distant metastasis cannot be assessed M0 No distant metastasis M1 Distant metastasis
- 173. OTHER TUMORS • CARCINOID, with or without syndrome • LYMPHOMA (MALTOMAS, B-Cell) • LEIOMYOMA/-SARCOMA • LIPOMA/-SARCOMA
- 174. ANAL CANAL CARCINOMAS • MORE LIKELY TO BE SQUAMOUS, or “basaloid” • WORSE IN PROGNOSIS • HPV RELATED
- 175. A P P E N D I X
- 176. ANATOMY • Junction of 3 tenia coli, variable in location • All 4 layers, true serosa • Thickest layer is submucosal lymphoid tissue • APPENDICITIS (ACUTE) • MUCOCELE • MUCUS CYSTADENOMA • MUCUS CYSTADENOCARCINOMA
- 177. ACUTE APPENDICITIS • GENERALLY, a disease of YOUNGER people • OBSTRUCTION by FECALITH the classic cause but fecaliths present only about half the time • EARLY APPENDICITIS: NEUTROPHILSMucosa, submucosa • NEED NEUTROPHILS in the MUSCULARIS to confirm the DIAGNOSIS • 25% normal rate, usually • Perforationperitonitis the rule, if no surgery
- 178. ACUTE APPENDICITIS
- 180. Mucus “TUMORS” • Mucocele (common) • Mucinous Cystadenoma (rather rare) • Mucinous Cystadenocarcinoma (rare)
- 181. MUCOCELE • COMMON CYST on APPENDIX filled with MUCIN • Can RUPTURE to become: PSEUDOMYXOMA PERITONEII
- 183. MUCINOUS CYSTADENO(CARCINO)MA ADENOMA CARCINOMA
- 184. PERITONEUM • Visceral, Parietal: all lined by mesothelium • Peritonitis, acute: – Appendicitis, local or with rupture – Peptic ulcer, local or ruptured – Cholecystitis, local or ruptured – Diverticulitis, local or with rupture – Salpingitis gonococcal or chlamydial – Ruptured bowel due to any reason – Perforating abdominal wall injuries
- 185. PERITONITIS • E. coli • STREP • S. aureus • ENTEROCOCCUS
- 186. PERITONITIS, outcomes: • Complete RESOLUTION • Walled off ABSCESS • ADHESIONS
- 187. SCLEROSING RETROPERITONITIS • Unknown cause (autoimmune?) • Generalized retroperitoneal fibrosis, progressive hydronephrosis
- 188. TUMORS • MESOTHELIOMAS (solitary nodules or diffuse constricting growth pattern, also asbestos caused) • METASTATIC, usually diffuse, often looking very much like pseudomyxoma peritoneii, but containing tumor cells, usually adenocarcinoma
