lec 1 RS-ppt (1).pptx
- 2. Intended Learning Outcomes Introduction to Renal System. Multiple Functions of the Kidneys Physiologic Anatomy of the Kidneys Renal Blood Supply Nephron
- 3. Location of the Kidneys Dimensions Reddish-brown, bean shaped 12cm long, 6cm wide, 3cm thick High on posterior abdominal wall at the level of T12 to L3- superior lumbar region Retroperitoneal & against the dorsal body wall The right kidney is slightly lower than the left ,convex laterally Attached to ureters, renal blood vessels, and nerves at renal hilus (medial indention) Atop each kidney is an adrenal gland
- 4. Coverings of the Kidneys Adipose capsule Surrounds the kidney Provides protection to the kidney Helps keep the kidney in its correct location against muscles of posterior trunk wall Ptosis-kidneys drop to a lower position due to rapid fat loss, creating problems with the ureters. Ptosis can lead to hydronephrosis, a condition where urine backs up the ureters and exerts pressure on the kidney tissue. Renal capsule Surrounds each kidney
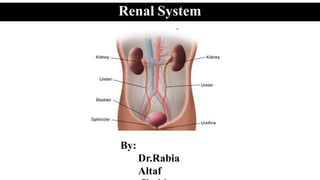
- 5. The organs of the urinary system include • the paired kidneys, • paired ureters, • urinary bladder • urethra Renal System
- 6. Multiple Functions of the Kidneys in Homeostasis Excretion of Metabolic Waste Products, Foreign Chemicals, Drugs, and Hormone Metabolites. Conserving valuable nutrients, by preventing their loss in urine Regulation of Water and Electrolyte Balances. Regulation of ArterialPressure. Regulation of Acid-Base Balance. Regulation of Erythrocyte Production. Regulation of 1,25–Dihydroxyvitamin D3 Production. Glucose Synthesis. Renal System
- 7. General Organization of the Kidneys and Urinary Tract Physiologic Anatomy of the Kidneys
- 8. General Organization of the Kidneys and Urinary Tract Physiologic Anatomy of the Kidneys
- 9. Physiologic Anatomy of the Kidneys Three regions of kidneys Renal cortex – outer region, forms an outer shell Renal columns – extensions of cortex- material inward Renal medulla – inside the cortex, contains medullary (renal) pyramids Medullary pyramids – triangular regions of tissue in the medulla, appear striated Renal pelvis – inner collecting tube, divides into major and minor calyces Calyces – cup-shaped structures enclosing the tips of the pyramids that collect and funnel urine towards the renal pelvis
- 10. Physiologic Anatomy of the Kidneys The walls of the calyces, pelvis, and ureter contain contractile elements that propel the urine toward the bladder, where urine is stored until it is emptied by micturition
- 12. The NEPHRON Is the Functional Unit of the Kidney In the kidneys, the functional units—the smallest structures that can carry out all the functions of a system— are the nephrons Each nephron consists of a Renal corpuscle o glomerular (Bowman’s) capsule o the glomerulus (glomerular capillaries) a renal tubule o The renal tubule has three crucial functions: 1) reabsorbing all the useful organic nutrients in the filtrate; 2) reabsorbing more than 90 percent of the water in the filtrate; 3) secreting into the tubule lumen any wastes that did not pass into the filtrate at the glomerulus.
- 13. The NEPHRON Is the Functional Unit of the Kidney the total glomerulus is encased in Bowman’s capsule. Fluid filtered from the glomerular capillaries flows into Bowman’s capsule and then into the proximal tubule, which lies in the cortex of the kidney. From the proximal tubule, fluid flows into the loop of Henle, which dips into the renal medulla. Each loop consists of a descending and an ascending limb. The walls of the descending limb and the lower end of the ascending limb are very thin and therefore are called the thin segment of the loop of Henle.
- 14. The NEPHRON Is the Functional Unit of the Kidney After the ascending limb of the loop has returned partway back to the cortex, its wall becomes much thicker, and it is referred to as the thick segment of the ascending limb. At the end of the thick ascending limb is a short segment, which is actually a plaque in its wall, known as the macula densa. Beyond the macula densa, fluid enters the distal tubule, which, like the proximal tubule, lies in the renal cortex. Collecting duct.
- 15. The NEPHRON Is the Functional Unit of the Kidney Blood arrives at the renal corpuscle by way of an afferent arteriole. Blood leaves the glomerulus in an efferent arteriole. It flows into a network of capillaries called the peritubular capillaries, which surround the renal tubule. These capillaries in turn drain into small venules that return the blood to the venous system
- 20. URINE FORMATION Different segments of the nephron form urine by filtration, reabsorption, and secretion Basic Processes of Urine Formation Filtration. Reabsorption of substances from the renal tubules into the blood Secretion of substances from the blood into the renal tubules. Urinary excretion rate = Filtration rate - Reabsorption rate + Secretionrate
- 21. URINE FORMATION The substance shown in panel A is filtered by the glomerular capillaries but is neither reabsorbed nor secreted.e.g. Certain waste products in the body, such as creatinine In panel B, typical for many of the electrolytes of the body. In panel C, This pattern occurs for some of the nutritional substances in the blood, such as amino acids and glucose, allowing them to be conserved in the body fluids. The substance in panel D, This pattern often occurs for organic acids and bases, permitting them to be rapidly cleared from the blood and excreted in large amounts in the urine.
- 22. Excretion Rate of different Substances Panel A • Substance is freely filtered by the glomerular capillaries but is neither reabsorbed nor secreted. • Excretion rate = Filtration rate • Eg: Creatinine Panel B • Substance is freely filtered but is also partly reabsorbed from the tubules • Excretion rate < Filtration rate • Eg: Most of the electrolytes
- 23. Excretion Rate of different Substances Panel C • Substance is freely filtered & is fully reabsorbed thus is not excreted • Excretion rate = 0 • Eg: AA andGlucose Panel D • Substance is freely filtered & is not reabsorbed, but additional quantities of this substance are secreted from the peritubular capillary • Excretion rate = Filtration rate + Secretion rate • Eg : Organic acids and Bases blood
- 24. Glomerular Filtration • It is the “First Step” in Urine Formation. • Blood is filtered through Filtration Barrier. • Endothelium • Basement Membrane • Filtration slit
- 25. URINE FORMATION Glomerular Filtration—The First Step in Urine Formation Composition of the Glomerular Filtrate Glomerular filtrate is essentially: Devoid of cellular elements like RBC/WBC/PLTand Protein-free The concentrations of most salts and organic molecules, are similar to the concentrations in the plasma. Exceptions include Calcium and fatty acids Because of the fact that, they are partially bound to the plasma proteins. Almost one half of the plasma calcium and most of the plasma fatty acids are bound to proteins, and these bound portions are not filtered through the glomerular capillaries.
- 26. URINE FORMATION GFR Is About 20 Per Cent of the Renal Plasma Flow the GFR is determined by 1) the balance of Hydrostatic and colloid osmotic forces acting across the capillary membrane and 2) the capillary filtration coefficient (Kf), the product of the permeability and filtering surface area of the capillaries. The filtration fraction is calculated as follows: Filtration fraction = GFR/Renal plasma flow
- 27. Glomerular Filtration Filterability • It is the “Degree of easiness for a substance to cross the glomerulus” • It is inversely propotional to Molecular weight (MW). • Negative charged molecules cross less easily than positive charged molecule for same MW, due to the fact that basement membrane and podocytes are also negatively charged.
- 28. URINE FORMATION Glomerular Capillary Membrane Filterability of Solutes Is Inversely Related to Their Size. The glomerular capillary membrane is thicker than most other capillaries, but it is also much more porous and therefore filters fluid at a high rate. Despite the high filtration rate, the glomerular filtration barrier is selective in determining which molecules will filter, based on their size and electrical charge.
- 29. URINE FORMATION Determinants of the GFR The GFR is determined by 1) the sum of the hydrostatic and colloid osmotic forces across the glomerular membrane, which gives the net filtration pressure, 2) the glomerular capillary filtration coefficient, Kf. Expressed mathematically, GFR = Kf × Net filtration pressure
- 30. URINE FORMATION Determinants of the GFR Net filtration pressure These forces include 1) Glomerular hydrostatic pressure, PG, which promotes filtration; 2) the hydrostatic pressure in Bowman’s capsule (PB) outside the capillaries, which opposes filtration; 3) the colloid osmotic pressure of the glomerular capillary plasma proteins (π G), which opposes filtration; and 4) the colloid osmotic pressure of the proteins in Bowman’s capsule (π B), which promotes filtration. The GFR can therefore be expressed as GFR = Kf × (PG – PB – πG + πB) PG – PB – πG +πB
- 31. URINE FORMATION Determinants of the GFR GFR = Kf × (PG – PB – πG +πB) Increased Glomerular Capillary Filtration Coefficient Increases GFR Kf = GFR/Net filtrationpressure Increased Bowman’s Capsule Hydrostatic Pressure Decreases GFR Increased Glomerular Capillary Colloid Osmotic Pressure Decreases GFR Increased Glomerular Capillary Hydrostatic Pressure Increases GFR PG – PB – PG +PB
- 32. Glomerular hydrostatic pressure • It is determined by three variables: (1) Arterial pressure ∞ GFR (2) Afferent arteriolar resistance 1/∞ GFR (3) Efferent arteriolar resistance ∞ GFR in the beginning; later on 1/∞ GFR The initial increase causes blood to stay in glomerulus for longer time thus GFR increases , but as soon as resistance increases more than 3 folds in efferent arteriole the RPF decreases, So GFR also declines
- 33. Filtration Fraction ( FF = GFR / RPF ) • It is the ratio of the GFR to the RPF. • Increasing the filtration fraction also concentrates the plasma proteins and raises the glomerular colloid osmotic pressure. Glomerular colloid osmotic pressure
- 34. URINE FORMATION Determinants of the GFR
- 35. Renal Blood Flow: In an average 70-kilogram man, the combined blood flow through both kidneys is about 1100 ml/min, or about 22 per cent of the cardiac output. As with other tissues, blood flow supplies the kidneys with nutrients and removes waste products. Renal Blood Flow and Oxygen Consumption: On a per gram weight basis, the kidneys normally consume oxygen at twice the rate of the brain but have almost seven times the blood flow of the brain. A large fraction of the oxygen consumed by the kidneys is related to the high rate of active sodium reabsorption by the renal tubules. If renal blood flow and GFR are reduced and less sodium is filtered, less sodium is reabsorbed and less oxygen is consumed. Therefore, renal oxygen consumption varies in proportion to renal tubular sodium reabsorption, which in turn is closely related to GFR and the rate of sodium filtered.
- 36. Determinants of Renal Blood Flow: Renal blood flow is determined by the pressure gradient across the renal vasculature Pressure gradient = The total vascular resistance through the kidneys is determined by the sum of the resistances in the individual vasculature segments, including the arteries, arterioles, capillaries, and veins An increase in the resistance of any of the vascular segments of the kidneys tends to reduce the renal blood flow, whereas a decrease in vascular resistance increases renal blood flow
- 37. Physiologic Control of Glomerular Filtration and Renal Blood Flow: The determinants of GFR that are most variable and subject to physiologic control include • the glomerular hydrostatic pressure and • the glomerular capillary colloid osmotic pressure. These variables, in turn, are influenced by the: • Sympathetic nervous system, • Hormones and autacoids and • Other feedback controls that are intrinsic to the kidneys. Sympathetic Nervous System Activation DecreasesGFR • Essentially all the blood vessels of the kidneys, including the afferent and the efferent arterioles, are richly innervated by sympathetic nerve fibers. • Strong activation of the renal sympathetic nerves can constrict the renal arterioles and decrease renal blood flow and GFR
- 38. Control of GFR: 1. NE and Epinephrine: Released from adrenal medulla. They constrict afferent and efferent arterioles, causing reductions in RBF & thus GFR is reduced. 2. Endothelin: Released by damaged vascular endothelial cells It is a powerful vasoconstrictor. Causes renal vasoconstriction & thus decreases GFR. 3. eNO: Released by the endothelium Decreases Renal Vascular Resistance and Increases GFR. 4. PGs and Bradykinin: It causes vasodilation & GFR is increased. These vasodilators are not of major importance in regulating GFR in normal conditions, but Under stressful conditions, such as volume depletion or after surgery, the administration of nonsteroidal anti-inflammatory drugs (NSAID’s), such as aspirin, that inhibit prostaglandin synthesis may cause significant reductions in GFR 5. Angiotensin: It preferentially constricts efferent arterioles. It should be kept in mind that increased angiotensin II formation usually occurs in circumstances associated with volume depletion, which tend to decrease GFR. In these circumstances, angiotensin II, by constricting efferent arterioles, helps prevent decreases in glomerular hydrostatic pressure and GFR. Thus it is better to say “Angiotensin II prevents ↓in GFR due to volume depletion”.
- 40. Autoregulation of GFR and Renal Blood Flow: Feedback mechanisms intrinsic to the kidneys normally keep the renal blood flow and GFR relatively constant, despite marked changes in arterial blood pressure. This relative constancy of GFR and renal blood flow is referred to as autoregulation. Importance of GFR Autoregulation in Preventing Extreme Changes in Renal Excretion: The autoregulatory mechanisms of the kidney are not 100 per cent perfect, but they do prevent potentially large changes in GFR and renal excretion of water and solutes that would otherwise occur with changes in blood pressure. Change in arterial pressure exerts much less of an effect on urine volume for two reasons: (1) renal autoregulation prevents large changes in GFR that would otherwise occur, and (2) there are additional adaptive mechanisms in the renal tubules that allow them to increase their reabsorption rate when GFR rises, a phenomenon referred to as glomerulotubular balance
- 41. Role of Tubuloglomerular Feedback in Autoregulation of GFR: To perform the function of autoregulation, the kidneys have a feedback mechanism that links changes in sodium chloride concentration at the macula densa with the control of renal arteriolar resistance. The tubuloglomerular feedback mechanism has two components that act together to control GFR: (1) an afferent arteriolar feedback mechanism and (2) an efferent arteriolar feedback mechanism. These feedback mechanisms depend on special anatomical arrangements of the juxtaglomerular complex
- 42. Tubuloglomerular Feedback Juxtaglomerular apparatus (1) Macula densa (2) Juxtaglomerular (JG) cells (3) Extraglomerular mesangium
- 43. Tubuloglomerular Feedback • Not completely understood. • Experiment suggests that decreased GFR slows the flow rate in the loop of Henle, causing increased reabsorption of sodium and chloride ions in the ascending loop of Henle, thereby reducing the concentration of sodium chloride at the macula densa cells.
- 44. Tubuloglomerular Feedback • This decrease in sodium chloride concentration initiates a signal from the macula densa that has two effects : 1. It decreases resistance to blood flow in the afferent arterioles • Which raises glomerular hydrostatic pressure and helps return GFR toward normal 2. It increases renin release from the juxtaglomerular cells • Renin increases the formation of angiotensin I from angiotensinogen, which is converted to angiotensin II. • Finally, the angiotensin II constricts the efferent arterioles, thereby increasing glomerular hydrostatic pressure and returning GFR toward normal.
- 45. Autoregulation of GFR and Renal Blood Flow Role of Tubuloglomerular Feedback in Autoregulation of GFR Decreased Macula Densa Sodium Chloride Causes Dilation of Afferent Arterioles and Increased Renin Release.
- 47. • Myogenic Autoregulation of Renal Blood Flow andGFR • Another mechanism that contributes to maintenance of a relatively constant renal blood flow and GFR. • Ability of individual blood vessels to resist stretching during increased arterial pressure, a phenomenon referred to as the myogenic mechanism. • Muscles of small arterioles respond to increased wall tension or wall stretch by contraction of the vascular smooth muscle.
- 48. Myogenic Autoregulation of Renal Blood Flow andGFR (cont.) • Stretch of the vascular wall allows increased movement of calcium ions from the extracellular fluid into the cells, causing them to contract. • This contraction prevents over distention of the vessel and at the same time, by raising vascular resistance, helps prevent excessive increases in renal blood flow and GFR when arterial pressure increases.
- 49. Why increased protein intake causes increased GFR? • GFR and renal blood flow increase 20 to 30 per cent within 1 or 2 hours after a person eats a high-protein meal. Possible explanation is : • Increased release of AA in blood, which are reabsorbed in the PCT. • AA and sodium are reabsorbed together by the proximal tubules, increased amino acid reabsorption also stimulates sodium reabsorption in PCT. • This decreases sodium delivery to the macula densa, which elicits a tubuloglomerular. • Decreased afferent arteriolar resistance then raises renal
- 50. Why polyuria in Diabetes? • Large increases in blood glucose levels in uncontrolled diabetes mellitus. • Because glucose is also reabsorbed along with sodium in PCT, increased glucose delivery to the tubules causes them to reabsorb excess sodium along with glucose. • This, in turn, decreases delivery of sodium chloride to the macula densa, activating a tubuloglomerular feedback.
- 51. REFERENCES 59 BOOKS: Textbook of Medical Physiology by Guyton & Hall 11th Edition, Chapter26