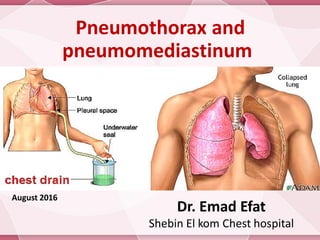
Pneumothorax and pneumomediastinum
- 1. Pneumothorax and pneumomediastinum Dr. Emad Efat Shebin El kom Chest hospital June 2017
- 2. Definition Pneumothorax: Is collection of air within the pleural space with secondary lung collapse.
- 4. Syndromes Spontaneous pneumothorax: Pneumothorax in the absence of iatrogenic or traumatic injury to the chest or lung. Classified into : 1. 1ry spontaneous pneumothorax: usually occurs at rest without any prior lung disorders or diseases. 2. 2ry spontaneous pneumothorax: can occur as a complication of underlying lung disease. Traumatic pneumothorax: Results from blunt or penetrating injury that disrupts the parietal or visceral pleura. Iatrogenic pneumothorax is secondary to diagnostic or therapeutic medical intervention
- 5. Syndromes Tension pneumothorax : Is a life-threatening condition caused by air within the pleural space that is under pressure; displacing mediastinal structures and compromising cardiopulmonary function. Artificial pneumothorax : It is introduction of measured volume of air into pleura by needle using device Indication:- Treatment of pulmonary TB in the era before antituberculous therapy, but now obsolete Diagnostically ; in thoracoscopic exam.
- 6. Syndromes Catamenial pneumothorax Occurs in conjunction with menstruations & is usually recurrent. It is rare phenomenon which the usual way in which the thoracic endometriosis declares itself It generally occurs in women aged 30-40 years. It frequently begins 1-3 days after menses onset. The majority (90-95% ) affect the Right hemithorax, but isolated Left side or bilateral pneumothorax has been reported. Catamenial pneumothorax is usually treated by: 1. Oral contraceptive or danazol (weak androgen) in few cases to suppress ovulation. 2. Surgical menopause by hysterectomy with bilateral oopherectomy 3. Thoracotomy with pleural abrasion or pleurectomy
- 7. Syndromes Pneumomediastinum : (Air in mediastinal tissue or mediastinal emphysema) 1. 1ry spontaneous Pneumomediastinum : usually occurs without any prior lung disorders or diseases 2. 2ry spontaneous Pneumomediastinum : can occur as a complication of underlying lung or mediastinal diseases , most often any cause of 2ry spontaneous Pneumomediastinum . Bilateral spontaneous pneumothorax: Is rare & may be rapidly fatal if occurring , may be due to: 1.Rupture bilateral apical blebs simultaneously 2. Patient with extensive bilateral emphysema or cystic lung disease
- 8. Pathophysiology If the air enters the pleural cavity from: The outside (open pneumothorax) from the lung (closed pneumothorax) Primary spontaneous pneumothoraces (PSP): Results from apical pleural blebs related to airway inflammation from cigarette smoking in many patients & it is dose-dependent. Secondary spontaneous pneumothoraces (SSP): Occurs in the presence of lung disease, e.g. COPD . Air enter the pleural space via distended, damaged, or compromised alveoli.
- 10. Pathophysiology Tension pneumothorax: The condition develops from a combination of mechanical and hypoxic effects. The injured tissue forms a one-way valve, allowing air to enter the pleural space and preventing the air from escaping naturally the pressure of trapped air the ipsilateral lung collapses and the mediastinum shifts toward the contralateral side compression of the contralateral lung and the vasculature entering the Right atrium of the heart respiratory insufficiency, cardiovascular collapse, death if untreated.
- 12. Pathophysiology Pneumomediastinum Air escapes into the mediastinum from: Rupture of alveoli bordering the mediastinum. Esophageal trauma or elevated airway pressures. Air may then travel superiorly into the visceral, retropharyngeal, and subcutaneous spaces of the neck. From the neck, the subcutaneous compartment is continuous throughout the body; thus, air can diffuse widely (Subcutaneous emphysema). Mediastinal air can also pass inferiorly into the retroperitoneum and other extraperitoneal compartments. The mediastinal parietal pleura may rupture and cause a pneumothorax.
- 13. Causes 1ry Spontaneous pneumothorax The male-to-female ratio is about 6:1 . most likely to occur during the fall or winter months. Occurs most often in persons early in the third decade of life . Occurs from the rupture of subpleural apical emphysematous blebs or bullae . Smoking the risk by more than 22 fold in men and by nearly 10-fold in women. The risk is directly dose related to smoking PSP is typically observed in tall people due to increased shear forces in the apex. Familial tendency has been noted
- 14. Causes 2ry spontaneous pneumothorax Occur as a complication of underlying lung disease: Diseases of the airways: COPD, cystic fibrosis, and status asthmaticus ,………..etc. Interstitial lung diseases : (sarcoidosis, fibrosis, tuberous sclerosis,………..etc) Infectious diseases : Pneumonia (especially with Staph. Pn, Klebsiella, Pseudomonas, and Pneumocystis species), tuberculosis, pertussis, lung abscess ,………..etc. Malignancies: Sarcoma, lung cancer . Pneumoconiosis . Connective tissue diseases . Chemotherapy for malignancy . Radiation therapy .
- 15. Causes Iatrogenic pneumothorax Transthoracic needle aspiration procedures (most common cause, accounting for 32-37% of cases) Transbronchial lung biopsy, Pleural biopsy, liver biopsy or surgery Thoracentesis Tracheostomy Mechanical ventilation (directly related to peak airway pressures) , central venous cannulation; hyperbaric oxygen therapy. Cardiopulmonary resuscitation Subclavian and supraclavicular cannulation Intercostal nerve block . Unsuccessful attempts to convert an open pneumothorax to a simple pneumothorax in which the occlusive dressing functions as a 1-way valve can lead to a tension pneumothorax.
- 16. Causes Traumatic pneumothorax Penetrating (Open pneumothorax ) and non penetrating injury . Rib fracture . Thoracic endometriosis : Leading to catamenial pneumothorax . Other causes: Tall, thin stature in a healthy person or a person with Marfan syndrome. High-risk occupation (e.g., diving, flying) . Acupuncture Tension Pneumothorax Any condition that leads to pneumothorax can cause a tension pneumothorax
- 17. Causes Pneumomediastinum Acute production of high intrathoracic pressures (usual cause) Mechanical ventilation Severe cough & Smoking marijuana Asthma Inhalation of cocaine Athletic competition Respiratory tract infection Decompression of intrathoracic gas Violent vomiting may cause vertical tear in the lower 8cm of esophagus postero-laterally Trauma ( traheostomy) or surgical disruption of the oropharyngeal, esophageal, or respiratory mucosa
- 18. Clinical Details History Primary spontaneous pneumothorax usually develops at rest, and many affected individuals do not seek medical attention for days after symptoms develop depending on the severity of the incident. The major symptom is chest pain - sharp or stabbing pain, radiating to ipsilateral shoulder and increasing with inspiration (pleuritic) Secondary spontaneous pneumothorax: Dyspnea more severe Anxiety, cough, malaise and Cyanosis tension pneumothorax Sudden chest pain, extreme dyspnea, consciousness decreased and cyanosis.
- 19. Clinical Details General examination: General appearances may be normal Diaphoretic Splinting chest wall to relieve pleuritic pain . Cyanotic (with tension pneumothoraces and SSP ) . With a tension pneumothorax: Increasing resistance to providing adequate ventilation assistance Tachycardia, Pulsus paradoxus & Hypotension (key sign of a tension pneumothorax) Jugular venous distension Tracheal deviation (late finding) Abdominal distension
- 20. Clinical Details General examination: Vital signs: Tachypnea Tachycardia (most common finding) Pulsus paradoxus Hypotension (with tension pneumothorax)
- 21. Clinical Details Chest Ipsilateral diminished chest movement & may be appear larger with mediastinal and tracheal shift which suspects tension pneumothorax Hyperresonant percussion note. Distant or absent breath sounds & tactile focal fremitus on affected side. Hydropneumothorax :- Succusion splashing sound is produced by rocking the patient. to & fro. The coin test , scratch sign is sometime usefully employed. In open pneumothorax: Air may be heard passing in and out of the wound with breathing.
- 22. Clinical Details In ventilated patients, the physician may begin to suspect tension pneumothorax when: Sudden onset of tachycardia & hypotension (key sign of a tension pneumothorax) The distressed patient appearing to fight the ventilator Sudden decline in O2 saturation Increased pleural pressures necessitate an increase in peak airway pressure in order to deliver the same tidal volume. Decreased expiratory volumes (air leakage into the pleural space) and increased end-expiratory pressure.
- 23. Clinical Details Clinical feature of Pneumomediastinum: None (Physical findings are absent in some patients.) Central chest pain, radiating to the neck, back, or shoulders and exacerbated by deep inspiration, coughing, or supine positioning & relived by leaning forward & by shallow breathing. Neck pain accompanied by Dysphagia & Subcutaneous emphysema of the chest wall Hamman sign “precordial crunching” It result from free air in the mediastinum moving heart muscle Pulsus paradoxus in absence of asthma May be cardiac tamponad from air surrounding the heart dyspnoea, cyanosis & hypotension 2ry spontaneous or traumatic types symptoms & signs of associated disease ± fever, pleural effusion, or empyema
- 24. Investigations - X-ray X-ray: The first investigation performed (confirms pneumothorax) A linear shadow of visceral pleura (the pleural line) with lack of lung markings peripheral to it, indicating collapsed lung. Contralateral deviation of mediastinal structures, & rib cage expansion is evidence of a tension pneumothorax . Delayed traumatic pneumothorax can develop in penetrating chest wound. Obtain serial chest radiographs every 6 hours in the 1st day of injury to rule this out. In tension pneumothorax if a chest x-ray is obtained safely, findings can include: lung collapse at the hilum, diaphragmatic depression and widened intercostal spaces on the affected side Tracheal and mediastinal deviation to the contralateral side.
- 25. Investigations - X-ray Rotation of CXR can obscure a pneumothorax . Rotation can also mimic a mediastinal shift. Expiratory images are thought to better depicting minimal (subtle) pneumothoraces. In erect patients: Pleural gas collects over the apex .
- 26. Investigations - X-ray In the supine position: The juxtacardiac area, the lateral chest wall, and the subpulmonic region are the best areas to search for evidence of pneumothorax. The deep sulcus sign: (very wide and deep costophrenic angle) An ipsilateral increased lucency in the upper quadrant of the abdomen. Double Diaphragm Sign: both the diaphragmatic dome and anterior portions of the diaphragm are visualized
- 27. Investigations - X-ray Double Diaphragm Sign of Pneumothorax. Air in the right hemithorax displaces both the dome (white arrow) and the anterior costophrenic angle (yellow arrow) in this patient with a large, right-sided pneumothorax. There is also a deep sulcus sign present (red arrow).
- 28. Investigations - X-ray A large pneumothorax as being of greater than 2 cm width at the level of the hilum. The volume of a pneumothorax approximates to the ratio of the cube of the lung diameter to the hemithorax diameter lateral decubitus studies: Should be done with the suspected side up the lung will then 'fall' away from the chest wall Rib films are indicated This chest X-ray shows a large pneumothorax (P) which is >2 cm depth at the level of the hilum.
- 29. Investigations - X-ray A bulla or thin wall cyst can be mistaken for loculated pneumothorax. The pleural line caused by pneumothorax is usually bowed at its center towards lateral chest wall but the inner margins of bulla or cyst is generally concave rather than convex. Pneumothorax with pleural adhesion may simulate bulla or lung cyst. DD by comparison with previous chest radiography, lateral decubitous or CT scanning A chest radiograph shows RT bullous formation
- 30. Investigations - X-ray A skin fold can be mistaken for a pneumothorax. Unlike pneumothorax, skin folds usually continue beyond the chest wall, and lung markings can be seen beyond the apparent pleural line.
- 31. Deep sulcus sign (red arrow) in a supine patient in the ICU. The pneumothorax is subpulmonic. Investigations - X-ray
- 32. Investigations - X-ray Hydropneumothorax: with the patient upright, there will be an air-fluid level in the thoracic cavity On supine radiographs, a hydropneumothorax will be more difficult to see although a uniform grayness to the entire hemithorax with the absence of vascular markings suggest the diagnosis
- 33. Investigations - X-ray Radiographic features of Pneumomediastinum PA Chest X-Ray Small amounts of air appear as linear or curvilinear lucencies outlining mediastinal contours and form: 1. Subcutaneous emphysema 2. Air anterior to pericardium: (Pneumoprecardium) Pneumo- precardium subcutaneous emphysema
- 34. Investigations - X-ray Radiographic features of Pneumomediastinum PA Chest X-Ray 3. air around pulmonary artery and main branches: ring around artery sign 4. air outlining major aortic branches: tubular artery sign Tubular Artery Sign (Red arrows) Ring around artery sign
- 35. Investigations - X-ray Radiographic features of Pneumomediastinum PA Chest X-Ray 5. continuous diaphragm sign: due to air trapped posterior to pericardium 6. Spinnaker Sail Sign (angel wing sign) is seen on neonatal postero-anterior CXR when thymic lobes are displaced laterally by air, (Very typical sign in neonatal age). Spinnaker Sail Sign (angel wing sign) Continuous diaphragm sign
- 36. Investigations - X-ray Radiographic features of Pneumomediastinum PA Chest X-Ray Naclerio V sign It is seen as a V-shaped air collection. One limb of the V is produced by mediastinal air outlining the left lower lateral mediastinal border. The other limb is produced by air between the parietal pleura and medial left hemidiaphragm. Lateral Chest X-Ray Retrosternal air Lateral Decubitus Chest X-Ray Air will not move with change in position Neck Films Air outlining fascial planes of the neck Naclerio V sign
- 37. HRCT benefits: 1. CT is the most reliable imaging study for the diagnosis, but it is not recommended for routine use 2. Confirm the diagnosis of pneumothorax in mechanically ventilated patients 3. Detect underlying emphysema, parenchymal and pleural diseases 4. Determine the exact size of the pneumothorax Moderate left-sided pneumothorax. (A) Axial and ( B ) coronal CT demonstrating subpleural blebs ( blue arrow ). Red arrows indicate pneumothorax Investigations - CT scanning
- 38. 5. Detect occult (a pneumothorax that is seen only on CT and not a conventional chest x-ray) pneumothoraces, blebs, bullae, cysts and pneumomediastinum a) Anteroposterior supine radiograph shows no abnormality. b) CT scan shows the existence of an occult pneumothorax on the right side. Tension pneumothorax (green arrow) and subcutaneous emphysema (red arrow). CT shows increased volume of the right hemithorax, reduction of ipsilateral pulmonary volume and shifts the mediastinum to the left Investigations - CT scanning
- 39. 6. Distinguish between a large bulla and a pneumothorax Chest radiograph shows unilateral hyperlucency affecting the entire right lung (white arrows). (b) CT demonstrates a large bulla (star) on the right side causing considerable compression of the mediastinum Investigations - CT scanning
- 40. CT shows large asymmetric upper lobe bullae. Chest tube is located peripherally in right pleural space. Note presence of air in pleural space surrounding anterior bulla on right (arrow) and parallel configuration of bulla wall with chest wall. This is double-wall sign of pneumothorax. 7. "Double wall" sign described in cases with ruptured bulla causing pneumothorax (air outlining both sides of the bulla wall parallel to the chest wall). Investigations - CT scanning
- 41. Hydropneumothorax: The concurrent presence of both free fluid and air within the pleural space It can occur secondary to various situations such as thoracocentesis, thoracic trauma, esophagopleural fistula, neoplastic processes, post- traumatic, post-pneumonectomy, infection, pulmonary infarction, cystic lung disease, obstructive lung disease or bronchopleural fistula. CT depicts hydropneumothorax, with the horizontal air fluid interface Axial contrast CT image demonstrates a right-sided hydropneumothorax. Note the air and fluid interface (arrow). Investigations - CT scanning
- 42. A loculated pneumothorax is a pocket of pleural air trapped in a localised area. The plain film appearances may be subtle. Chest CT revealed a loculated pneumothorax chest CT revealed Bilateral loculated pneumothoraces Investigations - CT scanning
- 43. Pneumomediastinum: CT findings: assess the extent, (i.e., mild, moderate or severe) Detect possible aerodigestive tract injuries. differentiate between pneumomediastinum and pneumopericardium Pneumomediastinum: CT also shows air surrounding the mediastinal structures (arrows). Pneumomediastinum. There is air in the mediastinum surrounding the aorta and trachea (arrows). Investigations - CT scanning
- 44. Investigations - Ultrasonography Ultrasonography: A bedside technique, more sensitive than CXR and Useful in unstable patients who cannot go outside emergency department. In a supine patient, air accumulates in the anterior region of the chest at the second to fourth intercostal spaces in the mid- clavicular line. It is the recommended initial area for investigation in a trauma Sonographic modes: B-mode, or brightness mode: provides real-time imaging of structures that are clearly observable M-mode, or motion mode: determine a structure’s movement over time.
- 45. Investigations - Ultrasonography Sonographic signs: 1. bat sign: For the typical supine patient, Begin by selecting B-mode and place the probe on the anterior part of the chest. Obtain the bat sign, which is a basic sonographic landmark. It consists of an upper rib, a lower rib, and the pleural line. The periosteum of the ribs represents the wings and the bright hyperechoic pleural line in between them represents the bats’ body
- 46. Investigations - Ultrasonography Sonographic signs: 2. Lung Sliding sign: Between ribs in normal aerated lung, parietal and visceral plura are seen sliding across one another. the presence of lung sliding rules out pneumothorax at the location of the probe.
- 47. Investigations - Ultrasonography Sonographic signs: 3. seashore sign: By using M-mode, two different patterns are displayed in normal lung : The motionless portion above the pleural line creates horizontal “waves”, and the sliding below it creates a granular pattern, the ‘sand’, this resembles waves crashing in onto the sand.
- 48. Investigations - Ultrasonography Sonographic signs: 4. Stratosphere/barcode sign: M-mode only displays one pattern of parallel horizontal lines above and below the pleural line. This pattern resembles a “barcode” barcode
- 49. Investigations - Ultrasonography Sonographic signs: 5. Z-lines/comet tails/rockets: Small, vertical tapering hyperechoic lines that diminish distally, caused by air-fluid interface at the pleural line. Absent when air or pneumothorax is present The comet-tail artifact ( yellow arrows): an ultrasound sign ruling out pneumothorax.
- 50. Investigations - Ultrasonography Sonographic signs: 6. B-lines: The B-lines appear in B-mode ultrasonography as thin, vertical beams; however, they are really tiny horizontal lines tightly stacked on top of each other at increasing depth. B-lines that occur in a series of 3 or more have been termed B+ lines. The presence of B-lines is especially important to rule out pneumothorax “B-lines” (white arrows) originating from pleural line, extending to the edge of the screen.
- 51. Investigations - Ultrasonography Sonographic signs: 7. lung-point sign: Yellow arrow Indicates the lung point in M- mode: This is the region where the intra- pleural air (pneumothorax) ends and normal pleural connection (seashore sign) begins. Note the characteristic streaking of the barcode/stratosphere sign on the lower indicating pneumothorax. The B-mode image (upper portion of image) will reveal the absence of lung sliding on a dynamic ultrasound scan.
- 52. Investigations Contrast-enhanced esophagogram: If emesis or retching is the precipitating event, an esophagogram should be obtained to evaluate Boerhaave syndrome (an esophageal tear), which has a high mortality rate . The electrocardiogram (ECG): Patient with left pneumothorax may shows changes suggesting antero lateral myocardial infarction ( A right axis deviation, poor R wave progression, ↓QRS amplitude & precordial T wave inversion ). Lab Studies Arterial blood gas In patients with severe lung disease In those with persistent respiratory distress despite treatment ABG analysis may be useful in evaluating the following: Hypoxia, Hypercarbia and respiratory acidosis
- 53. Differential diagnosis Pulmonary embolism Dissecting aortic aneurysm, rupture Esophageal spasm, Perforation, Rupture and Tears. Acute pericarditis Acute myocardial infarction Acute Coronary Syndrome Congestive Heart Failure and Pulmonary Edema Haemothorax Pleural effusion ARDS Asthma Foreign Bodies, Trachea Adult Diaphragmatic Injuries
- 54. Pneumothorax Treatment Treatment Based on Risk Stratification (Patient presentation ): The following are possible presentations of patients with pneumothorax: Asymptomatic (incidental finding): Treatment decisions are guided by estimate of long-term recurrence risk. Symptomatic but clinically stable: The British Thoracic Society (BTS) advocates for simple aspiration and deferring hospitalization in PSP A small-bore catheter or chest tube placement is recommended by the American College of Chest Physicians (ACCP) Clinically fragile: air evacuation and observation; comorbid conditions may preclude observation Life-threatening: must be treated immediately with tube thoracostomy
- 55. Pneumothorax Treatment Selection of site of patient care Outpatient care: This can occur in asymptomatic patients or those with a small pneumothorax and reliable follow-up Emergency department (ED) care: when Prolonged periods of observation are inefficient and clinically suboptimal; manual aspiration and placement of one-way valves are performed. Inpatient care: when high flow Oxygen is needed, the pneumothorax is larger but the patient is stable, or associated comorbidities ; the average hospital stay is 2-8 days Intensive care unit (ICU): for patients who are unstable or intubated
- 56. Pneumothorax Treatment Options for Restoring Air-Free Pleural Space: 1. Observation without oxygen 2. Administering supplemental oxygen 3. Simple aspiration 4. Chest tube placement 5. One-way valve insertion 6. Thoracostomy with continuous suction.
- 57. Pneumothorax Treatment 1. Observation without oxygen: Simple observation is appropriate for asymptomatic patients with a minimal pneumothorax (<15-20% by Light criteria; 2-3 cm from apex to cupola by alternate criteria) with close follow-up, ensuring no enlargement. Air is reabsorbed spontaneously 2. Supplemental oxygen: Oxygen administration at 3 L/min nasal canula or higher flow treats possible hypoxemia and is associated with a fourfold increase in the rate of pleural air absorption compared with room air alone.
- 58. Pneumothorax Treatment 3. Simple aspiration: A more recent ED study supports needle aspiration as safe and effective as chest tube placement for PSP, conferring the additional benefits of shorter length of stay and fewer hospital admissions 4. Chest tube placement: A tube inserted into the pleural space is connected to a device with one-way flow for air removal. Examples of such devices are Heimlich valves or water seal canisters, and tubes connected to wall suction devices.
- 60. Pneumothorax Treatment 5. One-way valve insertion (portable system): The typical goal of inserting one-way valve systems is to avoid hospital admission and still treat the spontaneous pneumothorax. One-way valves may be used during transport of an injured patient. A Heimlich valve is a one-way, rubber flutter valve that allows for complete evacuation of air that is not under tension Effective as simple manual needle aspiration or a conventional chest tube thoracotomy.
- 61. Pneumothorax Treatment One-way valve insertion (portable system): Heimlich valve
- 62. Pneumothorax Treatment 6. Thoracostomy with continuous wall suction: First time SPS (including chronic obstructive pulmonary disease [COPD]) and traumatic pneumothorax typically require this approach. A small-bore catheter (eg, 7-14 French) is safe to use in most patients, whereas a larger chest tube (24 French) is also appropriate initially, and increasing suction pressure can be used if the lung fails to inflate. A larger tube (eg, 28 French) can reduce resistance in patients who are ventilated and at greater risk for air leaks.
- 63. Pneumothorax Treatment Prehospital Care: Assess the ABCs (airway, breathing ,circulation). Evaluate the possibility of a tension pneumothorax. Assess the vital signs. Perform pulse oximetry. A tension pneumothorax is almost always associated with hypotension. Administer oxygen to the patient, ventilate the patient, and establish an intravenous (IV) line. Needle decompression for immediate relief of a tension pneumothorax. Prehospital ultrasonography: could provide diagnostic and therapeutic benefit when conducted by a proficient examiner In open pneumothorax: occlude wound with dressing (3 sides only to allow air to escape during expiration)
- 64. Pneumothorax Treatment Prehospital Care: Three sided occlusive dressing for open pneumothorax. It can be made from a good quality plastic bag and a roll of tape. The open side of the plastic is on the bottom side of the dressing to encourage any blood expelled from the wound to run downhill and out of the dressing
- 65. Pneumothorax Treatment Emergency Department Care: check: ABCs, Vital signs, Oxygen saturation. Give oxygen. Admission to the hospital. Bedside ultrasonography to look for cardiac tamponade, massive pulmonary embolus, severe hypovolemia, and tension pneumothorax
- 66. Pneumothorax Treatment Tension pneumothorax (a medical emergency) : Is a clinical diagnosis and a high index of suspicion and knowledge of basic emergency thoracic decompression are important for all health care personnel. Initial management: Establishing ABCs. Emergency endotracheal intubation in: Apnea, profound shock, and inadequate ventilation. Cover a sucking chest wound. Volume replenishment in hemorrhagic shock.
- 68. Pneumothorax Treatment 1. Urgent needle thoracocentesis: Performed prior to chest radiographs (is not indicated) and based on physical examination. It is both: Diagnostic (confirming suspicion) and Therapeutic (relieving the pneumothorax ) . The procedure : Insertion of a 14 or 16 gauge catheter over the needle at the second anterior intercostal space in the midclavicular line (over 3rd rib) or in the fourth or fifth intercostal space over the superior rib margin in the anterior axillary line (similar to for chest drain insertion). The catheter is connected to a 3-way stopcock and a large-volume syringe. Aspiration is performed. Leave the catheter in place until the chest tube is placed.
- 70. Do NOT x-ray - this is a clinical diagnosis Immediate needle decompression. Confirm side clinically. Inform patient. 14G cannula . 2nd intercostal space. Listen for hiss. Protect with gauze. Tape and leave in situ. Prepare chest drain for insertion.
- 71. Chest tap with 60 ml syringe, 3-way stopcock, IV extension tube, and 16 gauge needle .
- 72. Pneumothorax Treatment Primary spontaneous pneumothorax : Stop smoking. 1. Small (involving <15% of hemithorax): Observation and oxygen to asymptomatic patient. Needle aspiration to symptomatic hemodynamically stable patient. 2. large (involving >15-20% of hemithorax): Drained by aspiration using a pigtail catheter left to low suction or water seal is recommended. Strong suction should not be used with PSP because of delayed presentation increased risk of re-expansion pulmonary edema Follow-up chest radiographs are performed: If residual pneumothorax is present after 12 hour attach the catheter to underwater seal. If not succeed, do tube thoracostomy
- 74. Pneumothorax Treatment Secondary spontaneous pneumothoraces : 1. Admission to hospital for at least 24 h and receive supplemental oxygen (caution for patients with carbon dioxide retention) 2. Aspiration is less likely to be successful in SSP but can be considered in small pneumothoraces (Size 1-2cm) in an attempt to avoid chest drain insertion. 3. Tube thoracostomy is the procedure of choice in large pneumothoraces (Size >2cm ) or failed aspiration of small one. 4. Thoracotomy or video-assisted thoracoscopy: To excise the bullae. 5. Medical pleurodesis or ambulatory management with a Heimlich valve: may be appropriate for inoperable patients.
- 75. Pneumothorax Treatment Tube thoracostomy : Insert a chest tube in the fourth or fifth intercostal space over the superior rib margin in the anterior axillary line. Indications: Pneumothorax: open or closed; simple or tension Hemothorax, Hemopneumothorax, drain a malignant pleural effusion, drain a empyema. They can also be placed postoperatively following a thoracotomy, esophagectomy or cardiac surgery. For children: Chest drain insertion in 4th or 5th intercostal space mid- axillary line. Drain size: Use a large drain for blood (i.e. 16 gauge for a 5-10 kg child) and a smaller drain for pneumothorax.
- 77. Chest tube
- 78. Pneumothorax Treatment Video-Assisted Thoracoscopic Surgery (VATS): Is a minimally invasive surgical technique Used to diagnose and treat problems in the chest. VATS can replace a traditional thoracotomy, which uses one larger incision to gain access to the chest. The minimally invasive procedure typically results in less pain and faster recovery time for the patient, among other advantages for patients.
- 79. Pneumothorax Treatment One or more small incisions are made in the chest. A tiny fiber-optic camera (called a thorascope) is inserted through one incision, and surgical instruments are inserted through this or other small incisions. Video-Assisted Thoracoscopic Surgery (VATS): The thorascope transmits images of the inside of the chest on a video monitor, guiding the surgeon in maneuvering the instruments to complete the procedure.
- 80. Pneumothorax Treatment Iatrogenic pneumothorax: Aspiration is the technique of choice, because recurrence is usually not a factor. Tube thoracostomy is reserved for very symptomatic patients. Traumatic pneumothorax: In general, traumatic pneumothoraces should be treated with insertion of a chest tube. A subset of patients who have a small (<15-20%), minimally symptomatic pneumothorax may be admitted, observed closely, and monitored by using serial chest radiographs. administration of 100% oxygen promotes resolution.
- 82. Pneumothorax Treatment Catamenial pneumothorax: Oral contraceptives carry a high success rate May also (rarely) be treated surgically Pneumomediastinum: Most patients with pneumomediastinum should be observed for signs of serious complications (e.g., pneumothorax, tension pneumothorax, mediastinitis). If the pneumomediastinum occurred from the inhalation of cocaine or smoking of marijuana, observation in the ED for progression may be indicated. A follow-up chest radiograph should be obtained in 12-24 hours to detect any progression or complication, such as pneumothorax. If no progression occurs at 24 hours and if no evidence of mediastinitis exists, the patient may be discharged.
- 83. Pneumothorax Treatment Surgical strategies: Open thoracotomy and pleurectomy. Video-assisted thoracoscopic surgery (VATS) with pleurectomy and pleural abrasion. Indications for surgical assistance: Repeated episodes of pneumothorax The lung remains unexpanded after 5 days Persistent air leak for more than 7 days Contralateral pneumothorax Bilateral pneumothorax A high-risk occupation (e.g., diver, pilot) In acquired immunodeficiency syndrome (AIDS) patients Lymphangiomyomatosis, a condition at a high risk of pneumothorax
- 84. Pneumothorax Treatment Drug treatment: Local Anesthetics (Lidocaine hydrochloride): Used for analgesia, for thoracentesis and chest tube placement. Opiate Analgesics (Fentanyl citrate and Morphine): Used for pain control, ensures patient comfort, and promotes pulmonary toilet. Benzodiazepines (Midazolam and Lorazepam ): Used for conscious sedation,in premedication before pleurodesis, sclerotherapy or placement of a thoracostomy tube. Antibiotics (Doxycycline and Cefazolin): In patients with repeated pneumothoraces who are not good candidates for surgery, pleurodesis (or sclerotherapy) may be necessary. Prophylactic antibiotics are not recommended for the placement of chest tubes in non-traumatic causes.
- 85. Pneumothorax-Complications Pneumothorax complications include the following: Hypoxemic respiratory failure Respiratory or cardiac arrest Hemopneumothorax Bronchopulmonary fistula Pulmonary edema (following lung reexpansion) Empyema Pneumomediastinum Pneumopericardium Pneumoperitoneum Pyopneumothorax Complications of surgical procedures: Infection of the pleural space, Persistent air leak and Pain at the site of chest tube insertion
- 86. Recurrent Pneumothorax Recurrent Pneumothorax: the recurrence rate for primary pneumothorax is more than 20% after the first episode and even greater after the second episode and tends to be more likely in women, tall men and smokers Causes of recurrent spontaneous pneumothorax are: Cystic fibrosis Lung cysts Emphysematous bulla / apical subpleural bleb Rupture of bronchogenic carcinoma / esophageal carcinoma Honeycomb lung Catamenial pneumothorax (associated with menstruation) AIDS
- 87. Recurrent Pneumothorax Available treatment options include: Medical treatment: Medical chemical plerurodesis: should only be used if a patient is either unwilling or unable to undergo surgery Surgical treatment: Video-assisted thoracoscopic surgery (VATS) with (partial) pleurectomy or talc poudrage A thoracotomy with partial or complete pleurectomy
- 88. Pneumothorax - Prevention of Recurrent Strategies for the prevention of recurrent include: Prompt recognition and treatment of bronchopulmonary infections When subclavian vein cannulation is required, use the supraclavicular approach rather than the infraclavicular approach when possible The incidence of iatrogenic tension pneumothorax may be decreased with prophylactic insertion of a chest tube in patients with a simple pneumothorax that requires positive pressure ventilation Pleurodesis decreases the risk of recurrence of spontaneous pneumothorax Thoracotomy or VATS to excise the bullae
