8086990 lecture-notes-for-mental-health-nursing-psych-nursing
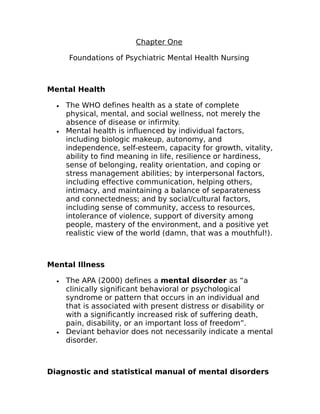
- 1. Chapter One Foundations of Psychiatric Mental Health Nursing Mental Health · The WHO defines health as a state of complete physical, mental, and social wellness, not merely the absence of disease or infirmity. · Mental health is influenced by individual factors, including biologic makeup, autonomy, and independence, self-esteem, capacity for growth, vitality, ability to find meaning in life, resilience or hardiness, sense of belonging, reality orientation, and coping or stress management abilities; by interpersonal factors, including effective communication, helping others, intimacy, and maintaining a balance of separateness and connectedness; and by social/cultural factors, including sense of community, access to resources, intolerance of violence, support of diversity among people, mastery of the environment, and a positive yet realistic view of the world (damn, that was a mouthful!). Mental Illness · The APA (2000) defines a mental disorder as “a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and that is associated with present distress or disability or with a significantly increased risk of suffering death, pain, disability, or an important loss of freedom”. · Deviant behavior does not necessarily indicate a mental disorder. Diagnostic and statistical manual of mental disorders
- 2. · The DSM-IV-TR is a taxonomy published by the APA. The DSM-IV-TR describes all mental disorders, outlining specific criteria for each based on clinical experience and research. · The DSM-IV-TR has 3 purposes: o To provide standardized nomenclature and language for all mental health professionals. o To present defining characteristics or symptoms that differentiates specific diagnoses. o To assist in identifying the underlying causes of disorders. · A multiaxial classification system that involves assessment on several axes, or domains of information, allows the practitioner to identify all the factors that relate to a persons condition. o Axis I is for identifying all major psychiatric disorders except MR and personality disorders. Examples include depression and schizophrenia. o Axis II is for reporting mental retardation and personality disorders as well as prominent maladaptive personality features and defense mechanisms. o Axis III is for reporting current medical conditions that are potentially relevant to understanding or maintaining the person’s mental disorder as well as medical conditions that might contribute to understanding the person. o Axis IV is for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders. Included are problems with the primary support group, the social environment, education, occupation, housing, economics, access to health care, and the legal system. o Axis V presents a Global Assessment of Functioning which rates the person’s overall psychological functioning on a scale of 0 to 100. This represents the clinician’s assessment of the person’s current level of functioning.
- 3. · All clients admitted to a hospital or psychiatric treatment will have a multiaxis diagnosis from the DSM-IV- TR. Period of Enlightenment and Creation of Mental Institutions · In the 1790’s Phillippe Pinel in France and Willian Tukes of England formulated the concept of asylum as a safe refugee or haven offering protection at institutions where people had been beaten, whipped, and starved for their mental illness. · In the US, Dorothea Dix (1802-1887) began a crusade to reform the treatment of mental illness after a visit to the Tukes’ institution in England. She was instrumental in opening 32 state hospitals that offered asylum to the suffering. · 100 years after establishment of the first asylum, state hospitals were in trouble. Attendants were accused of abusing the residents, the rural locations of the hospitals were viewed as isolating patients from their families and homes, and the phrase insane asylum took on a negative connotation. Development of Psychopharmacology · In the 1950’s the development of psychotropic drugs were used to treat mental illness. · Chlorpromazine (Thorzine), an antipsychotic drug, and lithium, an anti-manic agent, were the first drugs to be developed. · 10 years later, monoamine oxidase inhibitors, haloperidol (Haldol), an antipsychotic; tricyclic antidepressants; and antianxiety agents (benzodiazepines), were introduced.
- 4. · Because of these new drugs, hospital stays were shortened, and many people were well enough to go home. Move toward Community Mental Health · The enactment of the Community Mental Health Centers Act came about in 1963. · Deinstitutionalization, a deliberate shift from institutional care in state hospitals to community facilities, began. · In addition to deinstitutionalization, federal legislation was passed to provide an income for disabled persons: SSI and SSDI. This allowed people with mental illnesses to be more independent financially and not to rely on family for money. Mental Illness in the 21st Century · The Department of Health and Human Services (DHHS) estimates that 56 million Americans have a diagnosable mental illness. · The term Revolving door effect is used to explain how people with severe and persistent mental illness have shorter hospital stays, but they are admitted more frequently. People with severe and persistent mental illness may show signs of improvement in a few days but are not stabilized. Thus, they are discharged into the community without being able to cope with community living. Substance abuse issues cannot be dealt with in the 3-5 days typical for admissions in the current managed care environment. · Many providers believe today’s clients are to be more aggressive than those in the past. Between 4% and 8% in clients seem in Psychiatric ER’s are armed. People
- 5. not receiving adequate mental health care commit about 1,000 homicides each year. · In state prisons, 1 in 10 prisoners take psychotropic medications and 1 in 8 receives counseling or therapy for mental health issues. · 85% of the homeless population has a psychiatric illness and/or a substance abuse problem. · The United States has the largest percentage of mentally ill citizens (29.1%) and provided care for only 1 in 3 people who needed it (Bijl et al., 2003). · Persons with minor or mild cases are most likely to receive treatment while those with severe and persistent mental illness were least likely to be treated. Cost containment and managed care · Managed Care is a concept designed to purposely control the balance between the quality of care provided and the cost of that care. In a managed care system, people receive care based on need rather than request. · Case management or management of care on a case-by- case basis represented an effort to provide necessary services while containing costs. The client is assigned a case manager, a person who coordinates all types of care needed by the client. · In 1996, Congress passed the Mental Health Parity Act, which eliminated annual and lifetime dollar amounts for mental health care for companies with more than 50 employees. However, substance abuse was not covered by this law, and companies could limit the number of days in the hospital or the number of clinic visits per year. Thus, parity did not really exist. Psychiatric Nursing Practice
- 6. · In 1873, Linda Richards improved nursing care in psychiatric hospitals and organized educational programs in state mental hospitals in Illinois. Richards is called the first American psychiatric nurse. · The first training of nurses to work with persons with mental illness was in 1882. The care focused on nutrition, hygiene and activity. Nurses adapted medical-surgical principles to the care of clients with psychiatric disorders and treated them with tolerance and kindness. · Treatments such as insulin shock therapy (1935), psychotherapy (1936), and electroconvulsive therapy (1937) required nurses to use their medical skills more extensively. · John Hopkins was the first school of nursing to include a course on psychiatric nursing in its curriculum. · In 1950, the National League for Nursing (which accredits nursing programs) required schools to include an experience in psychiatric nursing. · In 1973, the ANA developed Standards of care, which states the responsibilities for which nurses are accountable. · Psychiatric nursing practice has been profoundly influenced by Hildegard Peplau and June Mellow, who wrote about the nurse-client relationship, anxiety, nurse therapy, and interpersonal nursing therapy. Psychiatric Mental Health Nursing Phenomena of Concern · The maintenance of optimal health and well-being and the prevention of psychobiologic illness. · Self-care limitations or impaired functioning related to mental and emotional distress. · Deficits in the functioning of significant biologic, emotional, and cognitive symptoms. · Emotional stress or crisis components if illness, pain, and disability.
- 7. · Self-concept changes, developmental issues, and life process changes. · Problems related to emotions such as anxiety, anger, sadness, loneliness, and grief. · Physical symptoms that occur along with altered psychological functioning. · Alterations in thinking, perceiving, symbolizing, communicating, and decision making. · Difficulties relating to others · Behaviors and mental states that indicate the client is a danger to self or others or has a significant disability. · Interpersonal, systemic, sociocultural, spiritual, or environmental circumstances or events that affect the mental or emotional well-being of the individual, family, or community. · Symptom management, side effects/toxicities associated with psychopharmacologic intervention, and other aspects of the treatment regimen. Standards of Psychiatric mental health clinical nursing practice. · Standard I. Assessment o The psychiatric-mental health nurse collects health data · Standard II. Diagnosis o The psychiatric-mental health nurse analyzes the data in determining diagnoses. · Standard III. Outcome identification. o The psychiatric-mental health nurse identifies expected outcomes individualized to the client. · Standard IV. Planning. o The psychiatric-mental health nurse develops a plan of care that prescribes interventions to attain expected outcomes. · Standard V. Implementation o The psychiatric-mental health nurse implements the interventions identified in the plan of care.
- 8. · Standard Va. Counseling o The psychiatric-mental health nurse uses counseling interventions to assist clients in improving or regaining their previous coping abilities, fostering mental health, and preventing mental illness and disability. · Standard Vb. Milieu Therapy o The psychiatric-mental health nurse provides structures, and maintains a therapeutic environment in collaboration with the client and other health care practitioners. · Standard Vc. Self-care activities. o The psychiatric-mental health nurse structures interventions around the client’s activities of daily living to foster self-care and mental and physical well-being. · Standard Vd. Psychobiologic Interventions. o The psychiatric-mental health nurse uses knowledge of psychobiologic interventions and applies clinical skills to restore the client’s health and prevent further disability. · Standard Ve. Health teaching. o The psychiatric-mental health nurse, through health teaching, assists clients in achieving, satisfying, productive, and healthy patterns of living. · Standard Vf. Case Management. o The psychiatric-mental health nurse provides case management to coordinate comprehensive health services and ensure continuity of care. · Standard Vg. Health promotion and maintenance. o The psychiatric-mental health nurse employs strategies and interventions to promote and maintain mental health and prevent illness. Areas of practice · Counseling
- 9. o Interventions and communication techniques o Problem solving o Crisis intervention o Stress management o Behavior modification · Milieu therapy o Maintain therapeutic environment o Teach skills o Encourage communication between clients and others o Promote growth through role modeling · Self-care activities o Encourage independence o Increase self-esteem o Improve function and health · Psychobiologic interventions o Administer medications o Teaching o Observations · Health teaching · Case management · Health promotion and maintenance Advanced level functions · Psychotherapy · Prescriptive authority for drugs (in many states) · Consultation · Evaluation Self-awareness issues · Self-awareness is the process by which the nurse gains recognition of his or her own feelings, beliefs, and attitudes.
- 10. Chapter Two Neurobiologic Theories and Psychopharmacology The Nervous system and how it works · The cerebrum is the center for coordination and integration of all information needed to interpret and respond to the environment. · The cerebellum is the center for coordination of movements and postural adjustments. · The brain stem contains centers that control cardiovascular and respiratory functions, sleep, consciousness, and impulses. · The limbic system regulates body temperature, appetite, sensations, memory, and emotional arousal. Neurotransmitters · Neurotransmitters are the chemical substances manufactured in the neuron that aid in the transmission of information throughout the body. o They either excite or stimulate an action in the cells (excitatory) or inhibit or stop an action (inhibitatory). o After neurotransmitters are released into the synapse (point of contact between the dendrites and the next neuron) and relay the message to the receptor cells, they are either transported back from the synapse to the axon to be stored for later use (reuptake) or are metabolized and inactivated by enzymes, primarily monoamine oxidase (MAO).
- 11. · Dopamine, a neurotransmitter located primarily in the brain stem. Dopamine is generally excitatory and is synthesized from tyrosine, a dietary amino acid. o Antipsychotic medications work by blocking dopamine receptors and reducing dopamine activity. · Norepinephrine and Epinephrine o Norepinephrine, the most prevalent neurotransmitter, is located primarily in the brain stem. It plays a role in mood regulation. o Epinephrine is also known as noradrenaline and adrenaline. Epinephrine has limited distribution in the brain but controls the fight-or-flight response in the peripheral nervous system. · Serotonin o A neurotransmitter found only in the brain, is derived from tryptophan, a dietary amino acid. o The function of serotonin is mostly inhibitory, involved in the control of food intake, sleep and wakefulness, temperature regulation, pain control, sexual behavior, and regulation of emotions. o Some antidepressants block serotonin reuptake, thus leaving it available longer in the synapse, which results in improved mood. · Histamine o The role of histamine in mental illness is under investigation. · Acetylcholine o Acetylcholine is a neurotransmitter found in the brain, spinal cord, and peripheral nervous system. It can be excitatory or inhibitory. It is synthesized from dietary choline found in red meat and vegetables and has been found to affect the sleep-wake cycle and to signal muscles to become active. o Studies have shown that people with Alzheimer’s disease have decreased acetylcholine secreting neurons. · Glutamate
- 12. o Glutamate is an excitatory amino acid that at high levels can have major neurotoxic effects. · Gamma-Aminobutyric Acid (GABA) o GABA is a major inhibitory neurotransmitter in the brain and has been found to modulate other neurotransmitter systems rather than to provide a direct stimulus. o Drugs that increase GABA function such as benzodiazepines are used to treat anxiety and to induce sleep. Neurobiologic causes of mental illness · Current theories and studies indicate that several mental disorders may be linked to a specific gene or combination of genes but that the source is not solely genetic; nongenetic factors also play important roles. · Two genetic links to Alzheimer’s disease are chromosomes 14 and 21. · The Human Genome Project, funded by NIH and the US Department of Energy, is the largest of its kind. It has identified all human DNA. In addition, the project also addresses the ethical, legal, and social implications of human genetics research. Stress and the Immune system (Psychoimmunology) · This is a relatively new field of study, which examines the effect of psychological stressors on the body’s immune system. Infection as a possible cause
- 13. · Some researchers are focusing on infection as a cause of mental illness. Studies such as this are promising in discovering a link between infection and mental illness. The Nurse’s role in research and education · The nurse must ensure that client’s and families are well informed about progess in these areas and must also help them to distinguish between facts and hypotheses. The nurse can explain if or how new research may affect a client’s treatment or prognosis. The nurse is a good resource for providing information and answering questions. Psychopharmacology · Efficacy refers to the maximal therapeutic effect that a drug can achieve. · Potency describes the amount of the drug needed to achieve that maximum effect; low-potency drugs require higher doses to achieve efficacy, whereas high-potency drugs achieve efficacy at lower doses. · Half Life is the time it takes for half of the drug to be removed from the bloodstream. Drugs with shorter half-life may need to be given three or four times a day, but drugs with a longer half-life may be given once a day. · The FDA may issue a black-box warning when a drug is found to have serious or life-threatening side effects. This means that package inserts must have a highlighted box, separate from the text, which contains a warning about the serious side-effects. Antipsychotic drugs
- 14. · Also known as neuroleptics, are used to treat the symptoms of psychosis, such as the delusions and the hallucinations seen in schizophrenia, schizoaffective disorder, and the manic phase of bipolar disorder. · Antipsychotic’s work by blocking receptors of the neurotransmitter, dopamine. · Dopamine receptors are classified into subcategories (D1, D2, D3, D4, and D5) and D2, D3, and D4 have been associated with mental illness. · The typical antipsychotic drugs are potent antagonists (blockers) of D2, D3, and D4. This makes them effective in treating target symptoms but also produces many extrapyramidal side effects because of the blocking of the D2 receptors. · Newer, atypical antipsychotic drugs such as clozapine (Clozaril) are relatively weak blockers of D2, which may account for the lower incidence of extrapyramidal side effects. · The newer antipsychotics also inhibit the reuptake of serotonin, increasing their effectiveness in treating the depressive aspects of schizophrenia. Extrapyramidal Side Effects · (EPS) are the major side effects of antipsychotic drugs. They include acute dystonia (prolonged involuntary muscular contractions that may cause twisting of the body parts, repetitive movements, and increased muscular tone), pseudoparkinsonism, and akathisia (intense need to move about). Blockage of the D2 receptors in the midbrain region of the brain stem is responsible for the development of EPS. Included in the EPS are: o Torticollis : twisted head and neck o Opisthotonus : tightness of the entire body with head back and an arched neck.
- 15. o Oculogyric crisis : eyes rolled back in a locked position. · Immediate treatment with anticholinergic drugs usually brings rapid relief. · Pseudoparkinsonism , or drug-induced Parkinsonism if often referred to by the generic label of EPS. Symptoms include a stiff, stooped posture; mask-like facies; decreased arm swing; a shuffling. festinating gait; drooling; tremor; bradycardia; and coarse pill rolling movements of the thumb and fingers while at rest. · Treatment of these symptoms can include adding an anticholinergic agent or amantadine, which is a dopamine agonist that increases transmission of dopamine blocked by the antipsychotic drug. Neuroleptic Malignant syndrome · (NMS) is a potentially fatal idiosyncratic reaction to an antipsychotic. Death rates have been reported at 10% to 20%. · Symptoms include rigidity, high fever; autonomic instability such as unstable blood pressure, diaphoresis, and pallor; delirium; and elevated levels of enzymes, particularly creatine and phosphokinase. · Clients with NMS are confused and often mute; they may fluctuate from agitation to stupor. · Dehydration, poor nutrition, and concurrent medical illness all increase the risk of NMS. · Treatment includes immediate discontinuation of the antipsychotic and the institution of supportive medical care to treat dehydration and hyperthermia. Tardive Dyskinesia
- 16. · (TD) is a syndrome of permanent involuntary movements. This is most commonly caused by the long-term use of antipsychotic drugs. · There is no treatment available. · The symptoms of TD include involuntary movements of the tongue, facial, and neck muscles, upper and lower extremities, and truncal musculature. Tongue thrusting and protruding, lip smacking, blinking, grimacing, and other excessive unnecessary facial movements are characteristic. · One TD has developed, it is irreversible. Agranulocytosis · Some antipsychotics produces agranulocytosis. This develops suddenly and is characterized by: o Fever o Malaise o Ulcerative sore throat o Leucopenia · The drug must be discontinued immediately if the WBC drops by 50% or to less that 3,000. Antidepressant drugs · Although the mechanism of action is not completely understood, antidepressants somehow interact with the two neurotransmitters, norepinephrine and serotonin. · Antidepressants are divided into four groups: o Tricyclic and the related cyclic antidepressants o Selective serotonin reuptake inhibitors (SSRIs) o MAO inhibitors (MAOIs) o Other antidepressants such as venlafaxine (Effexor), bupropion (Wellbutrin), duloxetine (Cymbalta), trazodone (Desyrel), and nefazodone (Serzone).
- 17. · MAOIs have a low incidence of sedation and anticholinergic effects, they must be used with extreme caution for several reasons: o A life-threatening side effect, hypertensive crisis, may occur if the client ingests food containing tyramine (an amino acid) while taking MAOIs. Mature or aged cheeses Aged meats (sausage, pepperoni) Tofu ALL tap beers and microbrewery beer. Sauerkraut, soy sauce, or soybean condiments Yogurt, sour cream, peanuts, MSG o MAOIs cannot be given in combination with other MAOIs, tricyclic antidepressants, Demerol, CNS depressants, and hypertensives, or general anesthetics. o MAOIs are potentially lethal in overdose and pose a potential risk for clients with depression who may be considering suicide. · SSRIs, venlafaxine, nefazodone, and bupropion are often better choices for those who are potentially suicidal or highly impulsive because they carry no risk of lethal overdose in contrast to the cyclic compounds and the MAOIs. However, SSRIs are only effective for mild to moderate depression. · The major actions of antidepressants are with the monoamine neurotransmitter systems in the brain, particularly norepinephrine and serotonin. o Norepinephrine, serotonin, and dopamine are removed from the synapses after release by reuptake into presynaptic neurons. After reuptake, these three neurotransmitters are reloaded for subsequent release or metabolized by the enzyme MAO. o The SSRIs block the reuptake of serotonin; the cyclic antidepressants and venlafaxine block the reuptake of norepinephrine primarily and block
- 18. serotonin to some degree; and the MAOIs interfere with enzyme metabolism. Mood stabilizing drugs · Mood stabilizing drugs are used to treat bipolar disorder by stabilizing the client’s mood, preventing or minimizing the highs and lows that characterize bipolar illness, and treating acute episodes of mania. · Lithium is considered the first-line agent in the treatment of bipolar disorder. o Lithium normalizes the reuptake of certain neurotransmitters such as serotonin, norepinephrine, acetylcholine, and dopamine. It also reduces the release of norepinephrine through competition with calcium. o Lithium produces its effects intracellularly rather than within neuronal synapses. o Lithium serum levels should be about 1.0 mEq/L. Levels less than 0.5 mEq/L are rarely therapeutic, and levels of more than 1.5 mEq/L are usually considered toxic. o If Lithium levels exceed 3.0 mEq/L, dialysis may be indicated. · The mechanism of action for anticonvulsants is not clear as it relates to their off-label use as mood stabilizers. o Valporic acid and topiramate are known to increase the levels on the inhibitatory neurotransmitter, GABA. Both are thought to stabilize mood by inhibiting the kindling process. The kindling process can be described as the snowball-like effect seen when minor seizure activity seems to build up into more frequent and severe seizures. In seizure management, anticonvulsants raise the level of the threshold to prevent these minor seizures. It is suspected that this same kindling process
- 19. may occur in the development of full-blown mania with stimulation by more frequent, minor episodes. Antianxiety drugs (Anxiolytics) · Benzodiazepines mediate the actions of the amino acid GABA, the major inhibitory neurotransmitter in the brain. Because GABA receptor channels selectively admit the anion chloride into neurons, activation of GABA receptors hyperpolarizes neurons and thus is inhibitory. · Benzodiazepines produce their effects by binding to a specific site on the GABA receptor. Stimulants · Today, the primary use of stimulants is for ADHD in children and adolescents, residual attention deficit disorder in adults, and narcolepsy. · Stimulants are often termed indirectly acting amines because they act by causing release of the neurotransmitters (norepinephrine, dopamine, and serotonin) from presynaptic nerve terminals as opposed to having direct agonist effects on the postsynaptic receptors. They also block the reuptake of these neurotransmitters. · By blocking the reuptake of these neurotransmitters into neurons, they leave more of the neurotransmitter in the synapse to help convey electrical impulses in the brain. Cultural considerations
- 20. · I’m not going to go much into this. Just know that clients from various cultures may metabolize medication at different rates and therefore require alterations in standard dosages. Psychosocial Theories and Therapy Sigmund Freud, the Father of Psychoanalysis · Founded the personality components; Id, Ego, and Superego o Id: The part of ones nature that reflects basic or innate desires such a pleasure seeking behavior, aggression, and sexual impulses. The id seeks instant gratification, causes impulsive thinking behavior, and has no rules or regard for social convection. o Superego: The part of ones nature that reflects moral and ethical concepts, values, parental and social expectations; therefore, it is the directional opposite to the id. o Ego: The balancing or mediating force between the id and the superego. The ego represents mature and adaptive behavior that allows a person to function successfully. · Psychosexual development o Oral (birth to 18 months) o Anal (18 to 36 months) o Phallic/Oedipal (3 to 5 years) o Latency (5 to 11 or 13 years) o Genital (11 or 13 years) · Transference and Countertranference o Transference occurs when the client onto the therapist/nurse attitudes and feelings that the client previously felt in other relationships. o Countertranference occurs when the therapist/nurse displaces onto the client attitudes or feelings from his or her past.
- 21. Developmental Theorists; Erikson and Piaget · Erikson focused on personality development across the life span while focusing on social and psychological development in life stages. o Trust vs. Mistrust (infant) o Autonomy vs. Shame and Doubt (toddler) o Initiative vs. guilt (preschool) o Industry vs. Inferiority (school age) o Identity vs. Role confusion (adolescence) o Intimacy vs. isolation (young adult) o Generativity vs. stagnation (middle adult) o Ego integrity vs. despair (maturity) · Erikson believed that psychosocial growth occurs in sequential stages, and each stage is dependent on the completion of the previous stage/life task. · Piaget explored how intelligence and cognitive functioning develop in children. o Sensorimotor (birth to 2 years): The child develops a sense of self as separate from the environment and the concept of object permanence. Begins to form mental images. o Preoperational (2-6 years): Child begins to express himself with language, understands the meaning of symbolic gestures, and begins to classify objects. o Concrete operations (6-12 years): Child begins to apply logical thinking, understands reversibility, is increasingly social and able to apply rules; however, thinking is still concrete. o Formal operations (12 to 15 years and beyond): Child learns to think and reason in abstract terms, further develops logical thinking and reasoning, and achieves cognitive maturity. Harry Stacks Sullivan: Interpersonal Relationships and Milieu therapy · The importance and significance of interpersonal relationships in one’s life was Sullivan’s greatest contribution to the field of mental health.
- 22. · Sullivan developed the first therapeutic community or milieu with young men with schizophrenia in 1929. He found that within the milieu, the interactions among clients were beneficial, and then the treatment should emphasize on the roles of the client-client interaction. o Milieu therapy is used in the acute care setting; one of the nurses’ primary roles is to provide safety and protection while promoting social interaction. Hildegard Peplau: Therapeutic nurse-patient relationship (The bomb-diggity of nursing) · Developed the concept of the therapeutic nurse-patient relationship, which includes 4 phases: orientation, identification, exploitation, and resolution. o The orientation phase is directed by the nurse and involves engaging the client in treatment, providing explanations and information, and answering questions. During this time the nurse would orient the patient to the rules and expectations (if in an acute setting). o The identification phase begins when the client works interdependently with the nurse, expresses feelings, and begins to feel stronger. This phase can begin either within a few hours to a few days; the patient can identify the nurse and environment on his own. They “come together”. Kinky. o In the exploitation phase, the client makes full use of the services offered. He moves toward independence. o In the resolution phase, the client no longer needs professional services and gives up dependent behavior. o Keep in mind that after the resolution phase, the client can regress and move back into the above mentioned phases. · Paplau defined anxiety as the initial response to a psychic threat, describing 4 levels of anxiety: acute, moderate, severe, and panic. o Acute anxiety is a positive state of heightened awareness and sharpened senses, allowing the person to learn new behaviors and solve problems. The person can take in all available stimuli (perceptual field).
- 23. o Moderate anxiety involved a decreased perceptual field (focus on immediate task only); the person can learn new behavior or solve problems only with assistance. Another person can redirect the person to the task. Remember, this is the ideal anxiety state for teaching a client regarding health concerns such as diabetes, as Cathy says so. o Severe anxiety involves feelings of dread or terror. The person CANNOT be redirected to a task; he focuses only on scattered details and has physiologic symptoms such as tachycardia, diaphoresis, and chest pain. The client may go to the ER thinking he is having a heart attack. In lecture, Cathy stated that this person can still be “talked down”. The first priority is to move the person away from all stimuli, and then attempt to talk with them to calm down. o Panic anxiety can involve loss of rational thought, delusions, hallucinations, and complete physical immobility and muteness. The person my bolt and run aimlessly, often exposing himself and others to injury. Humanistic Theories; Maslow’s Hierarchy of needs. · Everyone should know this one. It is outlined on page 56 in your book. · He used a pyramid to arrange and illustrate the basic drives or needs to motivate people. o The most basic needs, physiologic needs, need to be met first. This includes food, water, shelter, sleep, sexual expression, and freedom of pain. These MUST be met first. o The second level involves safety and security needs, which involve protection, security, freedom from harm or threatened deprivation. o The third level is love and belonging needs, which include enduring intimacy, friendship, and acceptance. o The fourth level involves esteem needs, which includes the need for self-respect and esteem from others. o The highest level is self-actualization, the need for beauty, truth, and justice. Few people actually become self-actualized.
- 24. o Remember, traumatic life experiences or compromised health can cause a person to regress to a lower level of motivation. Pavlov: Classic conditioning (Behavior theory) · Pavlov believed that behavior can be changed through conditioning with external or environmental conditions or stimuli. Crisis Intervention · Maturational crises, sometimes called developmental crises, are predictable events in the normal course of a life, such as leaving home for the first time, getting married, having children, etc. · Situational crises are unanticipated or sudden events that threaten an individuals integrity; such as a death of a loved one and loss of a job. · Adventitious crises, sometimes called social crises, include natural disasters like floods, earthquakes, or hurricanes; war, terrorist attacks; riots; and violent crimes such as rape or murder. Non-violent crisis intervention The heart of crisis intervention is: · Care · Welfare · Safety (#1!) · Security People in crisis need care and welfare.
- 25. Staff responses should be safety and security. Anxiety: · Increase or change in behavior. Can be anything different from usual behavior (excitement, pacing). · Nursing interventions: o Ask “What’s going on?” o Give supportive care and let the patient know that you’re there. Defensive: · Loss of rationality. · Nursing interventions: o Direct approach to setting limits. o Take away privileges. o Give the patient some control and choices. Acting out person: · Loss of rational control. · Nursing interventions: o Everything Cathy showed us on non-violent physical crisis intervention Tension-Reduction: · Subsiding of energy. · Nursing interventions: o Establish therapeutic rapport o Prime time to talk and teach about preventions of behavior.
- 26. What if the patient simply refuses? · Set limits! · Make the limits reasonable and enforceable. Releasing… Venting… Mad as heck! · Allow the patient to do this! · Just stay calm as a nurse · While they’re venting, they’re also releasing. This is a good thing. Intimidation: · This is NOT A GOOD THING. · What if the patient tells you…? o I know what car you drive. o I know your last name. o I know you have 2 dogs and I’m going to kill them. · Nursing interventions: o Get a witness! Do not be by yourself with this patient! Non-verbal behavior that affect proxemics · Factors that affect: o Size, gender, disability, environment, agitation, history, and speed. · 18-36” is personal space (usually how wide ones arm length is). · Always be the closest to the door.
- 27. Kinesics (Body language) · Facial expressions, stance, posture, breathing, hand gestures · When approaching a client, stand at 45 degree angle · Stand with hands to side (especially when with a paranoid client) · Move when the patient moves. · Be as calm as possible. Paraverbal communication · 55% nonverbal · 7% verbal · 38% paraverbal it’s not what you say; it’s how you say it! · TVC (total voice control) o Tone o Volume o Cadence Always remember not to lose eye contact. If you’re being grabbed… · Gain physiologic advantage o Know where the weak point of grab is o Leverage- use what you have! o Momentum—it comes in handy · Gain psychological advantage o Stay calm o Have a plan o Don’t forget the element of surprise
- 28. Non-Violent physical control and restraint should be used as a LAST RESORT. Mood disorders Categories of Mood disorders · Unipolar o Major depression · Bipolar o Mania o Depression o Period of normalcy Unipolar: Major depression · Sad mood or lack of interest in life for 2 or more weeks · Another 4 symptoms must also be present o Change in appetite (increase or decrease) o Change in sleep patterns (too much or too little) o Unable to concentrate and make decisions o Loss of self-esteem (guilt- how you were raised; how worthy a person perceives themselves). · Those at risk: o PMS/PMDD o Suffering from anxiety and irritability o PP depression o Chronic illness (dialysis) o PTSD o Grief and loss · Can be observed by others, or the depression is just in one’s “head”
- 29. Incidence · Major depression occurs at least twice as often in women · Single and divorced people have the highest rates of depression Treatments · Psychotherapy (groups, counselor) · Psychopharmacology (Meds) · ECT Electroconvulsive therapy · The biggest concern is memory loss. · Patient is pre-medicated, much like a pre-op patient · Elders are treated for depression with ECT more frequently than younger persons. o Elder persons have increased intolerance of side effects of antidepressants o ECT produces a more rapid response Suicidal Ideation · Safety is primary concern · Watch for overt cues of suicide (Obvious) active · Covert cues are more subtle—passive · People who suddenly are happier are of great concern; may have made the suicidal plan are content with their decision. · People whose meds are finally working—have enough energy to carry out the act
- 30. Client’s Affect · Compare verbal with non-verbal behaviors—do they match up? · Asocia l: Withdrawal from family and friends · Anhedonic : Lose sense of pleasure · When confronting these client’s about their behavior, use “I” statements o “I really wish you’d join the group” Judgment · Feel overwhelmed with normal activities · Difficulty with task completion · Always exhausted Self Concept · Ruminate : Worry to excess. · Lack energy for normal activities (always tired) Interventions · Assess safety for client (PRIORITY!) · Perform suicide lethality assessment · Orient client to new surroundings (they need structure) · Offer explanations of unit routine (again, need structure) · Start to promote a therapeutic relationship; schedule short interaction times. Patient and Family teaching
- 31. · Stress importance of follow-up care—keep it structured; make appointment for them. · Stress importance of continuing medications; assess if they can afford them · Make phone number lists of how to get help if they need it. Bipolar disorder · Condition with cyclic mood changes · Person has manic episodes, periods of profound depression, and times of normal behavior in-between · Occurs equally in men and women; often seen in highly educated people. Clinical course of mania · Episode of unusual, grandiose, or agitated mood lasting at least one week with three or more of the following symptoms: o Exaggerated self-esteem o Sleeplessness o Pressured speech o Flight of ideas o Reduced ability to filter out stimuli o Distractibility o More activities with increased energy Drug treatment · Lithium o Lithium is not metabolized; rather, it is reabsorbed by the proximal tubule and excreted in the urine. o Thought to work in the synapse to increase destruction of dopamine and norepinephrine;
- 32. decreases sensitivity to postsynaptic receptors (Basically- when a person is in a manic phase, they are synapsing super fast. Lithium helps slow this synapsing down). o Onset of action is 5-14 days; other drugs must be used during the acute phases to reduce symptoms of mania or depression. o Maintenance lithium level is 0.5-1.0 mEq/L. 3 is toxic! Duh. o Lithium is a salt contained in the human body. It not only competes for salt receptor sites but also affects calcium, potassium, and magnesium ions as well as glucose metabolism. MUST complete an electrolyte blood panel (focus on Chloride). o Having too much salt in the diet can cause the lithium level to be too low. o Not having enough dietary salt can cause the lithium levels to be too high. o Persistent thirst and diluted urine can indicate the need to call the MD; lithium dosage may need to be reduced. · Anticonvulsant drugs: mechanism is unclear, but they raise the brains threshold for dealing with stimulation; this prevents the person from being bombarded with external and internal stimuli. o Tegretol Huge concern about agranulocytosis (a decrease in WBC). Need serum levels monitored 12 hours after last dose. o Depakote Need to monitor serum level, CBC with platelets, liver function including ammonia level (ammonia is a by-product of liver metabolism) o Klonopin Anticonvulsant and benzodiazepine Drug dependence can occur
- 33. Monitor CBC, liver function Withdrawal drug slowly to prevent GI issues Cannot be used alone to manage bipolar; must be used in conjunction with lithium or another mood stabilizer. Helpful hints to care for bipolar clients · You can’t teach a manic client · Safety is a huge issue because their judgment is poor. · Only spend short periods of time with patient · Must be flexible in taking intake assessment; may need to obtain data in several short sessions as well as talking to family members. · Ask the client to explain any coded speech · Assist the client to meet socially accepting behaviors. “Kathy, you are too close to my face. Please stand back two feet.” · Feed them finger foods high in calories while in a manic phase; provide nutritional support! · Use simple sentences when communicating. It is also helpful to ask client to repeat brief messages to ensure they have heard and incorporated them. o “Please speak more slowly. I’m having trouble following you.” · Avoid becoming involved in power struggles over who will dominate the conversation. Suicide · 4 out of 5 who actually commit suicide have made at least one prior attempt · In a majority of cases, there are clear indicators hat the person was very troubled. · Few than 15% of suicide victims leave suicide notes
- 34. · The suicide risk is greatest in the 90 days following a major depressive episode. · “survivor guilt” happens when 1 or more family members feel guilty that they are still living · “Separation anxiety” may cause they surviving to “join the beloved deceased” · Make the patient sign a “contract for life” · Crisis intervention—may need 1:1 care. The client is no more than 2-3 feet away from a staff member at any time, including going to the bathroom. Anxiety disorders & Substance abuse Incidence · Most common emotional disorder in the U.S. · Prevalent in women; age <45 Physiologic responses · Flight or fight responses · Sympathetic fibers increase the vital signs · Adrenal glands release adrenalin which causes the body to: o Take in more oxygen o Dilate the pupils (brings more light into eyes; better vision) o Increase the arterial blood pressure and heart rate o Constrict peripheral vessels (makes skin cool and pale) o Increase glycogenolysis to free glucose for fuel (glycogen is being broken down in the liver) o Shunt blood from GI and reproductive organs
- 35. Psychological response · Difficulty with logical thought · Increased agitation with motor activity · Increased vital signs · Client will try to change the feelings of discomfort by: o Changing behavior by adaptation o Changing behavior with defense mechanisms Anxiety disorders · Panic disorder · Phobic disorder · Agoraphobia · Obsessive-compulsive · PTSD · Generalized anxiety · Anxiety related to medical conditions · Substance-induced anxiety disorder Development of Anxiety Disorders · Predisposing factors o Onset: Acute or insidious (builds up) o Precipitating event o Chronic stressors o Unusual behavior o Fears disproportionate to reality Levels of anxiety · Mild:
- 36. o Psychological: Wide perceptional field, sharpened senses, increased motivation, effective problem solving, increased learning ability, irritability. o Physiologic: Restlessness, fidgeting, “butterflies”, difficulty sleeping, hypersensitivity to noise. · Moderate: o Psychological: perceptual field narrowed to immediate task, selectively attentive, cannot connect thoughts or events independently, increased use of automatisms o Physiologic: Muscle tension, diaphoresis, pounding pulse, HA, dry mouth, high voice pitch, faster rate of speech, GI upset, frequent urination · Severe: o Psychological: Perceptual field narrowed to one detail or scattered details; cannot complete tasks; cannot solve problems or learn effectively; behavior geared toward anxiety relief and is usually ineffective; doesn’t respond to redirection; feels awe, dread, or horror; cries; ritualistic behavior. o Physiologic: Severe HA, N/V, diarrhea, rigid stance, vertigo, pale, tachycardia, chest pain. · Panic: o Psychological: Perceptual field reduced to focus on self; cannot process any environmental stimuli; distorted perceptions; loss of rational thought; doesn’t recognize potential danger; can’t communicate verbally; possible delusions or hallucinations; may be suicidal. o Physiologic: May bolt and run OR totally immobile and mute; dilated pupils, increased blood pressure and pulse; flight, fright, or freeze. Seyle Response to stress · Alarm reaction o Physiologic response
- 37. o Body prepares to defend itself · Resistance stage o Body will defend by flight or fight o If the stress is gone; body relaxes · Exhaustion stage o Negative response to anxiety and stress o Body stores are depleted Panic disorders · An episode lasting 15-30 minutes in which a client experiences rapid, intense, escalating anxiety; great emotional discomfort; and physiologic discomfort. · Defined as recurrent, unexpected panic attacks followed by a month of persistent concern or worry about having another attack. · 75% with panic disorder have spontaneous attacks with no triggers · Others have attacks stimulated by phobias or chemical changes within the body. Treatment · Psychotherapy o Positive reframing o Assertiveness training · Psychopharmacology o SSRIs o Anxiolytics o Antidepressants o MAOIs Phobias
- 38. · An illogical, intense, persistent fear of a specific object or social situation that causes extreme distress and interferes with having a normal life. · Treatment for phobias: o Psychopharmacology Anxiolytics Benzodiazepines SSRIs Beta Blockers o Psychotherapy Behavioral therapy Systemic desensitization “Flooding” Getting rid of fear all at one time Obsessive-Compulsive Disorder (OCD) · Obsessions: Recurrent thoughts, ideas, visualizations, or inappropriate impulses that disturb a person’s life; has no control over them. · Compulsions: Behaviors or rituals continuously carried out to get rid of the obsessive thoughts and reduce anxiety. · Higher incidence with groups in higher economic status and with more education · Nursing interventions: o Remember, a lot of the time people feel guilty about their thoughts and behaviors. o Do not try to stop the act unless the act is harmful (dangerous) o Talk to them! Use “I” statements o If they are too down on themselves—limit your time with them. For instance, “I hate myself. No one cares about me. I’m fat and ugly.” The nurse would then say, “I am going to come back in 30 minutes. In that time frame, I want you to think of your good qualities.” o Do not argue with OCD person.
- 39. o Inject reality. If a teenager thinks she is pregnant despite a negative pregnancy test, tell her the TEST IS NEGATIVE. Take them back into reality. o If they repetitively do an act over and over again; help them set a goal. For instance, “Let’s try to only wash your hands once every ten minutes.” Post Traumatic Stress disorder · Three clusters if symptoms are present o Reliving the event Memories, dreams, or flashbacks o Avoiding reminders of the event Staying away from any stimuli that could be associated with the trauma. o Being on guard (hyper-arousal) Less responsive to stimuli Insomnia, irritability, or angry outbursts · At risk people include: o Combat veterans o Victims of violence o Abused victims o Children in traffic accident (and the parents) Only 46% of parents sought help for their children. KIDS NEED HELP. · Symptoms of PTSD occur 3 months or more after the trauma. · Some more signs of PTSD: o Have issues with authority figures o Their first emotions are anger, rage, and guilt o Their guilt comes out as anger (violent behavior) o Isolate themselves o Cry o Don’t want to talk about it o Drug and alcohol abuse o Nightmares o Manifests in physiological symptoms (HA, GI distress)
- 40. o Irritable o Insomnia · Nursing interventions: o Have specific staff members assigned to client to facilitate building trust o Consistency is the key o Be non-judgmental; encourage client to talk o Help them acknowledge where grief is coming from o Involve family o Give positive feedback · Goals for PTSD: o Short term : Safety, decrease insomnia, identify source, grieve! o Long term : Accept the fact that the experience happened and live healthy. Substance abuse · I’m not going to go much into these notes; there wasn’t much information in the lecture that is not in the packet. · Overdose of alcohol: o Alcohol is a depressant; decreased respirations and blood pressure, vomiting may cause aspiration. · Overdose of benzodiazepines require a gastric lavage including instillation of activated charcoal. · Stimulants o Cocaine, amphetamines, and Ritalin o Increases HR and BP; decreases cardiac output and oxygen o Cocaine specifically causes MI’s Withdrawal
- 41. · Two purposes: o Safe withdrawal with medication Suppress symptoms of abstinence Around the clock schedule and PRN Never, ever go cold turkey. o Prevent relapse May need to go to AA for rest of life. Cognitive disorders Delirium · Disturbance of consciousness accompanied by change in cognition; disoriented o Alert and oriented to person only o Typically have problems recalling on memory and time. · Develops over a short period of time · Easily distracted · Difficulty concentrating · Illusions, hallucinations · Onset is rapid · Brief duration · Level of consciousness is impaired · Slurred speech · Anxious mood Causes of Delirium · Metabolic · Infection—UTI · Low sodium o Normal is 135-145 mEq/L
- 42. o Always check electrolytes! · Drug related o Or, withdrawal from drugs and alcohol o Sedatives and benzodiazepines cause confusion · Effects of anesthesia The nursing process: Assessment · Interview with simple questions and explanations · Frequent breaks · History of onset; not reliable from client o Interview family members; ask: “Is the how your mom typically acts?” · Mood/Affect o Frequently assess moods; moods change quickly · Thought process/content o Many have visual hallucinations o Very restless; hard to keep in bed. Nursing process: Goals · Free from injury o Fall precautions · Demonstrate increased orientation o Use reality orientation and validate feelings · Adequate balance of activity and rest o Help the patient keep days and nights straight · Adequate nutrition o Often forget to eat; needs nutritional supplements · Return to optimal level of functioning · A goal needs a timeline to make it measurable! Nursing process: Intervention
- 43. · Patient safety · Managing confusion o Often frightened at night. · Promote comfort and rest · Adequate fluids and nutrition o Always offer little sips of water! Nursing process: Evaluation · Successful treatment of underlying causes for delirium returns client to former level of functioning · Client and family education about avoidance of recurrence · Monitor chronic health problems · Careful use of medications · No alcohol or other non-prescribed drugs Dementia Dementia · More progressive, gradual, and permanent · Involves multiple cognitive deficits o Primarily memory impairment · Involves at least one of the following: o Asphasia (deterioration of language function) o Apraxia (impaired ability to execute motor functions) o Agnosia (inability to name or recognize objects) o Disturbance in executive functioning (ability to think abstractly and to plan, initiate, sequence, monitor, and stop complex behavior)
- 44. · May also present: o Echolalia (echoing what is heard) o Palilalia (repeating words or sounds over and over) Clinical course of Dementia · Mild: o Forgetfulness o Difficulty finding words o Frequently loses objects and experiences anxiety about these losses. o Occupational and social settings are less enjoyable, and the person may avoid them. · Moderate: o Confusion is present along with memory loss o The person cannot complete complex tasks but remains oriented to person and place. o Still recognizes familiar people. o Some assistance with care o Executive functioning suffers (especially with ADLs) · Severe: o Personality and emotional changes occur o May be delusional, wander at night, forget the names of spouse and children and require assistance in ADLs. o Most live in ECF. Causes of Dementia · Decreased metabolic activity · Genetic component · Infection · Alzheimer’s disease (#1)
- 45. · Creutzfeld-Jacob disease (CNS disorder; develops at 40- 60 years. Causes by infectious particle that is resistant to boiling) · Parkinson’s disease · Huntington’s disease (inherited gene; brain atrophy, demyelination, and enlargement of the brain ventricles. Begins in late 30’s) · Vascular Dementia (#2) o Symptoms similar to Alzheimer’s, but more abrupt, followed by rapid changes in functioning; a plateau; more abrupt changes, another plateau, and so on. o Caused by decreased blood supply to the brain. Culture · Native Americans and Eastern countries hold elders in a position of authority, respect, power, and decision making for family; this does not change despite memory loss or confusion. · May feel they are being disrespectful and reluctant to make decisions or plans for elders with dementia. Treatment for Dementia · Underlying cause o Example: Vascular dementia can be helped by diet, exercise, control of hypertension or diabetes. · Psychopharmacology o Cognex and Aricept are cholinesterase inhibitors and have shown therapeutic effects; slow the progress of dementia. They do not reverse damage already done. Must have liver function tests done with Cognex.
- 46. Flu-like symptoms, diarrhea, sleep disturbances are common. o Tegretol and Depakote help stabilize mood and diminish aggressive outbursts. These doses are often ½-2/3 less lower than prescribed for seizures, therefore, does not need to be in the “therapeutic level” for blood work. o Benzodiazepines may cause delirium and can worsen already compromised cognitive abilities. Nursing process: Assessment · History o Remember, interview family · Motor behavior and general appearance o Display aphasia o Conversation repetitive o Apraxia (such as combing hair) o Gait disturbance o Uninhibited behavior; never have displayed these behaviors before. · Mood and Affect o Grieve at first o Emotional outbursts are common o Pattern of withdrawal; lethargic, apathetic, look dazed and listless. · Thought process and content o Executive functioning impaired o Have to stop working o Client may accuse others of stealing lost objects · Sensorium and Intellectual Processes o First affects recent and immediate memory, eventually impairs the ability to recognize family members and oneself. o Confabulation : clients make up answers to fill in memory gaps; often inappropriate words or fabricated ideas (SCREW YOU, ASSHOLE).
- 47. o Visual hallucinations are common. · Judgment and insight o Underestimate risk · Self concept o Initially grieve, and then slowly lose sense of self. · Roles and Relationships · Physiologic and self-care considerations o Altered sleep-wake cycle o Some clients ignore internal cues such as hunger or thirst o Neglect bathing and grooming; become incontinent. Read the Nursing Diagnoses and Nursing Goals on your own. Too damn lazy to type out. Nursing Process: Interventions · Demonstrate caring attitude · Keep clients involved; relate to environment · Validate client’s feelings of dignity · Offer limited choices · Reframing (offering alternate points of view to explain events) · See page 487—there’s a good table there about interventions. · SAFETY! o Physical and Chemical restraint should be the last option Nursing process: Evaluation · Goals change as disease progresses · Reassessment is vital!
- 48. · Client always needs assessed, goals and interventions constantly revised · Evaluation is a continuing process. · Remember… short term goals; all goals need a time frame. Schizophrenia Types of schizophrenia · Paranoid schizophrenia o Suspiciousness o Hostility o Delusions o Auditory hallucinations o Anxiety and anger o Aloofness o Persecutory schemes o Violence · Disorganized schizophrenia o Extreme social withdrawal o Disorganized speech or behavior o Flat or inappropriate affect o Silliness unrelated to speech o Stereotyped behaviors o Grimacing mannerisms o Inability to perform activities of daily living · Catatonic schizophrenia o Significant psychomotor disturbances o Immobility o Stupor o Waxy flexibility o Excessive purposeless motor activity o Echolalia o Automatic obedience
- 49. o Stereotyped or repetitive behavior · Undifferentiated schizophrenia o Undifferentiated schizophrenia does not meet the criteria for paranoid, disorganized, or catatonic schizophrenia o Delusions and hallucinations o Disorganized speech o Disorganized or catatonic behavior o Flat affect o Social withdrawal · Residual schizophrenia o Diagnosed as schizophrenic in the past o Time limited between attacks but may last for many years o The client exhibits considerable social isolation and withdrawal and impaired role functioning Interventions · Assess the client’s physical needs · Set limits on the client’s behaviors when it interferes with others and becomes disruptive · Maintain a safe environment · Initiate one-on-one interaction and progress to small groups as tolerated o Although, reintegrating the client into the milieu as soon as possible is essential · Spend time with the client even if client is unable to respond · Monitor for altered thought processes · Maintain ego boundaries and avoid touching the client o Touching others without warning or invitation o Intruding in others’ living spaces o Talking to or caressing inanimate objects o Undressing, masturbating, or urinating in public · Limit the time of interaction with the client o Initially, the client may only tolerate 5-10 minutes of contact at one time.
- 50. · Avoid an overly-warm approach; a neutral approach is less threatening · Do not make promises to the client that cannot be kept · Establish daily routines · Assist the client to improve grooming and to accept responsibility for self-care · Sit with the client in silence if necessary · Provide short, brief and frequent contact with the client · Tell the client when you are leaving · Tell the client when you do not understand · Do not “go along” with the clients delusions or hallucinations · Provide simple concrete activities such as puzzles or word games · Reorient the client as necessary · Help the client establish what is real and unreal · Stay with the client if he is frightened · Speak to the client in a simple direct and concise manner · Reassure the client that the environment is safe · Remove the client from group situations if the client’s behavior is too bizarre, disturbing, or dangerous to others o Reassure others that the client’s inappropriate behaviors or comments are not his fault (without violating confidentiality). · Set realistic goals · Initially do not offer choices to the client, and gradually assist the client in making own decisions · Use canned or packaged food, especially with the paranoid schizophrenic client · Provide a radio or tape player at night for insomnia · Explain to the client everything that is being done · Set limits on the client behavior if the client is unable to do so · Decrease excessive stimuli in the environment · Monitor for suicide risk · Assist the client to use alternative means to express feelings through must or art therapy or writing.
- 51. Nursing interventions for the client experiencing delusions · Ask the client to describe the delusion · Be open and honest in interactions to reduce suspiciousness · Focus the conversation on reality based topics rather than the delusion · Encourage the client to express feelings and focus on the feelings that the delusions generate · If the client obsesses on the delusion, set firm limits on the amount of time for talking about the delusion · Do not dispute with the client or try to convince the client that the delusions are false · Validate if part of the delusion is real · Recognize accomplishments and provide positive feedback for successes Nursing interventions for the client experiencing hallucinations · Monitor for hallucination cues o See blue box on page 296 · Elicit description of hallucination to protect the client and others o The nurses understanding of the hallucination helps the nurse know how to calm or reassure the client · Intervene with one on one contact · Decrease stimuli or move the client to another area · Avoid conveying to the client that others are also experiencing the hallucination · Respond verbally to anything real the client talks about · Avoid touching the client · Encourage the client to express feelings
- 52. · During a hallucination, attempt to engage the client’s attention through a concrete activity o Teaching the client to talk back to the voices forcefully also may help him or her manage auditory hallucinations · Accept and do not judge or joke about the client’s behavior · Provide easy activities and a structured environment with routine activities of daily living · Monitor for signs or increasing fear, anxiety, or agitation · Provide seclusion if necessary · Administer medications as prescribed Language and communication disturbances · Clang association : Repetition of words or phrases that are similar in sound but in no other way. · Echolalia : Repetition of words or phrases heard from another person · Mutism : Absence of verbal speech · Neologism : A new word devised that has a special meaning to the client · Word salad : Form of speech in which words or phrases are connected meaninglessly · Latency of response : hesitation before the client responds to questions. This latency or hesitation may last 30-45 seconds and usually indicates the client’s difficulty with cognition or thought processes. · Thought broadcasting : believe that others can hear their thoughts · Thought withdrawa l: believe others are taking their thoughts · Thought insertion : others are placing thoughts in their mind against their will
- 53. Abnormal motor behaviors · Akathisia : Displaying motor restlessness and muscular quivering; the client is unable to sit or lie quietly · Echopraxia : Repeating the movements of another person · Waxy flexibility : having one’s arms or legs placed in a certain position and holding that same position for hours · Dyskinesia : Impairment of the power of voluntary movements Child and adolescent disorders Psychiatric disorders are not diagnosed as easily in children as they are in adults. · Children lack the abstract cognitive abilities and verbal skills to describe what is happening. Mental retardation · Mild retardations: IQ 50-70 · Moderate retardation: IQ 35-50 · Severe retardation: IQ 20-35 · Profound retardation: IQ less than 20. Adolescent depression
- 54. · Some issues are due to background and family issues · Transition into adulthood often very difficult · Depression is almost always due to a combination of factors · Boys are more successful in committing suicide; more violent in attempts o Acetaminophen affects liver o Ibuprophen affects kidneys · Presents as “classic” symptoms in girls · In boys, depression is more likely to be “acted out” with aggressive behavior such as risk taking, substance abuse, confrontations with authority. o Drinking in teenage years (ages 15-17) stops emotional growth. Kids that grow into adults are stuck in this stage (Identity vs. Role confusion). They learn that drinking is the way to cope. This is not awesome. · First major episode are during adolescent years; often between the ages of 15-19 · Manic depression o Teens may be sad and gloomy one day and excited and elevated the next o Mood stabilizers are important in decreasing mood swings Lithium (check blood levels!) Depakote Tegretol Neurontin · In depression, one of the first cues is a large drop in school performance · Other symptoms disguised: o Drug/alcohol abuse o Lack of concentration o Restlessness or hyperactivity o Anti-social behavior (conduct disorder) · Extreme fatigue, sleep all the time but are not rested · Suicide warning signs… o Constant insomnia; may be on computer at all hours of the night
- 55. o Changes in behavior o Dropping grades—again, school is a huge issue · Interventions for suicide o High risk teens make their decisions after a “disaster” has occurred: break-ups, academic failure, fight with parents, or run-in with authority o Alcohol is involved in ½ of all suicides; seriously impairs judgement · Suicide is not chosen; it happens when pain exceeds resources for pain · Talk to your kids! o The best place is in the car when they’re trapped, haha. Start with the basics; “How are you doing?” Then, praise Then get down and dirty to the real subject Childhood Schizophrenia · Group of disorders of thought processes characterized by gradual disintegration of mental function · Occurs in adolescents or as young adults · Suicide is the #1 cause of death in young people with schizophrenia · Treatment and prognosis o Lifetime of therapy and family support o Medications o Struggle for family to stay involved Often rejected or just can’t take anymore disruption in their lives. Obsessive-Compulsion disorder · Symptoms often begin slowly and gradually during their childhood or teenage years and increase in severity as time goes on.
- 56. · Though a chronic disease, there will be periods of reduced symptoms followed by “flare-ups”, often stressful times in person’s life. · Relief is only temporary; usually both obsessions and compulsions occur together · Recognize thoughts or behaviors are irrational; but are compelled to continue them “against their will”. · Treatment: o Exposure and response prevention o SSRIs help reduce symptoms of OCD—monitor for side effects · Compulsions o Washing, cleaning, constant checking, mental counting rituals o Touching, ordering, rearranging o Asking for reassurance or confessing o Masturbation—especially seen in children who haven’t yet discovered this is socially unacceptable behavior Autistic disorder · Most prevalent in boys; identified no later than 3-years of age · Child has little eye contact, few facial expression, doesn’t use gestures to communicate · Does not relate to parents or peers, lacks spontaneous enjoyment, apparent absence of mood and emotional affect, can not be engaged in play or make believe · Repetitive motor behaviors such as hand-flapping, body twisting, or head banging · May improve as child acquires language skills · Short term impatient therapy is used when behaviors such as head banging or tantrums are out of control o Haldol or Risperadol may be effective (prn, of course) · Goals of treatment: o Reduce behavioral symptoms
- 57. o Promotes learning and development o Language skills development Attention deficit disorder · Characterized by patterns of inattention, hyperactivity, and impulsiveness · Account for most mental health referrals · Needs to be physically seen for a renewal of ADHD drugs monthly · Often diagnosed when a child starts school · Distinguishing bipolar disorder from ADHD can be difficult but is crucial because treatment is so different for each disorder · Signs and symptoms o Inattentive behaviors o Hyperactive/impulsive behaviors Fidgets Often leaves seat Can’t play quietly Interrupts Cannot wait turn · Treatment o The most effective treatment combines pharmacotherapy with behavioral, psychosocial, and educational interventions · Psychopharmacology o Methylphenidate (Ritalin) o Amphetamine compound (Adderall) The most common side effects of these drugs are insomnia, loss of appetite, and weight loss or failure to gain weight. Giving stimulants during daytime hours usually combats insomnia. Give the child breakfast and snacks to gain weight o Atomoxetine (Strattera)
- 58. Non-stimulant drug; is an antidepressant— selective norepinephrine reuptake inhibitor. Most common side effects were decreased appetite, N/V, tiredness, and upset stomach. Can cause liver damage, must have liver function tests periodically. · Strategies for Home and School o Behavioral strategies are necessary to help the child master appropriate behaviors. o Effective approaches: Provide consistent rewards Consequences for behavior Offer consistent praise Use time out Give verbal reprimands Use daily report cards for behavior Point system for positive and negative behavior Therapeutic play; use play to understand thoughts and feelings and helps with communication. Educate parents! · Cultural considerations o Parents from different cultures have a different threshold for tolerating specific types of behavior. · General appearance and Motor behavior o Speech is unimpaired, but the child cannot carry on a conversation; he interrupts, blurts out answers before the question is finished, and fails to pay attention to what is said. · Mood and affect o Mood may be labile, even to the point of verbal outbursts or temper tantrums. o Anxiety, frustration, and agitation are common · Judgment and insight o May fail to perceive harm or danger and engage in impulsive acts such as running into the street and jumping off of high objects. · Physiologic and Self-care considerations
- 59. o Children with ADHD may be thin if they do not take time to eat properly or cannot sit through meals. o May be a history of physical injuries due to risk-taking behaviors · Nursing diagnoses o Risk for injury Child will remain free from injury If the child is engaged in a potentially dangerous activity, the first step is to stop the behavior. This may require physical intervention if the child is running into a street or jumping off of a high place. Attempting to talk or reason to a child engaged in a dangerous activity is unlikely to succeed because of their inability to pay attention and to listen. When the incidence is over and the child is safe, talk to the child about the behavior. o Ineffective role performance Will not violate others boundaries Give positive feedback for meeting expectations. State acceptable behavior clearly o Impaired social interactions Demonstrate age-appropriate social skills Supervise the child closely while he is playing. It is often necessary to act first to stop the harmful behavior by separating the child from the friend o Improved role performance Simplify instructions and directions—give one step of a process at a time Give the child positive feedback and sense of accomplishment Manage the environment
- 60. Minimal noise and distraction Face the teacher in the front row and away from window or door o Ineffective family coping Will complete tasks Face the child on his level and use good eye contact Give the child frequent breaks Routines are important; child with ADHD do not adjust to changes readily o Parental support Listen to parent’s feelings Because these children often are not diagnosed until the 2nd or 3rd grade, they may have missed much basic learning for reading and math. Parents should know that it takes time for them to catch up to other children the same age. o Evaluation Medications are often in decreasing hyperactivity and impulsivity relatively quickly. Improved sociability, peer relations, and academic achievement happen more slowly. Conduct disorder · Characterized by persistent antisocial behavior in children and adolescents that significantly impair their ability to function in social, academic, or occupational area. o Symptoms are clustered into 4 areas Aggression to people and animals Destruction to property Deceitfulness and theft Serious violation of rules and the law o More symptoms Decreased self-esteem
- 61. Poor frustration tolerance Tempter often out of control Early onset of sexual behavior, alcohol and substance abuse, smoking, risky behavior Anti-social See more in the red box on page 457 · Types of conduct disorder o Classified by age of onset Adolescent-onset type is defined by no behaviors of conduct disorder until after 10 years of age. Least likely to be aggressive Have more normal peer relationships Less likely to have persistent conduct disorder or antisocial personality disorder as adults Childhood-onset type involves symptoms before 10 years of age Physically aggressive Disturbed peer relationships More likely to have persistent conduct disorder and to develop antisocial personality disorder as adults o Can be classified as: Mild : few conduct problems causing minor harm to others Lying, truancy, staying out late without permission Moderate : Number of conduct problems increase as does the amount of harm to others. Vandalism and theft Severe : Many conduct problems that cause considerable harm to others. Forced sex, cruelty to animals, weapons, burglary, robbery. · Treatment of conduct disorder o MUST BE GEARED TOWARD DEVELOPMENTAL AGE o School aged:
- 62. Child, family, and school environment are the focus of treatment Family therapy is essential o Adolescents Rely less on their parents, so treatment is based on individual therapy. Conflict resolution, anger management, social skills Try to keep the adolescent in his environment (home) o Medications have little effect Antipsychotics for clients who present a clear danger to others Mood stabilizers for clients with labile moods · Cultural considerations o Be careful of diagnosis of Conduct disorder, must know history and circumstances of each child. High areas of crime rates Could be a matter of survival · Nursing process o Risk for Other-directed violence The client will not hurt others or damage property SET LIMITS Inform the client of the rule or limit Explain the consequences if broken State expected behavior Behavioral contract Time out; not a punishment—a place to regain self control Give client a schedule of daily activities o Noncompliance The client will participate in treatment More likely to participate in treatment and daily routines if they have input concerning the schedule o Ineffective coping The client will learn effective problem-solving and coping skills
- 63. Help identify the problem and to solve problems effectively. o Impaired social interaction The client will use age-appropriate and acceptable behaviors when interacting with others. Teach social skills Discuss the news, sports, or other topics as the client may not know how to have a normal conversation. o Chronic low self-esteem The client will verbalize positive, age-appropriate statements about self Oppositional Defiant disorder · Consists of an enduring pattern of uncooperative, defiant, and hostile behavior toward authority figures without major antisocial violations. · A certain level of oppositional behavior is common in children in adolescence. · Oppositional defiant disorder is diagnosed only when behaviors are more frequent and intense than unaffected peers and cause dysfunction in social, academic, or work situations. TIC disorders · Sudden, rapid, recurrent, non-rhythmic motor movement or vocalization · Stress and fatigue exacerbates tics · Treatment: Risperadol and Zyprexia · Complex vocal tics o Coprolalia : Use of socially unacceptable words, often obscene o Palilalia : Repeating own sounds or words
- 64. o Echolalia : Repeating the last heard sound, word, or phrase Tourette’s syndrome · Multiple motor tics and one or more vocal tics · May occur many times a day for over a year · Usually identified by 7 years of age Elimination disorders · Encopresis : repeated passage of feces into inappropriate places such as clothing or floor by a child who is at least 4 years of age either chronically or developmentally. Often involuntary, but can be intentional (oppositional defiant disorder or conduct disorder). Associated with constipation that occurs for psychological, not medical reasons. · Enuresis : Repeated voiding of urine during the day or night into clothing or bed by a child at least 5 years of age. · Treated with imipramine (Tofranil), an antidepressant with a side effect of urinary retention. o Was once treated with vasopressin which decreases circulatory volume. Eating disorders The distinguishing factor of anorexia includes an earlier age of onset and below-normal body weight; the person fails to recognize the eating behavior as a problem. Clients with
- 65. bulimia have a latter age at onset and a near-normal body weight. They usually are ashamed and embarrassed by the eating disorder. Eating disorders appear to be equally common among Hispanic and white women and less common among African American and Asian women. Anorexia Nervosa · A life-threatening eating disorder characterized by the client’s refusal or inability to maintain a minimally normal body weight, intense fear of gaining weight or becoming fat, significantly disturbed perception of the shape or size of the body, and steadfast inability or refusal to acknowledge the seriousness of the problem or even that one exists. · Has experienced amenorrhea for at least 3 consecutive cycles · Complaints of constipations and abdominal pain · Cold intolerance · Hypotension, hypothermia, bradycardia o Intravascular volume is decreased; less blood to pump through heart, also due to excessive exercise · Elevated BUN o Normal levels: 10-20 mg/dl o Urea is formed in the liver and is the end product of protein metabolism. o In anorexia, the body has already used fat for energy; it is now breaking down muscles for energy—the reason for the elevated BUN · Decreased albumin o Normal levels: 3.5-5 g/dl o Measures amount of protein in the body; albumin is a protein formed in the liver.
- 66. o Albumin tests are a great indicator of nutritional status · Leukopenia and mild anemia o Not enough food and nutrients to replenish cells · Has a preoccupation with food and food-related activities · Can be divided into 2 subgroups: o Restricting subtype : lose weight primarily through dieting, fasting, or excessively exercising. o Binge eating and purging subtype : engage regularly in binge eating followed by purging. · Engage in unusual or ritualistic food behaviors o Refusing to eat around others o Cutting food into minute pieces o Not allowing the food they eat to touch their lips · Excessive exercise is common · Diagnosed between 14 and 18 years of age · Pleased with their ability to control their weight and may express this. · As the illness progresses, depression and lability in mood become more apparent · Isolate themselves · Believe peers are jealous of their weight loss and believe family and health care professionals are trying to make them “fat and ugly”. · Clients who use laxatives are at a greater risk for medical complications. · Autonomy may be difficult in families that are overprotective or in with enmeshment (lack of clear boundaries) exists. By losing weight, these clients have some control in their lives. · Have body image disturbance (page 409) · Can be very difficult to treat because they are often resistant, appear uninterested, and deny their problems. · Treatment: o Focusing on weight restoration o Nutritional rehabilitation o Rehydration
- 67. o Correction of electrolyte imbalances o Severely malnourished individuals may require TPN, tube feedings, or hyperalimentation to receive adequate nutritional intake. o Access to the bathroom is supervised to prevent purging as clients begin to eat more food. o Weight gain and adequate food intake are most often the criteria for determining the effectiveness of treatment. o Amitriptyline (Elavil) and the antihistamine cyproheptadine (Periactin) in high doses (up to 28mg/d) can promote weight gain in inpatients. o Olanzapine (Zyprexa) has been used with success because of both its antipsychotic effect (on bizarre body image distortions) and associated weight gain. o Fluoxetine (Prozac) has shown some effectiveness in preventing relapse in clients whose weight has been partially or completely restored; close monitoring is needed because weight loss can be a side effect. · Family members often describe clients with anorexia as perfectionists with above average intelligence, dependable, eager to please, and seeking approval before their condition began. · Clients with anorexia appear slow, lethargic, and fatigued; they may appear emaciated, depending on the amount of weight loss. May be slow to respond and have difficulty deciding what to say. · Reluctant to answer questions fully because they do not want to acknowledge any problem. · Often wear loose clothing in layers · Seldom smile, laugh, or enjoy any attempts at humor Bulimia Nervosa · Characterized by recurrent episodes (at least twice a week for 3 months) of binge eating followed by
- 68. inappropriate measures to avoid weight gain such as purging (vomiting, laxatives, diuretics, enemas, or emetics), fasting, or excessively exercising. · Engaging in binge eating secretly · Binging or purging episodes are often precipitated by strong emotions and followed by guilt, remorse, shame, or self-contempt. · Recurrent vomiting destroys tooth enamel, has dental caries and ragged or chipped teeth. Dentists are often the first health care professionals to recognize this. · Bulimia is typically diagnosed at 18 or 19. · Clients with bulimia are aware that their eating behavior is pathologic and go great lengths to hide it from others. · Clients with a co-morbid personality disorder tend to have poorer outcomes than those without. · Most are treated on an outpatient basis · Antidepressants are more effective than the placebos in reducing binge eating · Clients are often focused on pleasing others and have a history of impulsive behavior such as substance abuse and shoplifting as well as anxiety, depression, and personality disorders. · May be underweight, overweight, but are generally close to expected body weight for age and size · Appear open and willing to talk; initially pleasant and cheerful as though nothing is wrong Nursing outcomes/interventions Imbalanced Nutrition: Less than/More than body requirements · The client will establish adequate nutritional eating patterns
- 69. o Implement and supervise the regimen for nutritional rehabilitation o A diet of 1200-1500 calories is ordered, with gradual increases in calories until clients are ingesting adequate amounts for height, activity level, and growth needs. Start slowly—will have massive diarrhea o The client with anorexia may be critically malnourished. TPN through central line Electrolyte balance Tube feeds o A liquid protein supplement is given to replace any food not eaten to ensure consumption to ensure total number of calories prescribed o Must monitor meals and snacks and will sit at the table during eating away from the other clients A major goal is to first get them to the table o Diet beverages and food substitutions may be prohibited o Specified time may be set for consuming each meal and snack o Discourage clients from performing food rituals such as cutting food into tiny pieces or mixing foods in unusual combinations o Be alert for any attempts by client to hide or discard food o Must remain in view of staff for 1-2 hours to ensure they do not vomit; access to bathrooms is supervised. o Client is weighed daily on awakening and after they have emptied their bladder. Have the client wear a hospital gown each time they are weighed; they may attempt to place objects in their clothing to give the appearance of weight gain. o In bulimia, the clients should sit at a table in a kitchen or dining room. o Write out a grocery list, it is easier to follow a nutritious eating plan
- 70. Ineffective coping · The client will eliminate use of compensatory behaviors such as excessive exercise and use of laxatives and diuretics · The client will demonstrate coping mechanisms not related to food · The client will verbalize feelings of guilt, anger, anxiety, or an excessive need for control o Help the client recognize emotions such as anxiety or guilt by asking them to describe what they are feeling; allow adequate time for response. Do not ask “are you anxious? Sad?” because the client may quickly agree rather than struggle for an answer o Encourage self-monitoring (page 414); a behavior-cognitive approach Disturbed body image · The client will verbalize acceptance of body image with stable body weight o Help clients identify areas of personal strength that are not food-related broadens clients’ perceptions of themselves. Somatoform disorders Somatization: The transference of mental experiences and states into bodily symptoms.
- 71. Somatoform disorders: Characterized as the presence of physical symptoms that suggest a medical condition without demonstrable organic basis to account fully for them. The three central features of somatoform disorders are as follows: · Physical complaints suggest major medical illness but have no demonstrable organic basis. · Psychological factors and conflicts seem important in initiating, exacerbating, and maintaining the symptoms. · Symptoms or magnified health concerns are not under the client’s conscious control. The five specific somatoform disorders are as followed: · Somatization disorder : Characterized by multiple physical symptoms. It begins by 30 years of age, extends over several years, and includes a combination of pain and GI, sexual, and pseudoneurologic symptoms. o Client’s jump from one physician to the next, or may see several providers at once in an effort to obtain relief of symptoms. o They tend to be pessimistic about the medical establishment and often believe their disease could be diagnosed of the providers were more competent. · Conversion disorder : Involves unexplained, usually sudden deficits in sensory or motor function (blindness, paralysis). These deficits suggest a neurological disorder but are associated with psychological factors. An attitude of la belle indifference, a seemingly lack of concern or distress, is the key feature. · Pain disorder : Pain is the primary physical symptom which is generally unrelieved by analgesics and greatly
- 72. affected by psychological factors in terms of onset, severity, exacerbation, and maintenance. · Hypochondriasis : Preoccupation with the fear that one has a serious disease (disease conviction) or will get a serious disease (disease phobia). It is thought that clients with this disorder misinterpret bodily sensations or functions. · Body dysmorphic disorder : Preoccupation with an imagined or exaggerated defect in personal appearance such as thinking one’s nose is too large or teeth are crooked and unattractive. Symptoms of a somatization disorder · Pain symptoms : complaints of headache, pain in the abdomen, head, joints, back, chest, rectum; pain during urination, menstruation, or sexual intercourse. · GI symptoms : nausea, bloating, vomiting (other than pregnancy), diarrhea, or intolerance of several foods. · Sexual symptoms : Sexual indifference (don’t care to do the dirty), erectile or ejaculatory dysfunction, irregular menses, excessive menstrual bleeding. · Pseudoneurologic symptoms : Impaired coordination or balance, paralysis or localized weakness, difficulty swallowing or lump in throat, aphonia (loss of speech sounds), urinary retention, swollen tongue, hallucinations, double vision, blindness, deafness, seizures; disassociative symptoms such as amnesia; or loss of consciousness other than fainting. Related disorders: · Malingering : The intentional production of false or grossly exaggerated physical or psychological symptoms; it is motivated by external incentives such as avoiding work, evading criminal prosecution,
- 73. obtaining financial compensation, or obtaining drugs. Their purpose is some external incentive or outcome that they view as important and results directly from their illness. People who malinger can stop the physical symptoms as soon as they have gained what they wanted. · Factitious disorder : This is also known as Munchausen syndrome. Occurs when a person intentionally produces or feigns physical or psychological symptoms solely to gain attention. o Munchausen syndrome by proxy occurs when a person inflicts illness or injury to someone else to gain the attention of emergency medical personnel or to be a “hero” for saving the victim. This occurs most often in people who are in or familiar with medical professions, such as nurses, physicians, medical technicians, or hospital volunteers. · Primary gain : Direct external benefits that being sick provides, such as relief of anxiety, conflict, or distress. · Secondary gains : Internal or personal benefits received from others because one is sick, such as attention from family members and comfort measures (being brought tea, receiving a back rub). Treatment: · Treatment focuses on managing symptoms and improving quality of life. · A trusting relationship helps to ensure that client’s stay with and receive care from one provider instead of “doctor shopping.” · SSRIs are commonly used for depression that may accompany somatoform disorders. Assessment
- 74. · The nurse must investigate physical health status thoroughly to ensure there is no underlying pathology requiring treatment. It is important not to dismiss all future complaints because at any time the client could develop a physical condition that would require medical attention. · In many cases, the client’s appearance brightens and they look much better as the assessment interview begins because they have the nurse’s undivided attention. · Client’s often have sleep pattern disturbances, lack basic nutrition, and get no exercise. Nursing diagnoses · Ineffective coping o The client will identify the relationship between stress and physical symptoms. Emotion-focused coping strategies help the clients relax and reduce feelings of stress. This includes progressive relaxation, deep breathing, guided imagery, and distractions such as music. Problem-focused coping strategies help to resolve or change a client’s behavior or situation or to manage life stressors. This includes learning problem solving methods. The nurse should help the client role play the above situations. · Ineffective denial o The client will verbally express emotional feelings The nurse should not attempt to confront clients about somatic symptoms or attempt to tell them that these symptoms are not “real.” Encourage the client to write in a daily journal
- 75. Limiting the time that clients can focus on physical complaints alone may be necessary. The nurse may have to explain to the family about primary and secondary gains; this will encourage relatives to stop reinforcing the “sick role.” · Impaired social interactions o The client will follow an established daily routine The nurse must help the client to establish this that includes improved health behaviors. The challenge for the nurse is to validate the client’s feelings while encouraging him to participate in activities. The nurse should help the client plan social contact with others, what to talk about (other than the client’s complaints), and can improve the client’s confidence in making relationships. · Anxiety o The client will demonstrate alternative ways to deal with stress, anxiety, and other feelings · Disturbed sleep pattern o The client will demonstrate healthier behaviors regarding rest, activity, and nutritional intake. The nurse explains that inactivity and poor eating habits perpetuate discomfort and that often it is necessary to engage in behaviors even though one doesn’t feel like it. · Fatigue · Pain