Va pcmh study 6 2014[1]
- 1. Copyright 2014 American Medical Association. All rights reserved. Implementation of the Patient-Centered Medical Home in the Veterans Health Administration Associations With Patient Satisfaction, Quality of Care, Staff Burnout, and Hospital and Emergency Department Use Karin M. Nelson, MD, MSHS; Christian Helfrich, MPH, PhD; Haili Sun, PhD; Paul L. Hebert, PhD; Chuan-Fen Liu, MPH, PhD; Emily Dolan, PhD; Leslie Taylor, PhD; Edwin Wong, PhD; Charles Maynard, PhD; Susan E. Hernandez, MPA; William Sanders, AA, AS; Ian Randall, MHSA; Idamay Curtis, BA; Gordon Schectman, MD; Richard Stark, MD; Stephan D. Fihn, MD, MPH IMPORTANCE In 2010, the Veterans Health Administration (VHA) began implementing the patient-centered medical home (PCMH) model. The Patient Aligned Care Team (PACT) initiative aims to improve health outcomes through team-based care, improved access, and care management. To track progress and evaluate outcomes at all VHA primary care clinics, we developed and validated a method to assess PCMH implementation. OBJECTIVES To create an index that measures the extent of PCMH implementation, describe variation in implementation, and examine the association between the implementation index and key outcomes. DESIGN, SETTING, AND PARTICIPANTS We conducted an observational study using data on more than 5.6 million veterans who received care at 913 VHA hospital-based and community-based primary care clinics and 5404 primary care staff from (1) VHA clinical and administrative databases, (2) a national patient survey administered to a weighted random sample of veterans who received outpatient care from June 1 to December 31, 2012, and (3) a survey of all VHA primary care staff in June 2012. Composite scores were constructed for 8 core domains of PACT: access, continuity, care coordination, comprehensiveness, self-management support, patient-centered care and communication, shared decision making, and team-based care. MAIN OUTCOMES AND MEASURES Patient satisfaction, rates of hospitalization and emergency department use, quality of care, and staff burnout. RESULTS Fifty-three items were included in the PACT Implementation Progress Index (Pi2 ). Compared with the 87 clinics in the lowest decile of the Pi2 , the 77 sites in the top decile exhibited significantly higher patient satisfaction (9.33 vs 7.53; P < .001), higher performance on 41 of 48 measures of clinical quality, lower staff burnout (Maslach Burnout Inventory emotional exhaustion subscale, 2.29 vs 2.80; P = .02), lower hospitalization rates for ambulatory care–sensitive conditions (4.42 vs 3.68 quarterly admissions for veterans 65 years or older per 1000 patients; P < .001), and lower emergency department use (188 vs 245 visits per 1000 patients; P < .001). CONCLUSIONS AND RELEVANCE The extent of PCMH implementation, as measured by the Pi2 , was highly associated with important outcomes for both patients and providers. This measure will be used to track the effectiveness of implementing PACT over time and to elucidate the correlates of desired health outcomes. JAMA Intern Med. doi:10.1001/jamainternmed.2014.2488 Published online June 23, 2014. Invited Commentary Supplemental content at jamainternalmedicine.com Author Affiliations: Author affiliations are listed at the end of this article. Corresponding Author: Karin M. Nelson, MD, MSHS, Seattle Center of Innovation for Veteran-Centered and Value-Driven Care, VA Puget Sound Health Care System, 1100 Olive Way, Ste 1400, Seattle, WA 98108 (karin .nelson@va.gov). Research Original Investigation E1 Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 2. Copyright 2014 American Medical Association. All rights reserved. A lthoughthepatient-centeredmedicalhome(PCMH)has been endorsed by most major primary care groups as a promising model to strengthen primary care, de- crease costs, and improve quality,1 early assessment of PCMH impact have yielded mixed results.2-10 Since 2010, the Veter- ans Health Administration (VHA) has undertaken national adoption of a PCMH model, called PACT (Patient Aligned Care Team).11 The focus of PACT has been to restructure primary care to provide team-based care that is more comprehensive, coordinated, and patient centered.11 The PACT initiative is a multifaceted and complex inter- vention, creating challenges to measuring implementation across diverse clinic sites. One of the most widely recognized PCMH recognition tools is the National Committee for Quality Assurance(NCQA)certificationprocess,whichfocusesonprac- ticeinfrastructureandhealthinformationtechnology,12 anarea in which the VHA has made considerable past investments.13,14 The VHA has a universally deployed electronic health record, electronic prescribing, patient registries, and a national qual- ity improvement and performance measurement infrastruc- tureforwhichallclinicsintheVHAwouldreceive“credit.”Many national programs for coordinating care, such as home-based primary care, integrated mental health services, and pallia- tive care, were already widely available before PACT was ini- tiated. The focus within the VHA has been on how effectively these extensive resources are being applied and coordinated to fulfill the goals of the PACT initiative.11 Our goal was to derive a comprehensive index from exist- ing data and survey instruments that would have a low re- spondent burden and would reflect processes and attributes that are essential to effective primary care. Our approach dif- fers from other PCMH measurement tools15 by incorporating multiple data sources, including a primary care personnel sur- vey, patient surveys, and administrative data. We sought to develop a measure to represent areas of focus of the PACT ini- tiative, including continuity through team-based care, patient access, care coordination, and patient-centered care.11 We desired an instrument that would facilitate comparisons across clinical sites within the VHA, assist in identifying sites that had most effectively implemented PACT, and determine the relationship between effective implementation and important outcomes, such as patient satisfaction, quality of care, provider experience, and use of health care services. Methods Survey Instruments and Data Sources Patient Survey We used data from the previously validated Consumer Assessment of Health Plans–Patient Centered Medical Home (CAHPS PCMH) survey16 that was administered to a nationally weighted random sample of veterans who received outpatient care from June 1 to December 31, 2012. The CAHPS PCMH scales have acceptable internal consistency reliability esti- mates for access (Cronbach α, 0.74), comprehensiveness (0.68), self-management support (0.62), patient-centered care and communication (0.91), and shared decision making (0.61).16 To test convergent validity, we used information on patient satisfaction from another sample of veterans from the Survey of the Health Experiences of Patients, an ongoing national mailed US Department of Veterans Affairs (VA) sur- vey that assesses the health care experiences of veterans who receive care at the VHA and uses a stratified random sampling method.17 The evaluation efforts are part of an going quality improvement effort at the VHA and are not considered research activity; they are thus not subject to institutional review board review or waiver. Primary Care Personnel Survey The PACT Primary Care Personnel Survey was an internally developed instrument designed to measure team functioning in PACT and has been described elsewhere.18 The target popu- lation of the survey was all VHA primary care personnel, including the 4 occupations included in PACT teams: primary care providers, nurse care managers, medical associates (eg, licensed practical nurses and medical technicians), and administrative clerks. Data were collected from May 21 through June 29, 2012. Team-based care was represented by items from the primary care personnel survey related to del- egation, staffing, team functioning, and team assignment.18 Administrative Data Information about demographics, clinical characteristics, and use of health services was obtained from the VHA Corporate Data Warehouse for fiscal year 2012 (n = 5 653 616). Using data from the Primary Care Management Module contained within the Corporate Data Warehouse, we identified all patients who were enrolled in primary care and assigned to a primary care provider.19 WeincludedadministrativedataforimportantPACT programmatic goals,11 including (1) access to care and use of non–face-to-face care, such as telephone clinics and secure messaging; (2) continuity of care; and (3) use of VHA pro- grams to support care coordination (eg, home telemonitor- ing, 2-day posthospital follow-up). We used data collected by the VHA External Peer Review Program(EPRP)duringfiscalyear2012toassessqualityofcare. The EPRP is an audit program designed to assess clinical per- formance using standard performance criteria. National data are collected through manual abstraction of electronic health recordsbyanindependentexternalcontractor.20 Previousstud- ies have found high interrater reliability (κ = 0.9) within the EPRP program.14 Construction of the PACT Implementation Progress Index The method for developing the PACT Implementation Prog- ress Index (Pi2 ) and a full description of all items are provided in eTable 1 in the Supplement. Briefly, we mapped data items to PACT conceptual domains, calculated domain scores based on these items, and then generated site-level rankings for each domain. Table 1 outlines Pi2 domains and provides examples of representative variable items. A Pi2 score was assigned to each clinic based on the number of domains in the top and bot- tom quartiles for the domain scores, ranging from 8 (all do- main scores in the top quartile) to –8 (all domain scores in the bottom quartile). Using these scores, we categorized sites in Research Original Investigation Patient-Centered Medical Home Implementation E2 JAMA Internal Medicine Published online June 23, 2014 jamainternalmedicine.com Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 3. Copyright 2014 American Medical Association. All rights reserved. the top decile of the Pi2 (score, 5 to 8) as having achieved ef- fective implementation and those in the lowest decile of the Pi2 (score, –7 to –5) as having been less effective. Patient- and Provider-Level Outcome Measures Patient satisfaction was assessed by using a single item from the CAHPS PCMH survey16 as follows: “Using any number from 0 to 10, where 0 is the worst provider possible and 10 is the best provider possible, what number would you use to rate this provider?” Staff burnout was assessed with both a single-item mea- sure and the emotional exhaustion subscale of the Maslach Burnout Inventory, a widely used measure of burnout.21-23 The single item measure asks: “Overall, based on your defini- tion of burnout, how would you rate your level of burnout,” with 5 ordinal response options.24 We defined burnout as a response of 3 or higher, where 3 corresponds to “I am defi- nitely burning out and have one or more symptoms of burn- out, such as physical and emotional exhaustion.”24 We also used a 3-item version of the Maslach Burnout Inventory subscale.25 Items reflecting burnout symptoms are scored using a Likert scale ranging from 0 (never) to 6 (every day) and summed to form a scale score. We defined burnout as a score of 10 or higher (range, 0-18). To assess quality of care, we examined outpatient mea- surementsfromtheEPRPforchronicdiseasemanagement,be- havioral health screening, and prevention services. These in- dicators include frequently used measures of the quality of prevention (eg, vaccinations, screening tests) and outpatient care of chronic diseases (eg, annual retinal examinations in pa- tients with diabetes mellitus). The performance measure- ment for preventive services and chronic disease cohorts, sam- pling frame, and criterion for meeting the measurement are provided in eTable 2 in the Supplement. The EPRP selects a random sample of patient records from VHA facilities to monitor quality and appropriateness of medical care.26 The sample includes veterans who used VHA health care at least once in the 2 years before the assessment. Patients who were sampled had at least 1 primary care or specialty medical visit in the month being sampled. Among eligible patients, a random sample is drawn with over- sampling of prevalent chronic conditions (eg, diabetes, heart failure).26 For patients at each primary care site, we determined the numbers of emergency department or urgent care visits, VA hospital admissions, and hospitalizations for ambulatory care– sensitive conditions (ACSCs), which are postulated to be most avoidable through provision of effective primary care.27 Hos- pitalizations for ACSCs were based on Agency for Healthcare Research and Quality Prevention Quality Indicators and were identified through standardized protocols using Interna- tional Classification of Diseases, Ninth Revision, diagnoses and Current Procedural Terminology codes from inpatient VA records.27 Table 1. PCMH Concepts and Pi2 Domains PACT Initiative Goals Pi2 Domains Total Items, No. Items From Each Data Source, No. Example Itemd CAHPS PCMHa CDWb Personnel Surveyc Accessible, continuous, and coordinated care Access 11 6 5 0 How often did you get an appointment as soon as you needed?a When you phoned this provider’s office, how often did you get an answer to your medical question that same day?a Same-day access to appointments (% of clinics)b Enhanced access: telephone clinics (%)b Continuity of care 3 1 2 0 How long have you been going to this provider?a Proportion of visits to assigned primary care providerb Care coordination 7 5 2 0 When this provider ordered a test, how often did someone from this provider’s office follow up to give you those results?a Did the provider seem informed and up to date about the care you got from specialists?a Percentage of patients contacted 2 d after hospital dischargeb Patient-centered care Comprehensiveness 3 3 0 Did you and anyone in this provider’s office talk about things in your life that worry you or cause you stress?a Self-management support 2 2 0 Did anyone in this provider’s office talk with you about specific goals for your health?a Patient-centered care and communication 6 6 0 How often did this provider explain things in a way that was easy to understand?a Shared decision making 3 3 0 When you talked about starting a prescription medicine, did this provider ask you what you thought was best for you?a Team-based care Delegation, staffing, and team functioning 18 0 0 18 Primary care provider relies on registered nurse care manager for tasks including gathering patient preventive services, responding to prescription refillsc Percentage reporting recommended staffing ratioc Time spent in team huddles: percentage spending >30 min/dc Total … 53 26 9 18 … Abbreviations: CAHPS PCMH, Consumer Assessment of Health Plans–Patient Centered Medical Home; CDW, Corporate Data Warehouse; PACT, Patient Aligned Care Team; PCMH, patient-centered medical home; Pi2 , PACT Implementation Progress Index. a CAHPS PCMH patient survey. b CDW data from US Department of Veterans Affairs. c PACT Primary Care Personnel Survey. d Full description in eTable 1 in the Supplement. The questions have been shortened for the sake of brevity. Patient-Centered Medical Home Implementation Original Investigation Research jamainternalmedicine.com JAMA Internal Medicine Published online June 23, 2014 E3 Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 4. Copyright 2014 American Medical Association. All rights reserved. Statistical Analysis PI2 Properties To test internal consistency reliability, we calculated the Cron- bach α for all items in each domain and all 53 items that make up the total scale. Variation in PCMH Adoption We evaluated bivariate comparisons of facility characteristics and level of implementation by using χ2 tests for categorical variables and t tests for continuous variables. We compared sites assessed to have effectively implemented PACT with those assessed as less effective according to type of facility (hospital or community-based outpatient clinic), number of patients, demographic characteristics, and Elixhauser comor- bidity score.28 Associations With Patient and Provider Outcomes We used a nonparametric test of trend for the ranks across or- dered groups (an extension of the Wilcoxon rank sum test) to test for trends in patient satisfaction and staff burnout by Pi2 scores. We tested differences in the proportions of eligible pa- tients at each VHA clinic fulfilling each of the 48 quality indi- cators according to the success of PACT implementation as measured by the Pi2 . We calculated rates of services at the fa- cility level by dividing the number of patients who satisfied the EPRP quality measure by the number who met inclusion criteria for each quality measure (eTable 3 in the Supple- ment). For each of the 48 facility-level quality indicators, we tested the trend in proportions of patients fulfilling the EPRP qualityguidelinebythelevelofPACTimplementation.Weused the nonparametric test for trend developed by Cuzick, which is an extension of the Wilcoxon test.29 We adjusted for mul- tiple comparisons using a method described by Benjamini and Yekutieli.30 To determine whether more effective implemen- tation (as measured by Pi2 ) corresponded to higher perfor- mance overall, we included all 48 outcome measures in a lin- ear mixed-effects model that accounted for correlation among outcomes from the same facility and estimated an overall implementation effect. We adjusted for implementation in this model as a linear term ranging from 1 to 5, corresponding to the grouped Pi2 scores. This approach was possible because all 48 outcomes were measured on the same scale. We examined fiscal year 2012 emergency department and urgent care visits and total hospitalizations for sites with more effective vs less effective implementation, adjusting for pa- tient age, community-based outreach clinics, and Elixhauser comorbidityscores.28 Toaccountfortemporaltrends,wemod- eled facility-level trends for hospitalization from 2003 to 2012. The method for examining such trends has been described elsewhere.31 We estimated interrupted time-series models of ACSC and all-cause hospitalizations from October 1, 2003, through September 20, 2012, for each facility and assessed how the trends in hospitalizations changed after the start of the PACT initiative in April 2010. All regression models adjusted for facility-level patient characteristics, unemployment rate in the VA market area, quarterly dummy variables to capture sea- sonal variation, and a linear time trend. Patient risk was mea- sured using mean facility-level Elixhauser comorbidity scores. Changes in admissions for ACSC and all-cause hospitaliza- tions after implementation of the PACT initiative were calcu- lated as the difference between the observed rate of admis- sions and the predicted rate had the initiative not been implemented during the 2½-year period between April 1, 2010, and September 30, 2012. In this way, we estimated changes in admissions that might be attributed to the PACT initiative. Trend analyses for hospitalizations were stratified by age (≥65 and <65 years) to account for the substantial use of non-VA health care by Medicare-eligible veterans.32 We then com- pared the estimated change in admissions among facilities that had effectively implemented PACT with the change in those that had done so less effectively. Results The final Pi2 consisted of 53 individual items assigned to the 8 overarching PACT concepts (Table 1). Detailed descriptions of all items and descriptive statistics are provided in eTable 1 in the Supplement. From more than 22 000 primary care per- sonnel at the time of the survey, 5404 (approximately 25% re- sponse rate) from 667 sites of care completed the PACT Pri- maryCarePersonnelSurveyduringthespringof2012.Between June and December 2012, more than 75 000 veterans who were enrolled in VA primary care completed the CAHPS PCMH mod- ule included in the Survey of the Health Experiences of Pa- tients (47% response rate). Psychometric Properties of Pi2 The Pi2 demonstrated satisfactory levels of internal consis- tency for total score (Cronbach α= 0.89), access (0.63), conti- nuity (0.67), comprehensiveness (0.81), self-management support (0.68), patient-centered care and communication (0.95), shared decision making (0.75), and team-based care (0.91). Similar to results reported by Scholle et al,16 the care coordination composite had lower internal consistency (0.51). With patient satisfaction as measured by the Survey of the Health Experiences of Patients used as a measure of con- vergent validity, provider ratings differed between sites with more vs less effective implementation (mean provider rating, 9.05 vs 8.37; P < .001). Variation in PCMH Adoption Clinical sites that had implemented PACT more effectively tended to have fewer patients than those that had been less effective (Table 2). However, the type of clinic, mean patient age, percentage of male patients, and mean Elixhauser comor- bidity score were similar among all sites irrespective of how well PACT had been implemented. Associations With Patient and Provider Outcomes Patient satisfaction was significantly higher among sites that had effectively implemented PACT than among those that had not (range of mean rating for satisfaction with provider, 9.33-7.53; P < .001) (Table 3 and the eFigure in the Supple- ment). A similarly favorable pattern was observed for staff burnout as measured by the Maslach Burnout Inventory Research Original Investigation Patient-Centered Medical Home Implementation E4 JAMA Internal Medicine Published online June 23, 2014 jamainternalmedicine.com Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
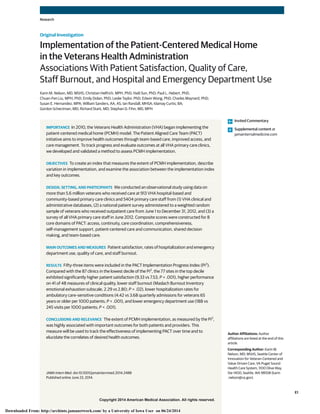
- 5. Copyright 2014 American Medical Association. All rights reserved. emotional exhaustion subscale (range, 2.29-2.80; P = .02) (Table 3 and the eFigure in the Supplement) but not for the 1-item burnout question. We observed significant trends in quality of care in rela- tion to the Pi2 score. The 77 sites that achieved the most ef- fective implementation exhibited higher clinical quality out- come measures than less successful sites. There was a statistically significant association (P < .05) between clinical quality outcomes and the Pi2 score for 19 of 48 measures, and better performance was associated with a higher Pi2 score for allbut2.Overall,ofall48measures,41werehigheramongsites with higher Pi2 scores. The Figure displays the difference in thepercentageofpatientsmeetingqualitycriteriabetweensites in the highest and lowest quintiles of Pi2 scores. The com- bined effect estimated from the mixed-effects model showed a significant increase in mean outcomes for facilities with higher Pi2 scores compared with those with lower Pi2 scores (P < .001). InthecomparisonoftrendsacrossPi2 scores,veteranswith chronic disease who received care at facilities with higher Pi2 scores had small but significant improvements in quality-of- care indicators (eTable 3 in the Supplement). For example, vet- erans with diabetes who received care at sites with the high- est Pi2 scores were more likely to have a hemoglobin A1c value less than 9% (range at high-implementation vs low- implementation sites, 84.0%-81.8%; P = .04) or a low- density lipoprotein cholesterol (LDL-C) level less than 100 mg/dL (to convert to millimoles per liter, multiply by 0.0259) (range,70.4%-66.0%;P = .03).Veteranswithhypertensionwere more likely to have a blood pressure reading less than 140/90 mm Hg (range, 80.2%-76.9%; P = .02). Among veterans with ischemicheartdisease,thoseatsiteswiththehighestPi2 scores were more likely to have LDL-C measured (range, 97.0%- 94%; P < .001), have a measured LDL-C level less than 100 mg/dL (range, 70.5%-65.3%; P < .001), and have documenta- tionofaprescriptionforaspirinattheirmostrecentvisit(range, 92.9%-89.5%; P = .03). Veterans receiving care at sites that ex- hibited more successful implementation of PACT were more likely to receive an influenza vaccination (range, 68.5%- 64.2%; P < .001 for veterans aged 50-64 years), to be screened for cervical cancer (range, 92.8%-86.7%; P = .047 for women aged 21-64 years), or offered medications for tobacco cessa- tion (range, 96.2%-93.4%; P < .001). The rate of emergency department visits was signifi- cantly lower in sites with more effective implementation than inthosewithlesseffectiveimplementation(range,188-245vis- its per 1000 patients; P < .001; Table 4 and eFigure in the Supplement). Although the total numbers of hospitalizations in fiscal year 2012 did not differ by level of implementation (Table 4), rates of hospitalization for ACSCs during the 2½- year period after implementation of PACT were lower among sites that had more effectively implemented PACT than among those that were less effective (Table 5). Among sites with Pi2 scoresinthehighestdecile,weestimatedthattherewasamean reduction of 2.28 admissions for ACSCs per 1000 patients younger than 65 years (a 13.4% decrease) attributable to the Table 2. Site Characteristics by Effectiveness of PACT Implementation Characteristic Clinic-Level National Mean (SD)a Implementation, Mean (95% CI)b P Valuec More Effective (Pi2 , 5 to 8) Less Effective (Pi2 , –7 to −5) Patients served, No. 5917 (6706) 2893 (2250-3535) 5467 (3910-7024) .004 CBOCs, No. (%) 735 (83.0) 72 (94.7) 73 (89.0) .19 Age, y 64.4 (3.9) 65.1 (64.2-66.0) 63.6 (62.7-64.4) .01 Female patients, % 5.4 (0.04) 6.2 (4.0-9.0) 5.9 (5.0-7.0) .77 Elixhauser score 0.76 (0.07) 0.77 (0.75-0.78) 0.76 (0.75-0.77) .43 Abbreviations: CBOCs, community-based outpatient clinics; PACT, Patient Aligned Care Team; Pi2 , PACT Implementation Progress Index. a Values represent mean (SD) except where otherwise indicated. b Values represent mean (95% CI) except where otherwise indicated. c P values determined with χ2 or t tests comparing more effective vs less effective implementation sites. Table 3. Patient Satisfaction, Staff Burnout, and Pi2 Scores Pi2 Score Clinics, No. Patient Satisfaction, Mean (SD) Staff Burnout, Mean (SD) Provider Rating From CAHPS PCMH Survey Provider Rating From SHEP Overall Health Care Rating From SHEP MBI EE Single-Item Measure 5 to 8 77 9.33 (0.34) 9.05 (0.28) 8.62 (0.34) 2.29 (1.55) 0.37 (0.36) 2 to 4 213 9.02 (0.44) 8.91 (0.34) 8.49 (0.36) 2.47 (1.29) 0.36 (0.33) −1 to 1 346 8.67 (0.46) 8.73 (0.34) 8.32 (0.35) 2.56 (1.13) 0.36 (0.29) −4 to −2 190 8.23 (0.64) 8.55 (0.40) 8.15 (0.40) 2.63 (1.23) 0.37 (0.29) −7 to −5 87 7.53 (0.88) 8.37 (0.45) 7.87 (0.47) 2.80 (1.42) 0.37 (0.35) P valuea … <.001 <.001 <.001 .02 .58 Abbreviations: CAHPS PCMH, Consumer Assessment of Health Plans–Patient Centered Medical Home; MBI EE, Maslach Burnout Inventory emotional exhaustion subscale; Pi2 , PACT [Patient Aligned Care Team] Implementation Progress Index; SHEP, Survey of the Health Experiences of Patients. a P values represent test for trend. Patient-Centered Medical Home Implementation Original Investigation Research jamainternalmedicine.com JAMA Internal Medicine Published online June 23, 2014 E5 Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 6. Copyright 2014 American Medical Association. All rights reserved. Figure. Differences Between Sites With More Effective and Less Effective Implementation in the Percentage of Patients Meeting Quality Criteria –6.00 0 8.00–2.00 2.00 6.004.00 % of Patients –4.00 Source Congestive heart failure LVF documented LVEF <40% on ACEI or ARB Diabetes mellitus Renal testing Hypertension Diagnosis of HTN and BP <140/90 mm Hg Mental health screening and treatment Alcohol misuse with timely counseling Obesity management Eligible patients who participated in MOVE Immunizations Immunization age ≥65 years Cancer and osteoporosis screening Colorectal cancer screening for those aged 51-75 years Tobacco use screening and treatment Patients using tobacco offered referral Patients using tobacco provided with counseling Patients using tobacco offered medications Screened for tobacco use Cervical cancer screening (women aged 21-64 years) Screened for breast cancer (women aged 40-49 years) Screened for breast cancer (women aged 60-69 years) Osteoporosis screening for women aged ≥65 years Screened for breast cancer (women aged 50-59 years) Influenza ages 50-64 years Pneumococcal Obese patients screened and offered weight management (MOVE) Annually screened for alcohol misuse, SUD Patients positive for PTSD with timely disposition Positive PTSD screen with timely suicide ideation/behavior evaluation PTSD screening using the PC-PTSD Combined scores for timely suicide evaluation if positive for PTSD or MDD Timely evaluation for patients with positive depression screen Annually screened for depression Ischemic heart disease AMI outpatient, ASA at most recent visit AMI, LVEF <40 on ACEI or ARB AMI discharged who received persistent β–blocker Hyperlipidemia screen–overall LDL-C <100 mg/dL LDL-C measured No diagnosis of HTN and BP <160/100 mm Hg Diagnosis of HTN and BP <160/100 mm Hg No diagnosis of HTN and BP ≤140/90 mm Hg LDL-C measured within 1 y of review Retinal examination, timely by disease BP <160/100 mm Hg BP <140/90 mm Hg LDL-C <100 mg/dL HbA1c <9% ACEI/ARB in current medications ASA in current medications HbA1c annual Foot sensory examination using monofilament Foot pedal pulses Foot inspection ACEI, angiotensin-converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, argiotensin II receptor blocker; ASA, aspirin; BP, blood pressure; HbA1c, hemoglobin A1c; HTN, hypertension; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; LVF, left ventricular fraction; MDD, major depressive disorder; MOVE, weight management program; PC-PTSD, primary care posttraumatic stress disorder; PTSD, posttraumatic stress disorder; SUD, substance use disorder. SI conversion factor: To convert LDL-C values to millimoles per liter, multiply by 0.0259. Research Original Investigation Patient-Centered Medical Home Implementation E6 JAMA Internal Medicine Published online June 23, 2014 jamainternalmedicine.com Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 7. Copyright 2014 American Medical Association. All rights reserved. PACT initiative compared with a reduction in admissions of only 0.08 for ACSCs (a 3.0% decrease) among sites with less effective implementation. Thus, the estimated reduction in hospitalizationsforACSCswassignificantlygreateratthemore effective sites, although the absolute number of admissions was relatively small (2.8 hospitalizations per 1000 patients). For veterans older than 65 years, the projected changes in ad- mission rates for ACSCs were more modest, and the differ- ence among sites was small. Similar trends of smaller magni- tude were noted for all-cause hospitalization. Discussion We constructed the Pi2 , a measure to assess progress in imple- menting PCMH in the VHA, using primary care personnel sur- veys, patient surveys, and administrative data. The index was favorably and meaningfully associated with important out- comes, including patient satisfaction, staff burnout, quality of care, hospitalizations, and emergency department visits. Pa- tient satisfaction was significantly greater (on the order of a fullpointhigherona0-10scale)andstaffburnoutloweratsites forwhichthePi2 indicatedmoreeffectiveimplementation.De- spite the overall high level of clinical care provided at the VHA, we found measurable differences between clinics by level of PCMH implementation in terms of the proportion of veterans meeting criteria for multiple measures of quality. In addition, sites with the highest Pi2 scores exhibited modestly lower rates of hospital admission for ACSCs and larger projected de- creases in rates of admission after the start of the VHA PACT initiative. These results are consistent with findings from a re- cent VHA study in which clinic directors’ reports about the medical home indicated that sites with better care coordina- tion and support for transition had lower rates of hospitaliza- tions for ACSCs.33 Previous studies have found a lack of association with measurements of structural and care processes in primary care and quality of care34,35 or patient experience.36 Thus, in devising a method to assess the degree of PCMH implemen- tation, we adopted an approach that differed substantially from the widely used NCQA recognition process, including patient-reported measures and using administrative data on access and continuity. We chose not to use the NCQA recogni- tion process for several reasons: the administrative burden is too high to determine certification for more than 900 clinics and much of the process relies on structural changes that have already been broadly implemented across the VA, there- fore diminishing the ability to discriminate among sites. Pre- vious authors have noted that the NCQA measurement for PCMH may not be able to differentiate on quality-of-care measures.10 In contrast, our measure of PCMH implementa- tion detects differences in quality across many clinics. Our data support the notion that the assessment of PCMH needs to include both patient-level and practice-level infrastructure measures.5,6,37 The VHA has a long-standing investment in infrastruc- ture considered a baseline prerequisite for a functioning PCMH, including a robust quality improvement and perfor- mance system.14 Our data are consistent with previous reports of the high quality of clinical care provided at the VHA.14,38 Paradoxically, this high baseline of quality makes it more difficult to demonstrate improvements than would probably be the case in other health systems where imple- mentation of PCMH has been evaluated and the baseline Table 4. Emergency Department Visits, Hospitalizations, and Pi2 Scores for Fiscal Year 2012 Pi2 Score Clinics, No. Emergency Department Visits per 1000 Patients, No.a Hospitalizations per 1000 Patients, No.a 5 to 8 77 188 68 2 to 4 213 227 77 −1 to 1 346 286 87 −4 to −2 190 289 83 −7 to −5 87 245 74 P valueb … <.001 .99 Abbreviation: Pi2 , PACT [Patient Aligned Care Team] Implementation Progress Index. a Adjusted for age, Elixhauser comorbidity score, and community-based outpatient clinics. b P values represent test for trend. Table 5. Effects of PACT Initiative Among Sites With More Effective or Less Effective Implementation for ACSC and Total Hospitalizations Pi2 Scorea Quarterly Hospital Admissions for ACSCs per 1000 Patients, No. Quarterly Total Hospital Admissions per 1000 Patients, No. Predicted With PACT Initiative Predicted Without PACT Initiative Absolute Difference, No. (%)b Predicted With PACT Initiative Predicted Without PACT Initiative Absolute Difference, No. (%) Patients <65 y 5 to 8 2.28 2.63 −0.35 (−13.4) 26.12 27.43 −1.31 (−4.8) −7 to −5 2.53 2.61 −0.08 (−3.0) 25.20 24.33 0.87 (3.6) Patients >65 y 5 to 8 3.68 3.85 −0.17 (−4.6) 21.75 22.21 −0.46 (−2.1) −7 to −5 4.42 4.33 0.09 (2.1) 23.47 22.37 1.10 (4.9) Abbreviations: ACSC, ambulatory care sensitive condition; PACT, Patient Aligned Care Team; Pi2 , PACT Implementation Progress Index. a Pi2 scores of 5 to 8 indicate more effective implementation; Pi2 scores of −7 to −5, less effective implementation. b All differences were significant at P < .001. Patient-Centered Medical Home Implementation Original Investigation Research jamainternalmedicine.com JAMA Internal Medicine Published online June 23, 2014 E7 Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 8. Copyright 2014 American Medical Association. All rights reserved. quality of care was substantially lower based on comparable measures.2 The favorable findings from our analysis may partly reflect the extensive improvements in clinical and resource infrastructure that the VHA has made since the 1990s, such as the use of electronic prescribing and a univer- sal electronic health record and deployment of pharmacists, dieticians, social workers, and mental health professionals in many primary care clinics. These analyses have several limitations. First, several of the domain scores rely on self-report, which are subject to biases, including response bias, framing bias, and others. However, we used well-validated measures, augmented these data with important team-based care domains from our primary care personnel survey, and used patient report to capture comprehensiveness of care that other measures may not include.15,39 Second, our primary care personnel survey had a low response rate, but our results were consistent with those from other surveys of primary care providers40,41 and with those from a survey of all VA employees. Third, the cross-sectional design of the study did not permit assessing change over time, although this is planned in future studies. Conclusions We found that the Pi2 score was favorably associated with pa- tientsatisfaction,staffburnout,qualityofcare,anduseofhealth care services. Our results may apply only to large integrated health systems that include a robust and integrated electronic health record and a well-developed quality improvement sys- tem that provides feedback to clinics and providers. All pri- mary care providers in the VHA, for example, have ready ac- cesstodetailedinformationabouttheirpatientpanels,including the likelihood of admission or death (updated weekly), as well as patients’ use of a range of inpatient, outpatient, and care co- ordination services.42 However, as accountable care organiza- tions evolve, this type of patient-centered measurement could be adopted by other large integrated health systems. ARTICLE INFORMATION Accepted for Publication: April 25, 2014. Published Online: June 23, 2014. doi:10.1001/jamainternmed.2014.2488. Author Affiliations: Seattle Center of Innovation for Veteran-Centered and Value-Driven Care, VA Puget Sound Health Care System, Seattle, Washington (Nelson, Helfrich, Sun, Hebert, Liu, Dolan, Taylor, Maynard, Hernandez, Randall); General Internal Medicine Service, VA Puget Sound Health Care System, Seattle, Washington (Nelson, Fihn); Department of Medicine, University of Washington School of Medicine, Seattle (Nelson, Fihn); Department of Health Services, University of Washington School of Public Health, Seattle (Helfrich, Sun, Hebert, Liu, Wong, Maynard, Hernandez, Randall); Office of Analytics and Business Intelligence, Veterans Health Administration, Washington, DC (Sanders, Curtis, Fihn); Office of Patient Care Services, US Department of Veterans Affairs, Washington, DC (Schectman); Office of Clinical Operations, US Department of Veterans Affairs, Washington, DC (Stark). Author Contributions: Dr Nelson had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Nelson, Helfrich, Hebert, Dolan, Wong, Hernandez, Schectman, Stark, Fihn. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Nelson, Helfrich, Sanders, Fihn. Critical revision of the manuscript for important intellectual content: Nelson, Helfrich, Sun, Hebert, Liu, Dolan, Taylor, Wong, Maynard, Hernandez, Sanders, Randall, Curtis, Schectman, Stark, Fihn. Statistical analysis: Nelson, Sun, Hebert, Liu, Dolan, Taylor, Wong, Maynard, Sanders, Randall. Obtained funding: Fihn. Administrative, technical, or material support: Nelson, Helfrich, Dolan, Hernandez, Sanders, Randall, Curtis, Schectman, Stark, Fihn. Study supervision: Nelson, Schectman, Fihn. Conflict of Interest Disclosures: None reported. Funding/Support: This work was supported by the VHA Office of Patient Care Service. Role of the Sponsors: This study was conducted as part of VHA Health Care Operations in accordance with VHA Handbooks 1605.1 and 1605.2. The study team had full responsibility for the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation of the manuscript. The study was reviewed through normal administrative channels. Additional Contributions: Data for this report were developed by the national evaluation team at the PACT Demonstration Lab Coordinating Center and the VHA Office of Analytics and Business Intelligence. The VHA Office of Primary Care Operations is responsible for PACT implementation, and the VHA Office of Patient Care Services is responsible for the PACT Demonstration Lab program. John Messina, BA, was paid to assist with data acquisition and administrative support. Previous Presentation: This study was presented at the Society for General Internal Medicine Annual Meeting; April 25, 2014; San Diego, California. This study was also presented at the Academy Health National Meeting; June 10, 2014; San Diego, California. REFERENCES 1. Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601-612. 2. Werner RM, Duggan M, Duey K, Zhu J, Stuart EA. The patient-centered medical home: an evaluation of a single private payer demonstration in New Jersey. Med Care. 2013;51(6):487-493. 3. Nielsen M, Langner B, Zema C, Hacker T, Grundy P. Benefits of implementing the primary care patient-centered medical home: a review of cost & quality results, 2012. http://www.pcpcc.org/guide /benefits-implementing-primary-care-medical-home. Patient-Centered Primary Care Collaborative, September 2012. Accessed May 7, 2014. 4. Liss DT, Fishman PA, Rutter CM, et al. Outcomes among chronically ill adults in a medical home prototype. Am J Manag Care. 2013;19(10):e348-e358. 5. Day J, Scammon DL, Kim J, et al. Quality, satisfaction, and financial efficiency associated with elements of primary care practice transformation: preliminary findings. Ann Fam Med. 2013;11(suppl 1): S50-S59. 6. Jaén CR, Ferrer RL, Miller WL, et al. Patient outcomes at 26 months in the patient-centered medical home National Demonstration Project. Ann Fam Med. 2010;8(suppl 1):S57-S67, S92. 7. Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;15(9):e71-e87. 8. Jackson GL, Powers BJ, Chatterjee R, et al. The patient-centered medical home: a systematic review. Ann Intern Med. 2013;158(3):169-178. 9. Solberg LI, Asche SE, Fontaine P, Flottemesch TJ, Anderson LH. Trends in quality during medical home transformation. Ann Fam Med. 2011;9(6):515-521. 10. Solberg LI, Asche SE, Fontaine P, Flottemesch TJ, Pawlson LG, Scholle SH. Relationship of clinic medical home scores to quality and patient experience. J Ambul Care Manage. 2011;34(1):57-66. 11. Rosland AM, Nelson K, Sun H, et al. The patient-centered medical home in the Veterans Health Administration. Am J Manag Care. 2013;19 (7):e263-e272. 12. Berenson RA, Hammons T, Gans DN, et al. A house is not a home: keeping patients at the center of practice redesign. Health Aff (Millwood). 2008;27(5):1219-1230. 13. Kizer KW. The “new VA”: a national laboratory for health care quality management. Am J Med Quality. 1999;14(1):3-20. 14. Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218-2227. 15. Burton RA, Devers KJ, Berenson RA. Patient-centered medical home recognition tools: a comparison of ten surveys’ content and operational details. http://www.urban.org /publications/412338.html. Washington, DC: Urban Institute; 2012. Accessed February 1, 2014. Research Original Investigation Patient-Centered Medical Home Implementation E8 JAMA Internal Medicine Published online June 23, 2014 jamainternalmedicine.com Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
- 9. Copyright 2014 American Medical Association. All rights reserved. 16. Scholle SH, Vuong O, Ding L, et al. Development of and field test results for the CAHPS PCMH Survey. Med Care. 2012;50(suppl):S2-S10. 17. Wright SM, Craig T, Campbell S, Schaefer J, Humble C. Patient satisfaction of female and male users of Veterans Health Administration services. J Gen Intern Med. 2006;21(3)(suppl 3):S26-S32. 18. Helfrich CD, Dolan ED, Simonetti J, et al. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. J Gen Intern Med. 2014. doi:10.1007/s11606-013-2702-z. 19. Shen Y, Hendricks A, Zhang S, Kazis LE. VHA enrollees’ health care coverage and use of care. Med Care Res Rev. 2003;60(2):253-267. 20. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manag Care. 2004;10(11, pt 2):828-836. 21. Schaufeli WB, Enzmann D, Girault N. Measurement of burnout: a review. In: Schaufeli WB, ed. Professional Burnout: Recent Developments in Theory and Research. Philadelphia, PA: Taylor & Francis; 1993:199-215. 22. Wheeler DL, Vassar M, Worley JA, Barnes LL. A reliability generalization meta-analysis of coefficient alpha for the Maslach Burnout Inventory. Educ Psychol Meas. 2011;71(1):231-244. doi:10.1177/0013164410391579. 23. Maslach C, Jackson SE. The measurement of experienced burnout. J Organiz Behav. 1981;2(2) 99-113. doi:10.1002/job.4030020205. 24. Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75-79. doi:10.1002/smi .1002. 25. Leiter MP, Shaughnessy K. The areas of worklife model of burnout: tests of mediation relationships. Ergonomia. 2006;28:327-341. 26. Goulet JL, Erdos J, Kancir S, et al. Measuring performance directly using the Veterans Health Administration electronic medical record: a comparison with external peer review. Med Care. 2007;45(1):73-79. 27. Agency for Healthcare Research and Quality. Prevention quality indicators. http://www .qualityindicators.ahrq.gov/modules/pqi_resources .aspx. Accessed February 28, 2014. 28. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. 29. Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4(1):87-90. 30. Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. 2001;29:1165-1188. 31. Hebert PLLC, Wong ES, Hernandez SE, et al. The economic effects and return on investment of the Veterans Health Administration’s Patient Centered Home Initiative, 2010 through 2012. Health Aff. In press. 32. Liu CF, Chapko M, Bryson CL, et al. Use of outpatient care in Veterans Health Administration and Medicare among veterans receiving primary care in community-based and hospital outpatient clinics. Health Serv Res. 2010;45(5, pt 1):1268-1286. 33. Yoon J, Rose DE, Canelo I, et al. Medical home features of VHA primary care clinics and avoidable hospitalizations. J Gen Intern Med. 2013;28(9):1188- 1194. 34. Holmboe ES, Arnold GK, Weng W, Lipner R. Current yardsticks may be inadequate for measuring quality improvements from the medical home. Health Aff (Millwood). 2010;29(5):859-866. 35. Friedberg MW, Safran DG, Coltin KL, Dresser M, Schneider EC. Readiness for the patient-centered medical home: structural capabilities of Massachusetts primary care practices. J Gen Intern Med. 2009;24(2):162-169. 36. Martsolf GR, Alexander JA, Shi Y, et al. The patient-centered medical home and patient experience. Health Serv Res. 2012;47(6):2273-2295. 37. Gray BM, Weng W, Holmboe ES. An assessment of patient-based and practice infrastructure-based measures of the patient-centered medical home: do we need to ask the patient? Health Serv Res. 2012;47(1, pt 1):4-21. 38. Kerr EA, Gerzoff RB, Krein SL, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med. 2004;141(4):272-281. 39. Birnberg JM, Drum ML, Huang ES, et al. Development of a safety net medical home scale for clinics. J Gen Intern Med. 2011;26(12):1418-1425. 40. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. 41. Lewis SE, Nocon RS, Tang H, et al. Patient-centered medical home characteristics and staff morale in safety net clinics. Arch Intern Med. 2012;172(1):23-31. 42. Wang L, Porter B, Maynard C, et al. Predicting risk of hospitalization or death among patients receiving primary care in the Veterans Health Administration. Med Care. 2013;51(4):368-373. Patient-Centered Medical Home Implementation Original Investigation Research jamainternalmedicine.com JAMA Internal Medicine Published online June 23, 2014 E9 Copyright 2014 American Medical Association. All rights reserved. Downloaded From: http://archinte.jamanetwork.com/ by a University of Iowa User on 06/24/2014
