Odontogenic infections (4)
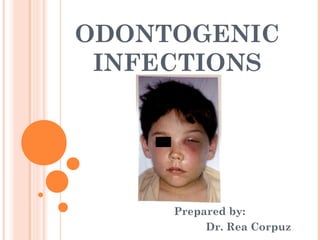
- 1. ODONTOGENIC INFECTIONS Prepared by: Dr. Rea Corpuz
- 2. Odontogenic Infections (1) Cellulitis (2) Ludwig’s Angina (3) Cavernous Sinus Thrombosis (4) Osteomyelitis
- 3. (1) Cellulitis if abscess is NOT able to establish drainage through the surface of skin or into oral cavity may spread diffusely through facial planes of soft tissue acute + edematous spread of acute inflammatory process
- 4. (1) Cellulitis two dangerous forms: Ludwig’s Angina Cavernous Sinus Thrombosis
- 5. (2) Ludwig’s Angina named after German physician who described the seriousness of disorder in 1836 Angina comes from Latin word angere strangle
- 6. (2) Ludwig’s Angina 70% of cases, develop from spread of an acute infection from lower molar teeth prevalence in patients who are immunocompromised secondary to disorders such as: diabetes mellitus organ transplantation acquired immunodeficiency syndrome (AIDS) aplastic anemia
- 7. (2) Ludwig’s Angina Clinical Features massive swelling on neck often extends close to clavicle involvement of sublingual space results in • elevation Woody Tongue • posterior enlargement can compromise • protrusion of tongue airway
- 9. (2) Ludwig’s Angina Clinical Features involvement of submandibular space results in • enlargement • tenderness of neck above level of hyoid bone Bull Neck • pain in neck + floor of mouth • restricted neck movement
- 10. (2) Ludwig’s Angina Clinical Features involvement of submandibular space results in • dysphagia • dysphonia • dysarthria • drooling • sore throat
- 11. (2) Ludwig’s Angina Clinical Features involvement of lateral pharyngeal space • respiratory obstruction secondary to laryngeal edema • tachypnea • dyspnea • tachycardia • patient needs to maintain erect position
- 12. (2) Ludwig’s Angina Treatment & Prognosis centers around 4 activities • maintenance of airway • incision + drainage • antibiotic therapy • elimination of original focus of inflammation
- 13. (2) Ludwig’s Angina Treatment & Prognosis initial observation many clinicians administer • systemic corticosteroid medications such as intravenous (IV) dexamethasone attempt to reduce cellulitis
- 14. (2) Ludwig’s Angina Treatment & Prognosis if signs or symptoms of impending airway obstruction: • fiber-optic nasotracheal intubation • tracheostomy • cricothyroidotomy
- 15. (2) Ludwig’s Angina Treatment & Prognosis if signs or symptoms of impending airway obstruction: • cricothyroidotomy sometimes performed instead of tracheostomy perceived lower risk of spreading infection to mediastinum
- 16. (2) Ludwig’s Angina Treatment & Prognosis • cricothyroidotomy
- 17. (2) Ludwig’s Angina Treatment & Prognosis high dose of penicillin penicillin- Clindamycin OR sensitive Choramphenicol patients anitbiotic medication is adjusted according to patient’s response + culture result from aspirates of fluid from enlargement
- 18. (2) Ludwig’s Angina Treatment & Prognosis if infection remains: diffuse surgical intervention indurated is at discretion of clinician brawny + often governed by patient’s response to noninvasive therapy
- 19. (2) Ludwig’s Angina Treatment & Prognosis complications: • Pericarditis • Pneumonia • Mediastinitis • Sepsis • Empyema • Respiratory Obstruction
- 20. (3) Cavernous Sinus Thrombosis edematous periorbital enlargement with involvement of eyelids + conjunctiva
- 21. (3) Cavernous Sinus Thrombosis in cases, involving canine space swelling along lateral border of nose may extend up to medial aspect of eye + periorbital area protrusion + fixation of eyeball
- 22. (3) Cavernous Sinus Thrombosis in cases, involving canine space induration + swelling of adjacent forehead + nose pupil dilation lacrimation may also photophobia occur loss of vision
- 23. (3) Cavernous Sinus Thrombosis in cases, involving canine space pain over eye + along distribution of: • opthalmic Trigeminal • maxillary branches Nerve
- 24. (3) Cavernous Sinus Thrombosis Treatment & Prognosis surgical drainage + high-dose antibiotic medication similar to those administered for patient’s with Ludwig’s Angina
- 25. (4) Osteomyelitis an acute or chronic inflammatory process in extends medullary spaces OR away from cortical surfaces of bone initial site of involvement
- 26. (4) Osteomyelitis caused by bacterial infections result in expanding lytic destruction of involved bone with suppuration sequestra formation
- 27. (4) Osteomyelitis patients of all ages can be affected strong male predominance most cases involves mandible
- 28. (4) Osteomyelitis Acute Supporative Osteomyelitis Chronic Suppporative Osteomyelitis
- 29. (4) Osteomyelitis (Acute Supporative Osteomyelitis) acute inflammatory process spreads through medullary spaces of bone insufficient time has passed for body to react to presence of inflammatory infiltrate
- 30. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Clinical Features symptoms of acute inflammatory process less than1 month in duration fever leukocytosis
- 31. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Clinical Features lymphadenopathy soft tissue swelling of affected area on occasion, paresthesia of lower lip
- 32. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Histopathologic Features biopsy material from patients • liquid content • lack of soft tissue component • consist predominantly of necrotic bone
- 33. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Histopathologic Features necrotic bone • loss of osteocytes • peripheral resorption • bacterial colonization • acute inflammatory infiltrate consists of polymorphonuclear leukocytes
- 34. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Radiographic Features ill- defined radioluscency periosteal new bone formation may be seen • response to subperiosteal spread of infection • proliferations more common in young patients
- 35. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Radiographic Features periosteal new bone formation may be seen • single-layered radioopaque line • separated from normal cortex by an intervening radiolucent band
- 36. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Radiographic Features on occasion, exfoliation of fragments of necrotic bone fragment of necrotic bone that has separated from adjacent vital bone is teremed sequestrum
- 37. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Radiographic Features on occasion, fragments of necrotic bone may become surrounded by new vital bone, known as involucrum
- 38. (4) Osteomyelitis (Acute Supporative Osteomyelitis) Treatment if obvious abscess formation, • antibiotics penicillin clindamycin cephalexin cefotaxime gentamicin • drainage
- 39. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) defensive response leads to production of granulation tissue subsequent forms dense scar tissue • attempt to wall off infected area
- 40. (4) Osteomyelitis (Chronic Supporative Osteomyelitis)
- 41. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) subsequent forms dense scar tissue • encircled dead space acts as reservoir for bacteria • antibiotic medications have great difficulty reaching the site
- 42. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Clinical Features if acute osteomyelitis is not resolved expeditiously entrenchment of chronic osteomyelitis occurs sometimes may arise without previous acute episode
- 43. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Clinical Features swelling pain sinus formation purulent discharge sequestrum formation tooth loss pathologic fracture
- 44. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Clinical Features may experience acute exacerbations or periods of decreased pain associated with chronic smoldering progression
- 45. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Histophathologic Features biopsy material from patient • soft tissue component • consists of chronically or subacutely inflammed connective tissue filling the intertrabecular areas of bone • scattered sequestra + pockets of abscess formation
- 46. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Radiographic Features patchy ragged ill-defined radiolucency • often contains central radiopaque sequestra
- 47. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Radiographic Features
- 48. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Treatment difficult to manage medically • pockets of dead bone • organisms are protected from antibiotic drugs due to surrounding wall of fibrous connective tissue
- 49. (4) Osteomyelitis (Chronic Supporative Osteomyelitis) Treatment surgical intervention is mandatory antibiotic medications are similar to those used in acute form • but must be given intravenously in high doses
- 50. References: Books Neville, et. al: Oral and Maxillofacial Pathology 3rd Edition • (pages 138-144)
