Investigations of d m
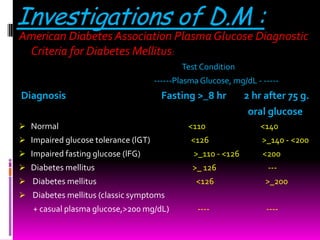
- 1. Investigations of D.M : American Diabetes Association Plasma Glucose Diagnostic Criteria for Diabetes Mellitus: Test Condition ------Plasma Glucose, mg/dL - ----- Diagnosis Fasting >_8 hr 2 hr after 75 g. oral glucose Normal <110 <140 Impaired glucose tolerance (lGT) <126 >_140 - <200 Impaired fasting glucose (lFG) >_110 - <126 <200 Diabetes mellitus >_ 126 --- Diabetes mellitus <126 >_200 Diabetes mellitus (classic symptoms + casual plasma glucose,>200 mg/dL) ---- ----
- 3. 1. Testing for diabetes should be considered in all persons at age 45 years and older; if results are normal, testing should be repeated at 3·yr intervals. 2. Testing should be considered at younger ages or performed more frequently in: • are obese ( >_20% desirable body weight or a BMI >_25 kg/m2) • have a first-degree relative with diabetes • are members of a high-risk ethnic population (eg, African American. Hispanic American, Native American, Asian American, Pacific Islander) • have delivered a baby weighing >9 Ib or have a diagnosis of gestational D.M • are hypertensive (>_140/90 mm Hg) • have an HDL cholesterol level <_35 mg/dL and/or a triglyceride level >_250 mg/ dL • were shown to have impaired glucose tolerance or impaired fasting glucose • have polycystic ovary syndrome • have history of vascular disease • are habitually physically inactive
- 4. Management the strategies of RX. Include: Glycemic control diet & exercise insulin therapy oral agents other therapies treatment of associated conditions. dyslipidemia HT obesity CHD treatment of complications
- 5. The goals of therapy : (1) eliminate symptoms related to hyperglycemia, (2) reduce or eliminate the long-term microvascular and macrovascular complications of DM. (3) allow the patient to achieve as normal a lifestyle as possible. To reach these goals, the physician should identify a target level of glycemic control for each patient. Index Goal Glycemic control <11.1 mmol/L (200 mg/dL) Hb A1C <7.0 Blood pressure <130/80 Lipids LDL <2.6 mmol/L (<100mg/dL) HDL >1.1 mmol/L (>40 mg/dL) TG <1.7 mmol/L (<150 mg/dL)
- 6. The care of an individual with either type 1 or type 2 DM requires a multidisciplinary team. Central to the success of this team are the patient's participation, which is essential for optimal diabetes management. Members of the health care team include the primary care provider and/or the endocrinologist or diabetologist, a certified diabetes educator, and a nutritionist. In addition, when the complications of DM arise, subspecialists (including neurologists,nephrologists, vascular surgeons, cardiologists, ophthalmologists, and pediatrics) with experience in DM-related complications are essential.
- 7. Diet & exercise : Adherence to nutrition and meal-planning principles is a challenging but essential component of successful diabetes management. Diet planning should include lifestyle and nutrition goals as well as specific biochemical and other physiologic parameters for the individual. Insulin requirements are then matched to the patient's diet, not vice versa. If type 2 diabetes is diagnosed and the patient is overweight. a diet that is prudently low fat and low cholesterol should be started and an exercise routine initiated but even a modest weight loss of 10- 20 pounds may ameliorate the diabetes or cause its remission. Before an exercise program is prescribed for anyone older than age 35. a determination must be made that the heart is normal and that there are no contraindications. Bariatric surgery-surgery that promotes weight loss-is a popular option for very obese individuals who are unresponsive to other forms of therapy. There are 3 general techniques for bariatric surgery: restrictive surgery. which restricts stomach volume; malabsorptive surgery. which minimizes the ability of the gastrointestinal tract to absorb nutrients; and a combination of restrictive and malabsorptive approaches.
- 8. Insulin therapy : This therapy usually involves use of a longer-acting insulin to maintain a baseline level and then use of a rapid-acting insulin to cover meals. Current insulin preparations are generated by recombinant DNA technology and consist of the amino acid sequence of human insulin. Animal insulin (beef or pork) is no longer used. In the United States, most insulin is formulated as U-100 (100 units/mL) Regular insulin is the traditional rapid-acting agent used for short-term coverage; however, the development of very rapid-acting insulins allows diabetic patients the convenience of timing injections just a few minutes before meals.
- 9. Very rapid-acting insulins include insulin lispro (Humalog), insulin aspart (NovoLog), and insulin glulisine (Apidra). Isophane insulin suspension (NPH insulin) is an intermediate-acting insulin. The newer long-acting insulins with very stable absorption characteristics that result in a constant level of basal insulin include Glargine (Lantus) and detemir (Levemir) Insulin zinc suspension (Lente insulin) and extended insulin zinc (Ultralente insulin) are no longer available. Premixed combinations of various insulins are also available for patients less able to work with all these variables. One commonly used regimen consists of twice-daily injections of a long-acting insulin like NPH (detemir could be used instead) mixed with a short-acting insulin before the morning and evening meal. Such regimens usually prescribe two-thirds of the total daily insulin dose in the morning (with about two-thirds given as long-acting insulin and one-third as short-acting) and one-third before the evening meal (with approximately one-half given as long-acting insulin and one-half as short-acting).
- 10. Pharmacokinetics of Insulin Preparations Time of Action Preparation Onset, h Peak, h Effective Duration, h Short-acting Lispro <0.25 0.5–1.5 3–4 Aspart <0.25 0.5–1.5 3–4 Glulisine <0.25 0.5–1.5 3–4 Regular 0.5–1.0 2–3 4–6 Long-acting NPH 1–4 6–10 10–16 Detemir 1–4 — 12–20 Glargine 1–4 — 24 Insulin Combinations 75/25– 75% protamine lispro, 25% lispro Up to 10–16 70/30– 70% protamine aspart, 30% aspart Up to 10–16 50/50– 50% protamine lispro, 50% lispro Up to 10–16 70/30– 70% NPH, 30% regular insulin 10–16 50/50– 50% NPH, 50% regular insulin 10–16
- 11. Continuous subcutaneous insulin infusion (CSII) pumps allow even more physiologic levels of insulin than do traditional injections. The pump tends to be used when multiple-injection therapy fails. Disadvantages include a higher cost, infection at the infusion site, and infusion failure. Complications of insulin therapy • Hypoglycemia • Lipodystrophy • Local insulin allergy • Generalized anaphylaxis, hives, and angioedema may also develop. • Immunologic insulin resistance may occur because of production of insulin-neutralizing antibodies
- 12. Oral agents: * Sulfonylureas: The sulfonylureas have been widely used in the United States and Canada since 1967 for treatment of type 2 diabetes. Their major mechanism of action is stimulation of pancreatic insulin secretion, although some studies have suggested a peripheral augmentation of insulin action. The most significant adverse effect of this drug is hypoglycemia, which, though infrequent, may be severe and prolonged, depending on the half-life of the specific drug. Second-generation sulfonylurea are approximately 50-100 times more potent than first-generation agents, and these drugs generally need to be given only once daily.
- 13. *Biguanides A major advance occurred with the development of metformin (Glucophage. Glucophage XR). currently the only available biguanide. Metformin improves insulin sensitivity. it may also lead to modest weight loss or at least stabilization (in contrast to the weight gain that may occur with use of insulin or sulfonylureas). In addition it is less likely to cause hypoglycemia and can be used in nonobese patients. Metformin is generally the first agent used in patients whose hyperglycemia cannot be controlled with lifestyle changes alone. Although metformin is generally very safe, patients may complain of gastrointestinal tract symptoms, including a metallic taste, nausea, and diarrhea. A more severe potential problem is lactic acidosis. Although rare, this problem is more likely to occur in patients with renal insufficiency.
- 14. * a-Glucosidase inhibitors Acarbose (Precose) and miglitol (Glyset) are administered with meals to delay digestion and absorption of carbohydrates by inhibiting the enzymes that convert complex carbohydrates into monosaccharides. Although relatively safe, these agents often cause flatulence, which limits patient compliance, and they are to be avoided in patients with intestinal disorders. * Thiazolidinediones This new class of orally active drugs, represented by rosiglitazone (Avandia) and pioglitazone (Actos), is thought to increase insulin sensitivity in muscle and adipose tissue and to inhibit hepatic gluconeogenesis, thereby increasing glycemic control while reducing circulating insulin levels. These drugs also act to increase insulin secretion. The first available agent of this class, troglitazone (Rezulin), was withdrawn from the market in 2000, when the FDA noted that this drug had a higher rate of liver toxicity than did the other drugs. In 2010, the FDA significantly restricted the use of rosiglitazone because of an increased risk of cardiovascular complications in patients using this drug. Both rosiglitazone and pioglitazone can cause weight gain, in part owing to the proliferation of new adipocytes. Another problem is fluid retention, which has been associated with cases of macular edema.
- 15. *Meglitinides Repaglinide (Prandin) and nateglinide (Starlix) are meglitinides, whose mechanism of action and side effect profile are similar to those of the sulfonylureas. However, they are more expensive and generally no more efficacious than the sulfonylureas. Because of their rapid onset of action and short duration, these agents are taken daily with meals. They can be used as Single agents or in combination therapy with other oral hypoglycemic agents. * Other therapies Incretins are gut-derived factors that are released when nutrients enter the stomach; they help to stimulate postprandial insulin release. Incretin mimetics improve glycemic control by enhancing pancreatic secretion of insulin in response to nutrient intake, Inhibiting glucagon secretion and promoting early satiety. Two recently approved injectable incretin mimetics are exenatide (Byetta). used as adjunctive therapy for patients with type 2 diabetes who are inadequately controlled by oral agents. and pramlintide (Symlin). a synthetic analogue of amylin. used in patients treated with mealtime insulin.
- 16. Dipeptidyl peptidase IV (DPP-IV) is an enzyme that deactivates bioactive peptides including incretins; therefore inhibiting this enzyme can enhance glucose regulation. Sitagliptin (Januvia) is an oral DPP-IV inhibitor that requires only once a day dosing. But it is expensive. only modestly effective. and not commonly used. Glucose transport inhibitors are a new class of drugs. Glucose is filtered in the renal glomerulus and reabsorbed in the proximal tubule. Beyond a certain threshold (usually 160- 180 mgldL). it is excreted in the urine. Glucose transport inhibitors prevent the reabsorption and thereby increase the loss of glucose in the urine. The lost calories then cause weight loss and improved blood glucose values.
- 17. Pharmacokinetics of Oral Hypoglycemic Drugs Drug Usual Daily Dose, mg Dosing per Day First-generation sulfonylureas Acetohexamide 500-750 Once or divided Chlorpropamide (Dabinese) 250-500 Once Tolbutamide (Orinase) 1000-2000 Once or divided Second-generation sulfonylureas Glipizide (Glucotrol) 2.5-10 Once or divided (Glueotrol XL) 5-10 Once Glyburide (DiaBeta, Micronase, 2.5-10 Once or divided Glynase) Glimepiride (Amaryl) 2-4 Once Biguanides Metformin (Glucophage, 1500-2550 Twice to 3 times Glueophage XR) a-Glucosidase inhibitors Acarbose (Precose) 150-300 3 times Miglitol (Glyset) 150-300 3 times Thiazolidinediones Rosiglitazone (Avandia) 4-8 Once or divided Pioglitazone (Actos) 15-45 Once Meglitinides Repaglinide (Prandin) 2-16 3 times w/meals Nateglinide (Starlix) 360 3 times w/meals Other Sitagliptin (Januvia) 100 Once
- 18. Is a pancreas transplantation is possible ???
- 19. Pancreatic transplantation For type I diabetic patients, pancreas transplantation can be performed in conjunction with renal transplantation. With modern techniques and immunosuppression, there is a high transplant survival rate, and the majority of patients become euglycemic without the need for insulin. Islet cells can be injected directly into the liver without the need for formal transplantation. This procedure has been attempted in humans, but rejection leads to a high failure rate. Studies are under way to identify effective immunosuppressive regimens as well as other sites for cell placement. Islet cell- producing stem cell research is still at a basic stage.
- 20. The Importance of Glucose Control ³ The Diabetes Control and Complications Trial showed that intensive therapy aimed at maintaining near-normal glucose levels had a large and beneficial effect on delaying the development and retarding the progression of long-term complications for type 1 diabetic patients. Intensive therapy decreased the risk of the development and progression of retinopathy, nephropathy, and neuropathy by 40%-76%.. ³ A related study, the United Kingdom Prospective Diabetes Study (UKPDS), was designed to assess the effect of intensive control on patients with type 2 diabetes. The UKPDS showed a reduction in complications. the risk of retinopathy progression rises almost exponentially as the HbA1c increases. However, patients who decrease their HbAjc by 1 percentage point (eg, from 8% to 7%) decrease the risk of retinopathy approximately 30%, and this benefit holds for other diabetic complications, such as nephropathy and neuropathy.
- 21. ³ For patients with type 1 diabetes, intensive control also provides protection against macrovascular complications, such as cardiovascular disease. For patients with type 2 diabetes, A recent study, suggested that intensive glycemic control in patients with type 2 diabetes might actually increase the risk of cardiovascular mortality. ³ Studies have shown that poor control can increase the rate of retinopathy progression after cataract surgery and blunt the treatment response to laser for diabetic macular edema.
- 22. Guidelines for Ongoing Medical Care for Patients with Diabetes: † Self-monitoring of blood glucose (individualized frequency) † HbA1C testing (2–4 times/year) † Patient education in diabetes management (annual) † Medical nutrition therapy and education (annual) † Eye examination (annual) † Foot examination (1–2 times/year by physician; daily by patient) † Screening for diabetic nephropathy (annual) † Blood pressure measurement (quarterly) † Lipid profile and serum creatinine (estimate GFR) (annual) † Influenza/pneumococcal immunizations † Consider antiplatelet therapy
- 23. THANK YOU & HAVE A NICE DAY