Empyema
- 1. EMPYEMA
- 3. •
- 4. • The bacteria traditionally associated with parapneumonic empyema are Streptococcus pneumonia, Streptococcus pyogenes, Staphylococcus aureus, and, more recently, Streptococcus anginosus (formerly Streptococcus milleri). Anaerobes have been identified as sole or coexisting pathogens in 25% to 76% of cases. A recent review of the NIS database between 1996 and 2008 characterized the changing epidemiology of parapneumonic empyema in community hospitals across the United States. The largest increase in relative incidence of empyema occurred in young adults. The most serious cases of empyema were associated with staphylococcal infections. For patients older than 40 years, staphylococcal empyema had a significantly higher in- hospital mortality rate than those associated with other pathogens.
- 5. • The incidence of pneumococcal empyema has remained relatively stable in both children and adults. Infant vaccination with a seven-valent pneumococcal conjugate vaccine (PCV7) started in 2000.11-14 Studies documented significant reductions in the incidence of pneumonia hospitalizations after the introduction of this vaccine The introduction of a 13-valent pneumococcal conjugate vaccine in 2010 in the United States may provide protection against several pneumococcal serotypes commonly associated with empyema
- 6. • Some studies using molecular techniques have suggested that a significant percentage of culture-negative empyema may be caused by pneumococci, mainly serotype 1.19-23 Although recent studies suggest Streptococcus anginosus may be a leading cause of empyema,24-26 it can be difficult to distinguish between streptococcal species. Mixed bacterial infections are found in some parapneumonic empyemas.
- 7. • PATHOGENESIS Classically, the development of empyema occurs in three clinical stages: • the exudative stage, • the fibrinopurulent stage, and • the organizing stage.
- 8. • When initially presented with an infectious organism, the pleura responds with edema formation, and exudation of proteins and neutrophils into the pleural space. Inflammatory cytokines result in increased pleural mesothelial and capillary cells permeability, resulting in an effusion. Activated by bacteria, mesothelial cells act as phagocytes and trigger an inflammatory cascade with the release of chemokines, cytokines, oxidants, and proteases. Polymorphonuclear cells are recruited.1
- 9. • Early in the exudative stage, bacterial growth may be minimal, and the exudate may be sterile. The rapidity of progression depends on the type and virulence of the organism, host defenses, and initiation of antibiotic treatment. Staphylococcal pneumonias are almost always associated with pleural effusions. With uncomplicated parapneumonic effusions, the pleural fluid has a pH greater than 7.20, relatively normal glucose levels, and lactate dehydrogenase (LDH) levels that, although elevated, are typically less than 3 times the upper limit of normal. Most patients with uncomplicated parapneumonic effusions respond to antibiotics alone
- 10. • Untreated exudative effusions may develop into fibrinopurulent effusions or complex parapneumonic effusions. The fibrinopurulent stage represents the deposition of fibrin on visceral and parietal pleural membranes and the formation of loculations. Ongoing phagocytosis and cell lysis result in pleural fluid with a pH less than 7.20, LDH levels more than 3 times normal, and low glucose. A complex parapneumonic effusion develops into a pleural empyema when the concentration of leukocytes becomes sufficient to form frank pus. Empyema fluid consists of fibrin, cellular debris, and viable or dead bacteria. As fibrin is deposited into the pleural space, lymphatic channels may become occluded, further increasing the amount of pleural fluid. The fibrin strands result in loculations of the pleural space, which prevent drainage of the pleural fluid using a single needle or tube.30 This stage is more likely to result in a positive Gram stain and/or positive bacterial cultures. This stage of pleural effusion requires catheter drainage and often surgical drainage
- 11. • The third and final phase is the organizing phase. This stage is characterized by the influx of fibroblasts and the formation of a thick, fibrous pleural peel along with continued maturation of dense septations. Both the visceral and the parietal pleura may become severely thickened with significant fluid remaining in the pleural space. During this stage of disease, simple drainage of the fluid may be possible, but the thick peel prevents reexpansion of the underlying lung. Failure of the “trapped” lung to reexpand will not allow for improved aeration of the lung or any improvement in breathing. The residual space quickly refills with infected fluid
- 12. •
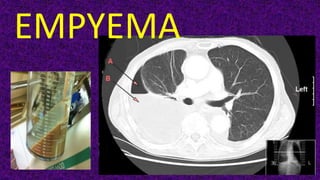
- 13. • Chest x-ray demonstrates multiple air fluid levels in the lower part of the right hemithorax. This is associated with patchy areas of consolidation, possibly with areas of cavitation. The left side is unremarkable
- 14. • CT demonstrates a large sub- pulmonic collection with consolidation of the compressed lung above.
- 15. •
- 16. • VATS decortication in pleural empyema stage II. a) Pre-operative CT of the thorax; b–d) operative views with multiple intrapleural loculations. 1: lung; 2: chest wall; 3: sub- pulmonary fibrin collection.
- 17. • Radiographic features • Plain radiograph • Can resemble a pleural effusion and can mimic a peripheral pulmonary abscess, although a number of features usually enable distinction between the two (see empyema vs lung abscess) 3. Pleural fluid is typically unilateral or markedly asymmetric 4. Generally, empyemas form an obtuse angle with the chest wall, and due to their lenticular shape are much larger in one projection (e.g. frontal) compared to the orthogonal projection (e.g. lateral) 3. The lenticular shape (biconvex) is also suggestive of the diagnosis, as transudative/sterile pleural effusions tend to be crescentic in shape (i.e. concave towards the lung, see empyema vs pleural effusion).
- 18. •
- 19. • Distinguishing between an empyema and a peripherally located pulmonary abscess is essential. • Lung abscesses are usually managed with prolonged antibiotics and physiotherapy with postural drainage whereas an empyema usually requires percutaneous or surgical drainage.
- 20. • Radiographic features • Plain radiograph • shape – abscess is usually (but not always) round in all projections – an abscess may form an acute angle with the costal surface / chest wall – empyema is usually (but not always) lentiform
- 21. • CT • relationship to adjacent bronchi/vessels – abscesses will abruptly interrupt the bronchovascular structures – empyema will usually distort and compress adjacent lung • split pleura sign – thickening and separation of visceral and parietal pleura is a sign of empyema • wall – abscesses have thick irregular walls – empyema are usually smoother • angle with pleura – abscesses usually have an acute angle (claw sign) – empyema tends to have obtuse angles • pleural enhancement – empyemas tend to show more pleural enhancement. • edema or hazyness of extrapleural fat - tends to occur with empyema
- 23. •
- 24. •
- 25. • CT • Typically appears as a fluid density collection in the pleural space, sometimes with locules of gas. They form obtuse angles with the adjacent lung, which is displaced and compressed. The pleura is thickened due to fibrin deposition and in-growth of vessels with enhancement. At the margins of the empyema, the pleura can be seen dividing into parietal and visceral layers, the so-called split pleura sign, which is the most sensitive and specific sign on CT, and is helpful in distinguishing an empyema from a peripheral lung abscess (see: empyema vs lung abscess) 2- 3. The inner walls of the empyema are smooth. There may be increased density and haziness of the extrapleural and extrathoracic fat
- 26. •
- 27. • DIAGNOSIS: CLINICAL SIGNS AND SYMPTOMS, FLUID ANALYSIS, AND RADIOLOGIC APPEARANCE The clinical presentation may vary depending on the underlying bacterial cause. Patients with aerobic infections tend to be more acutely ill with an initial presentation similar to that of pneumonia. This can be followed by a nonresolving picture with pleuritic chest pain, fever spikes, and failure to improve after receiving appropriate antibiotic therapy. Immunocompromised patients, older adults, and those with anaerobic infections may have a more indolent course and may experience weight loss, cough, fever, and anemia.25 The pleural effusions are generally evident on upright chest radiographs. Lateral decubitus films are useful in determining whether the fluid is free flowing and amenable to complete percutaneous drainage.
- 28. • The presence of leukocytosis, radiographic evidence of a pleural effusion, and the presence of purulent fluid on thoracentesis are classic findings of empyema. Signs or symptoms of infection, history of malignancy, or associated medical diseases such as cardiac failure or kidney or liver disease can be helpful in determining the cause of an effusion.
- 29. • Ultrasound can detect loculations and can determine an appropriate site for thoracentesis. A computed axial tomographic (CAT) scan can determine the size and the location of the effusion and provides information regarding associated underlying parenchymal and pleural abnormalities. A CAT scan with intravenous contrast can further characterize the empyema, suggesting loculations or a thickened pleura or rind. Inspection of the lung-fluid interface may suggest entrapped lung and may reveal an underlying parenchymal process such as an abscess or tumor. The appearance of the effusion and fluid-lung interface can give indications as to the need for operative intervention
- 30. •
- 31. •
- 32. •
- 33. • Thoracentesis is useful in determining the cause of an effusion. Pleural fluid evaluation should include a cytologic evaluation, pH level, gram stain and culture, cell count, and total protein, glucose, and LDH levels. Effusions are classified as exudative or transudative based on protein and LDH levels. Exudate effusions will have a pleural fluid protein/serum protein level higher than 0.5 and a pleural fluid LDH/serum LDH level higher than 0.6. The presence of an increased white blood cell count in the pleural fluid, particularly with a preponderance of neutrophils, may indicate pleural infection. Low pleural fluid glucose and a pH less than 7.20 are indicators of active pleural infection and the need for pleural drainage
- 34. •
- 35. •
- 36. •
- 37. •
- 38. • TREATMENT Initial antibiotic coverage of patients with parapneumonic effusions is generally dictated by treatment guidelines for pneumonia and may be modified according to blood and pleural fluid microbial cultures and sensitivities. Empiric anaerobic antibiotic coverage may be initiated although anaerobes are much less likely to be cultured. Patients with nosocomial empyema need adequate gram-negative coverage. Vancomycin may be added for suspected methicillin-resistant infection. Reported bacteriology of pleural sepsis varies significantly between community acquired and nosocomial infections.30 Early appropriate antibiotic therapy represents the cornerstone of therapy for pneumonia and parapneumonic effusion. Minimal size free-flowing effusions may be observed without a diagnostic aspiration because the risk of a complicated course is remote. All other freeflowing effusions should be aspirated for diagnostic purposes
- 39. • Uncomplicated parapneumonic, exudative effusions that are of small volume, free flowing without loculations, with a negative Gram stain, pH greater than 7.20, and negative cultures are usually inflammatory in nature. Most of these resolve with antibiotic treatment of the underlying pneumonia and can be observed without formal drainage.1 Early drainage of pleural fluid becomes necessary when a parapneumonic effusion advances beyond the exudative stage to the fibrinopurulent stage and becomes a complicated parapneumonic effusion. Indications for immediate drainage are large effusions (larger than half the hemithorax), effusions with loculations, pH less than 7.20, positive Gram stain or culture, and low glucose levels. The presence of frank pus on aspiration is also an indication for immediate and complete drainage
- 40. • Options for drainage include serial thoracenteses, tube thoracostomy (with or without intrapleural fibrinolytics), thoracoscopic drainage, thoracotomy and drainage (decortication), and chronic open drainage. • Choice of drainage is dependent on the viscosity of the pleural fluid; location, volume, and extent of loculations; and the general condition of the patient
- 41. • In theory, in the absence of loculations, either thoracentesis or tube thoracostomy should adequately drain any fluid. With significant ongoing infection and inflammation, however, continued production of fluid will occur, requiring repeat thoracentesis. Serial thoracenteses are generally not recommended. Using such strategy, one study showed that the average patient required 7.7 aspirates with an average hospital stay of 31 days.31 Tube thoracostomy is generally performed with a size 24 to 32 Fr chest tube placed in a dependent area (usually the posterior costophrenic recess). If pleural infection is confirmed and all fluid is drained, then the tube is generally left in place until drainage is very low, typically less than 30 to 40 mL/day.
- 42. • Complicated parapneumonic effusions and empyema are characterized by a procoagulant state within the pleural space, which results in the progressive development of dense layers of fibrin and loculations, as discussed earlier. These complex loculated effusions are unlikely to be adequately drained with simple tube thoracostomy. In an attempt to aid drainage of loculated areas of empyema, instillation of fibrinolytic agents via the chest tube has been proposed as a means of avoiding operation
- 43. • Intrapleural instillation of fibrinolytic agents can theoretically dissolve fibrinous clots and adhesions and prevent pleural loculations. The use of fibrinolytic agents is appealing because the most common reason for failure of pleural drainage among patients with an appropriately positioned catheter is occlusion of the catheter by viscous fibrin-rich fluid and/or debris, or partitioning of the pleural space with fibrin bands that loculate pleural fluid and prevent it from reaching the chest tube. Side effects with fibrinolytics are minimal with rare reports of fever and bleeding.
- 44. • Streptokinase, urokinase, and tissue plasminogen activator have all been instilled via chest tube. Streptokinase is usually administered as 250,000 IU in 100 to 200 mL saline daily for up to 7 days. Urokinase is usually administered as 100,000 to 200,000 IU in 100 mL saline daily up to 3 days. Tissue plasminogen activator is administered as 10 to 25 mg twice daily up to 3 days. Drains are typically clamped for several hours following the administration of the fibrinolytic. Tissue plasminogen activator, a recombinant agent, provides fibrinolytic activity without the risk of antigenic-based reactions that can be seen with repeated administration of streptokinase
- 45. • Tuncozgur and colleagues34 looked at fibrinolytic versus saline instillation via chest tube in 49 patients. They found a significantly lower decortication rate (60% vs. 29%) and shorter duration of hospitalization (14 vs. 21 days) with the addition of intrapleural fibrinolysis as well as a greater volume of chest tube drainage (1.8 liters vs. 0.8 liters). It should be noted, however, that even a 14-day hospital stay is considerably longer than what is expected following an expeditious video-assisted thoracic surgery (VATS) decortication. A single-center randomized placebo- controlled study by Diacon and colleagues32 reported that intrapleural streptokinase resulted in faster resolution of infection, reduced need for surgery (13.6% vs. 45.5%), and improved outcomes in patients with complex parapneumonic effusions and empyema.
- 46. • Davies and colleagues35 compared fibrinolysis versus saline control in the second to fifth hospital day in 24 patients with tube thoracostomy for empyema. These investigators looked at volume of drainage and improvement in chest radiographs. Fibrinolytics caused an increased rate of fluid drainage and greater improvement on chest radiograph. No bleeding complications were seen. Three patients in the control group and none in the fibrinolytic group required surgical drainage
- 47. •
- 48. •
- 49. • Surgical drainage via thoracoscopy is indicated in patients who fail chest tube drainage, in patients whose lung does not reexpand following either thoracentesis or tube thoracostomy, or as the initial treatment in patients who, based on chest computed tomography (CT) appearance, are unlikely to be effectively treated with a chest tube. These include patients with very loculated effusions, patients with thick pus, or with a thick pleural rind on CT scan. Loculations can be broken down, thick pleural fluid and debris completely evacuated, the pleural space can be extensively lavaged, and chest tubes can be carefully placed. Several small retrospective and nonblinded prospective studies suggest that thoracoscopy is superior to tube thoracostomy with fibrinolytics, with the need for thoracotomy halved
- 50. • In the only prospective randomized controlled trial of fibrinolytic therapy versus thoracoscopy for empyema, Wait and coworkers41 randomly assigned 20 patients with complicated multiloculated parapneumonic empyema to streptokinase (250,000 IU daily for 3 days) via tube thoracostomy or immediate thoracoscopic drainage. Thoracoscopy had a higher treatment success rate (91% vs. 44%), lower duration of chest tube drainage (5.8 vs. 9.8 days), and a shorter hospital stay (8.7 vs. 12.8 days). This study supports the preferred approach of primary thoracoscopic drainage in patients presenting with loculated collections, provided that they are suitable candidates for surgical intervention.
- 51. • Often in the chronic organizing phase of empyema, a thick fibrous peel builds up on the visceral pleura that restricts lung mechanics and prevents lung reexpansion, even after fluid drainage. The procedure allows for excision of all the fibrous tissue from the pleura to permit lung reexpansion.42 Decortication relies on lung elasticity to fill the cavity. Failure of reexpansion of the lung in the acute phase may result when there is densely consolidated lung that does not fully reexpand after drainage of fluid, even with decortication. Lung constriction after empyema can reduce lung perfusion by 20% to 25% on the involved side
- 52. • The pulmonary function of patients who undergo decortication can increase significantly. Decortication can improve lung perfusion and improve vital capacity from 62% up to 80% and the forced expiratory volume after 1 second (FEV1) from 50% to 69%. Nonetheless, decortication remains a procedure with significant morbidity and a reported mortality rate of up to 10%.42 Some investigators have suggested that pleural thickening may resolve over time and recommend deferring decortication for up to 6 months, but this opinion is in the minority.43 In patients suffering from overwhelming sepsis, pleural drainage by tube thoracostomy or expeditious VATS is the immediate goal. Decortication may then be performed at a later date when the patient is stable. Delayed decortication is advised if there remains significant restriction of the affected lung and if the patient is a good operative risk.
- 53. • For patients in whom sepsis cannot be controlled acutely with thoracoscopic drainage and in whom decortication is not appropriate, window thoracostomy may be performed. Open thoracostomy may be the procedure of choice if there is a permanent supply of causative organisms as a result of a bronchopleural fistula or if there is a space issue such as in a postpneumonectomy empyema
- 57. •
- 59. •
- 60. •
- 61. • Case Report • A 66-year-old man was referred to the authors’ department due to a bronchopleural fistula of the main bronchus. The fistula occurred three months after a left pneumonectomy that he underwent in another center for a pulmonary adenocarcinoma. The patient reported fever, dyspnea, and cough with mucopurulent sputum. Chest radiography demonstrated a drop in the air-fluid level and a computed tomography scan showed a fistulous communication that was confirmed by bronchoscopy. Parenteral antibiotic therapy was imposed. A pleural drainage (18 Fr) was positioned and repeated irrigations with betadine solutions were performed without benefit. Surgical indication for a left thoracostomy was thus given.
- 62. • Surgical Procedure • Under general anesthesia, the patient was placed in the standard right lateral decubitus position. • An “H-shaped” skin incision was made in the fourth intercostal space, and subcutaneous tissues were dissected to reach the muscular layer. Latissimus dorsi and pectoralis major muscles were identified and spared. The third rib was isolated and cut. The thickened parietal pleura was digitally opened. The pleural cavity appeared full of purulent material, and the bronchopleural fistula was clearly visible. The fourth and second ribs were then isolated and removed to enlarge the thoracostomy and to create an easy-to- pack drainage cavity. The pleural cavity was then deeply cleaned and debrided, and the purulent material was removed. Washings with saline solution and betadine were performed. Finally, the skin flaps were sutured directly to the parietal pleura with interrupted absorbable sutures anchored to the ribs stumps. This served to epithelialize the thoracostomy borders and maintain the patency of the window, improving the healing. The margins were sutured. After that, the bronchial fistula was covered with a sponge, and betadine-soaked gauzes were plugged into the pleural cavity. The cavity was thus packed, and the wound was dressed. During the hospital stay, the patient underwent daily dressing changes to ensure the sterilization of the cavity and to eradicate the local sepsis.
- 63. • Bronchial stump closure with staples had a protective effect against BPF compared with suture closure. Factors not affecting the incidence of PPE or BPF were gender, age, smoking history, associated cardiovascular disease, corticosteroid use, chronic renal failure, diabetes mellitus, hematologic disease, cirrhosis, nonpulmonary malignancy, body mass index, weight loss, stage, preoperative chemotherapy or radiation therapy, preoperative percentage of predicted total lung capacity and residual volume, PaO2, and PaCO2, extended resection, and duration of postoperative mechanical ventilation
- 64. • The signs and symptoms of postpneumonectomy empyema initially consist of low-grade fever, malaise, and leukocytosis. The appearance of air in the pleural fluid after pneumonectomy is nondiagnostic; however, a drop in the air-fluid level is strongly suggestive of a BPF even in the absence of other symptoms. Computed tomography can be helpful in demonstrating the size and location of loculated air-fluid pockets. It may also show reversal of the normal concavity of the mediastinal margin with increased thickening of the residual parietal pleura.50,51 Air in continuity with the bronchial stump may raise suspicion of a BPF but is not diagnostic. Bronchoscopy should be performed if the diagnosis of empyema is suspected after pulmonary resection. The bronchial stump should be thoroughly inspected for a small BPF. Similarly, the contralateral airway should be inspected and sputum collected for cultures.
- 65. • Staphylococcus aureus and Pseudomonas aeruginosa are the organisms most frequently involved.49 In patients with suspected early empyema who have no evidence of a fistula, systemic antibiotics and observation may be the most appropriate management option. In cases of confirmed postpneumonectomy empyema, however, treatment follows the well-established rules of managing any abscess.49 These management rules include adequate pleural drainage, appropriate parenteral antibiotics, removal of necrotic tissue, and obliteration of residual space. Obliteration of the empyema space can be accomplished by transposition of viable tissue such as omentum or skeletal muscle; this can be performed as a primary procedure to manage an empyema space or as a staged procedure some months after an open thoracostomy.
- 69. • Treatment When the patient presents acutely with clinical features of a BPF, contralateral pneumonitis, and respiratory distress, initial management begins with emergency chest tube drainage of the cavity to control infection and stop contralateral spillage. The patient should be positioned in the lateral decubitus position with the pneumonectomy side down until adequate drainage of the pleural space is achieved. Simultaneously, respiratory support is provided as clinically needed. When a large BPF is present and mechanical ventilation is required, a doublelumen endotracheal tube or a straight, long single-lumen tube is used to ventilate the remaining lung and bypass the fistula.
- 70. • The ventilation of these patients can be extremely challenging. If the fistula occurs in the perioperative period (i.e., within the first month or so), repeat thoracotomy and attempted closure of the stump with muscle flap reinforcement and drainage of the pleural space are recommended. After this time, scarring and granulation tissue prevent the precise placement of bronchial stump sutures. Other treatment options include thoracoplasty,52-54 open pleural drainage,55-57 and transsternal, transpericardial closure of the fistula.58-60 If bronchoscopy reveals a long main bronchus stump (i.e., >1 cm), then transsternal, transpericardial closure with a thoracoabdominal (TA) stapler may be a good option.
- 71. • Rarely, carinal resections have been used for treatment of a pneumonectomy stump BPF.61 Clagett and Geraci in 196362 showed that post-pneumonectomy empyema could be successfully treated by open pleural drainage, frequent wet-to-dry dressing changes, and, when the thorax was clean, secondary chest wall closure with obliteration of the pleural cavity with an antibiotic solution. Failure was most often due to a persistent or recurrent fistula.60 Because of this, the original Clagett technique is modified when a BPF is present to include transposition of a well-vascularized muscle to cover the stump at the time of open drainage to prevent further ischemia and necrosis.63
- 72. • Our preference is intrathoracic transposition of extrathoracic skeletal muscle.63-67 Usually, the serratus anterior muscle is intact despite a previous thoracotomy. Other available muscles include the pectoralis major, the cephalic portion of the previously transected latissimus dorsi, and the rectus abdominis. The advantages of using these muscles include adequate bulk, an axial blood supply, and the muscle’s availability in the same visceral cavity. Transposition of the latissimus dorsi and pectoralis major muscles results in minimal cosmetic or functional abnormality; transposition of the serratus anterior muscle, however, may result in scapular winging.
- 73. • CONCLUSIONS Patients with pneumonia and associated pleural effusion should initially be evaluated with thoracentesis. Presence of loculations or pleural fluid analysis showing bacteria on Gram stain or culture, low glucose or low pH, and frank pus are all indications for immediate drainage. Nonloculated parapneumonic effusion and empyema may be adequately treated with tube thoracoscopy, but loculated effusions, or those inadequately drained with a chest tube, are best treated with thoracoscopic drainage. The fundamental principles of therapy are to remove infection and allow for lung reexpansion to obliterate dead space. If visceral scarring results in lung entrapment, then decortication is required. With recent advances in
- 74. • VATS technology and skills, most decortications can be performed using minimally invasive techniques. Open decortication is usually reserved for patients with severe scarring after remote pleural empyema. If a significant pleural space exists and decortication is not possible, then the options are thoracoplasty, muscle flap transposition, or open window drainage
- 75. • BPF is a communication between the pleural space and the bronchial tree or lung parenchyma resulting in air leak in the chest tubes. It might be divided into alveolopleural fistula (APF) or bronchopleural fistula (BPF). An APF is a communication between the pulmonary parenchyma distal to a segmental bronchus and the pleural space, while a BPF is a communication between a main stem, lobar, or segmental bronchus and the pleural space. The term BPF is used for any air leak which failed to heal conservatively and progressed to chronicity. Chronic BPF is a serious complication of several pulmonary and postoperative conditions, as it carries a high morbidity and mortality and is associated with prolonged hospital stay and thus high resource consumption. The treatment of BPF includes control of infection, pleural space drainage, surgical interventions and bronchoscopic interventions. Till date surgical intervention has been the main stay of management of chronic BPF
- 76. • Modified silicone stent for the treatment of post- surgical bronchopleural fistula: a clinical observation of 17 cases
- 77. • Background • Bronchopleural fistula is a rare but life-threatening event with limited therapeutic options. We aimed to investigate the efficacy and safety of the modified silicone stent in patients with post-surgical bronchopleural fistula. • Methods • Between March 2016 and April 2020, we retrospectively reviewed the records of 17 patients with bronchopleural fistula and who underwent bronchoscopic placement of the Y-shaped silicone stent. The rate of initial success, clinical success and clinical cure, and complications were analyzed.
- 78. • Results • Stent placement was successful in 16 patients in the first attempt (initial success rate: 94.1%). The median follow-up time was 107 (range, 5–431) days. All patients achieved amelioration of respiratory symptoms. The clinical success rate was 76.5%. Of the 14 patients with empyema, the daily drainage was progressively decreased in 11 patients, and empyema completely disappeared in six patients. Seven stents were removed during follow-up: four (26.7%) for the cure of fistula, two for severe proliferation of granulomatous tissue and one for stent dislocation. No severe adverse events (i.e. massive hemoptysis, suture dehiscence) took place. Seven patients died (due to progression of malignancy, uncontrolled infection, myocardial infarction and left heart failure). • Conclusions • The modified silicone stent may be an effective and safe option for patients with post-surgical bronchopleural fistula patients in whom conventional therapy is contraindicated.
- 79. •
- 80. • Illustration of the modified silicone stent. a The modified silicone stent consists of the main branch, the lateral branch and the occluded branch; b the stent rings are sutured to the main branch and the lateral branch of silicone stent; c the stent ring is sutured to the occluded branch
- 82. • The bronchoscopic view of the stent placement in a representative case. Patient 5 is a 72-year-old male with BPF. a Bronchoscopic image of fistula in the left main bronchus and the drainage tube could be seen from the fistula (arrow); b the straight stent segment is used to measure the diameter of the left main bronchus; c bronchoscopic image of the carina, left main bronchus and right main bronchus after stenting; d the inner surface of the occluded branch
- 83. • The coronal computer tomography image of patient 5 in different time. a The fistula in the left main bronchus (arrow) and the drainage tube (arrow head) is placed in the left thoracic cavity; b the occluded branch of the stent can be seen in the left main bronchus (arrow) and the drainage tube (arrow head) is still in the left thoracic cavity; c the residual pleural space diminishes over time; d the residual pleural space disappears during follow-up
- 85. Background: Bronchopleural fistula (BPF) is a communication between the pleural space and the bronchial tree or lung paren- chyma resulting in air leak in the chest tubes. Chronic BPF is a serious complication of several pulmonary and postoperative conditions, as it carries a high morbidity and mortality and is associated with prolonged hospital stay and thus high resource consumption. Till date surgical intervention has been the main stay of management of chronic BPF. This study was carried out to assess the efficacy of surgical closure of the chronic BPF using vascularized tissue transfer into the pleural cavity.
- 86. Patients and methods: 28 patients were operated upon primarily due to chronic BPF with or without empyema. All patients were selected and subjected to surgical intervention using vascularized tissue transfer into the pleural cavity. The vascularized tissues had been used were: Intercostal muscle flap, Latissmus dorsi muscle transposition, Omental flap, and Pericardial pad of fat. Results: The mean hospital stay postoperatively was 4 ± 1 day. There was immediate or early stoppage of air leak after the intervention in all patients. No patient had prolonged postoperative air leak (5 days). One patient required negative suction for 2 days to help stoppage of the leak. No patient required instillation of sealants through the tubes.
- 87. •
- 96. • A) Pedicled intercostal muscle flap, IMF (B) ruptured pulmonary sarcoidosis cyst before closure with IMF (C) completely dissected and • isolated right sided latismus dorsi muscle, LDM, with preservation of its vascular pedicle (D) longitudinal skin incision along the anterior border • of LDM (E) operative view for the anatomy of pericardial pad of fat (F) omental flap passed through the foramin of Morgagni to be directed • toward the pleural cavity.
