Rotationplasty
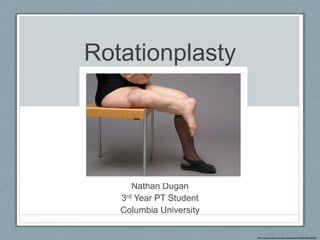
- 1. Rotationplasty Nathan Dugan 3rd Year PT Student Columbia University http://www.hindawi.com/journals/sarcoma/2008/402378/fig4/
- 2. Objectives • Explain what rotationplasty is and how it is performed • Discuss rehabilitation options for rotationplasty • Discuss prosthetics relating to rotationplasty • Review outcome measures that may be beneficial to administer in this population • Present conclusions drawn during the course of compiling this presentation related to research and outcomes in rotationplasty
- 4. What is Rotationplasty? • Biologic reconstructive option for congenital and acquired lower extremity bone loss • Indicated for: • Proximal femoral focal deficiency (PFFD) • Sarcomas of hip, femur, proximal tibia • Failed limb salvage procedures, failed THA/TKA • Traumatic bone loss • Severe burns with intact distal limb Gupta 2012
- 5. Types of Rotationplasty • Type A • ankle joint functions as knee joint • Type B • knee joint functions as hip joint, ankle joint functions as new knee joint Gupta 2012
- 6. Type A Rotationplasty • Type AI • distal femoral resection • Type AII • proximal tibial resection Gupta 2012
- 7. Type B Rotationplasty • Type BI • proximal femoral conditions with no hip involvement • Type BII • performed in the setting of hip joint or lower pelvis involvement Gupta 2012
- 8. Type B Rotationplasty • Type BIII • performed when complete resection of the femur is necessary • Type BIIIa • lateral condyle of the tibia is placed into the acetabulum (expected to remodel) • Type BIIIb • tibia is rotated and connected to pelvis with endoprosthesis Gupta 2012
- 9. Type B Rotationplasty • Type BIIIa • Type BIIIb Gupta 2012
- 11. Rehabilitation
- 12. Rehabilitation Course: General Guidelines • Gentle PROM of the ankle and AROM/antigravity movements of hip important early-on in process • Want to avoid hip flexion/adduction contractures, similar to AKA • Functional training with assistive devices • Progress to AROM of ankle/toes • Resisted exercise typically begins 6-12 weeks post-op, when soft tissue healing is complete • Advance to weight-bearing once there is evidence of healing at osteotomy site Gupta 2012, So 2014
- 13. Rehabilitation Course: Considerations • Full weight-bearing is not allowed until osteotomy site is fully healed • AROM 0-30 degrees is needed to operate knee in prosthesis (optimal PF/KE is 50 degrees) • Be mindful of pain post-operatively Gupta 2012, So 2014
- 15. Prosthetics
- 16. Rehabilitation Course: Prostheses • Retrospective observational study with n=12 • Median age: 10 years (5-13 yrs), 8 males • All patients had oncologic pathology • Osteosarcoma (10), synovial sarcoma (2) So 2014
- 17. Rehabilitation Course: Prostheses • Preliminary bypass prosthesis • Allows TTWB without shearing at osteotomy site • Bypasses “knee” joint • No “knee” flexion through prosthesis • Must use assistive device to ambulate • Components: • Polypropylene, ischial WB, quadrilateral sockets • Total elastic auxiliary suspension • Pylon and Seattle LightFoot So 2014
- 19. Rehabilitation Course: Prostheses • Definitive prosthesis • Acrylic laminate socket with polypropylene thigh section • Anatomic suspension • Calcaneal strap • Removable calcaneal wedge • Seattle LightFoot So 2014
- 20. First Definitive Prosthesis So 2014
- 21. How Long Did it Take? • In 10 patients requiring chemotherapy • 230.5 days • In 2 patient not requiring chemotherapy • 78.5 days • Time between first and second prosthesis • 18.5 months So 2014
- 22. Considerations for Prostheses • Stops for ankle (“knee”) flex/ext • Compensates for patient’s inability to control knee flexion moment at heel strike • Use longest foot that can fit in shoe • Provides a longer lever arm, assists in knee stability • Subsequent prostheses can incorporate carbon fiber dynamic response/multiaxial foot options • Allow for easy adjustments to compensate for growth So 2014
- 23. Innovation in Prosthetics • In cycling, thigh cuff of a conventional prosthesis leads to perspiration, chaffing, and skin abrasion • Case of an 18 y/o male cyclist with rotationplasty • He regularly contracted abrasion injuries at foot/thigh • Only able to cycle 35km (21.7mi) Scheepers 2015
- 26. Outcome Measures
- 27. Outcomes Assessment • FMA (functional motor assessment), MSTS (musculoskeletal tumor society) rating scale, Toronto Extremity salvage score (TESS) • SF-36v2 • Gait analysis, TUG, 6MWT, ROM, MMT, etc.
- 28. Functional Motor Assessment (FMA) • Six subcategories: • Pain • Function with two specific measures • Timed up-and-down 12 stairs (TUDS) • Timed up-and-go (TUG) • Supports • Satisfaction with walking quality • Participation in work, school, sports • Endurance • 9-minute walk-run test Marchese 2007
- 29. Musculoskeletal Tumor Society (MSTS) Rating Scale • Also known as Enneking Score • Examines 6 factors • Pain • Functional activities • Emotional acceptance • Use of supports • Walking ability • Gait Enneking 1993
- 30. Toronto Extremity Salvage Score (TESS) • Disease-specific measure developed for patients undergoing limb preservation surgery for tumors of the extremities • Evaluates physical disability based on patients’ reports of their function • 29-item lower extremity and 28-item upper extremity questionnaire • Items rated on 5-point scale from “not at all difficult” to “impossible to do” • Importance of each item is rated on 4-point scale from “totally unimportant” to “extremely important” Davis 1996
- 31. Conclusions
- 32. An Overall Paucity of Research • Search on PubMed for “rotationplasty” yields only 154 results since 1962 • Only 2.9 articles per year • Overall quality of research is low • Results yield many case studies/case series and few, if any, RCTs • Virtually no mention of rehabilitation in the research • At best, a few sentences within other studies mentioning generalities • Research is concentrated in the areas of surgical techniques/complications, quality of life, and function
- 33. Highly Functional Individuals • Individuals have been shown to be highly functional post-rotationplasty • Hillman 2007, Harris 2013 • Individuals often score highly on quality of life measures • Forni 2012, Barrera 2012, Rödl 2002
- 35. Questions?
- 36. References 1. Gupta SK, Alassaf N, Harrop AR, Kiefer GN. Principles of rotationplasty. J Am Acad Orthop Surg 2012;20:657-667. 2. So NF, Andrews KL, Anderson K, et al. Prosthetic fitting after rotationplasty of the knee. Am J Phys Med Rehabil 2014;93:328-334. 3. Scheepers LG, Storcken JO, Rings F, et al. New socket-less prosthesis concept facilitating comfortable and abrasion-free cycling after Van Nes rotationplasty. Prosthet Orthot Int 2015;39(2):161- 165. 4. Davis AM, Wright JG, Williams JI, et al. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual Life Res 1996;5:508-516 5. Marchese VG, Rai SN, Carlson CA, et al. Assessing functional mobility in survivors of lower-extremity sarcoma: reliability and validity of a new assessment tool. Pediatr Blood Cancer 2007;49:183- 189. 6. Enneking WF, Dunham W, Gebhardt MC, et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat R 1993;286:241-246. 7. Hillman A, Weist R, Fromme A, et al. Sports activities and endurance capacity of bone tumor patients after rotationplasty. Arch Phys Med Rehabil 2007;88(7):885-890. 8. Harris JD, Trinh TQ, Scharschmidt TJ, Mayerson JL. Exceptional functional recovery and return to high-impact sports after Van Nes Rotationplasty. Orthopedics 2013;36(1):126-131. 9. Forni C, Gaudenzi N, Zoli M, et al. Living with rotationplasty – quality of life in rotationplasty patients from childhood to adulthood. J Surg Oncol 2012;105(4):331-336. 10. Barrera M, Teall T, Barr R, et al. Health related quality of life in adolescent and young adult survivors of lower extremity bone tumors. Pediatr Blood Cancer 2012;58(2):265-273. 11. Rödl RW, Pohlmann U, Gosheger G, et al. Rotationplasty – quality of life after 10 years in 22 patients. Acta Orthop Scand 2002;73(1):85-88.
Notes de l'éditeur
- Rotationplasty is defined as, “a biologic reconstruction option for congenital and acquired lower extremity bone loss.” It is indicated in many conditions of varying etiologies, including proximal femoral focal deficiency, or PFFD, sarcomas of the hip, femur, and proximal tibia (this etiology is why it is most important to us, here), failed limb salvage procedures and failed arthroplasties, traumatic bone loss, and severe burns with an intact distal limb.
- There are two types of rotationplasty, A and B. Type A is the type that I’m sure we are all more acquainted with. In this type, the lower extremity is altered in such a way that the ankle joint functions as the new knee joint, when the knee joint is compromised by one of the disorders or injuries listed on the previous slide. In a type B rotationplasty, the knee joint is moved proximally to function as a new hip joint, while the ankle is moved proximally to function as the new knee.
- Within each type of roatationplasty, there are various subtypes. A type AI rotationplasty refers to a procedure in which the distal femur is compromised and resected. Type AII rotationplasty refers to a procedure in which the proximal tibia is compromised and resected. You can appreciate from the pictures that the osteotomy is reattached in a different location relative to the ankle joint in these two types.
- There are many variations of type B rotationplasty, and recall that these involve moving the knee joint proximally to form a new hip joint, in addition to moving the ankle joint proximally to form a new knee joint. Type BI refers to pathology that does not involve the hip, and type BII refers to pathology that involves the hip or lower pelvis.
- The final variation of rotationplasty is type BIII, and this is performed when complete resection of the femur is necessary. In a type BIIIa rotationplasty, the lateral condyle of the tibia is place into the acetabulum and is expected to remodel – because of this, it is typically performed in children. In a type BIIIb rotationplasty, typically performed in older individuals, the tibia is rotated and connected to the pelvis with an endoprosthesis.
- Here are pictures illustrating types BIIIa and BIIIb.
- I’m going to now describe the typical surgical process for a knee rotationplasty, or type A. First, the surgeons make two oblique elliptical incisions in the thigh and leg. Then, the hamstring and heads of the gastroc are identified, along with the popliteal artery/vein, and the tibial and common peroneal nerves. The nerves are protracted, the hamstrings divided to achieve adequate margins. The gastroc is detached from the femoral condyles, and care is taken to preserve the primary blood supply from sural arteries. The femoral artery and sciatic nerve are dissected proximally to the femoral osteotomy site. The surgeons then transect the medial and anterior muscle compartments of the thigh at the level of the femoral osteotomy. The soleus is detached from the tibia, and the anterior and lateral muscle groups are cut at the level of the distal osteotomy. The distal segment is externally rotated 180 degrees, and it is ensured that the neurovascular structures move medially without tension. Osseous fixation is performed. Soft tissue is repaired using heavy sutures. The quadriceps tendon is attached to the gastroc-soleus complex, and the hamstrings are attached to the peroneal and tibialis anterior muscles. The ankle is kept in neutral to achieve optimum tension. The vessels and nerve are coiled and placed within a soft-tissue bed in the antero-medial thigh. This represents a lot of trauma to all of the structures in the leg and thigh, and the complexity of the surgery is something to keep in mind moving forward.
- Let’s move forward to rehabilitation following surgery for rotationplasty. During my research for this presentation, I could find no established protocols, and was unable to attain much information at all specific to rehabilitation of rotationplasty. At best, general guidelines were given, and I will present these along with my own clinical experience here at Sloan-Kettering.
- In general, the rehabilitation course looks like this. Immediately after surgery, the focus is on passive range of motion of the ankle and active range of motion in antigravity planes of the hip to maintain ankle range of motion and hip strength and range of motion. It is important to be mindful of patient positioning, especially in the hospital, and to educate them appropriately re: positioning. Like amputees, patients are prone to hip flexion and adduction contractures, and we want to avoid this as this will have an impact on gait and prosthetic use later on. If you can imagine what a patient would look like lying in bed, then you can imagine how easily they could attain these contractures. Additionally, when the patient is in the hospital, it is important to train them to perform functional activities with the appropriate assistive device, for example crutches. Be mindful that due to pain from the surgery, these patients typically progress very slowly, and will likely be reliant on a rolling walker for the necessary support during ambulation upon discharge. Therapeutic exercise progress to AROM of the ankle and toes when the patient is able. However, resisted exercise is typically held for 6 to 12 weeks post-operatively, when soft tissue healing is complete. Weight-bearing is restricted until there is evidence of healing at the osteotomy site. Adjuvant chemotherapy is started 10 to 21 days after surgery
- Some considerations to keep in mind are listed here. Full WB is contraindicated until the osteotomy site is fully healed. AROM o 0 to 30 degrees is needed to operate the prosthesis, with 0 to 50 degrees of ankle ROM being optimal. Remember that these patient are typically in a lot of pain post-surgically, and this will delay the rehabilitation process, especially early-on.
- Let’s move on to prosthetic use after rotationplasty.
- To explore prosthetic fitting after rotationplasty, I researched an article written by So and colleagues entitled, “Prosthetic Fitting After Rotationplasty of the Knee.” This article is a retrospective observational study, with 12 subjects. The median age of subjects enrolled in the study was 10 years, and there were 8 males. All patients included in the study had an oncologic pathology, with 10 patients with a diagnosis of osteosarcoma and 2 patient with a diagnosis of synovial sarcoma. Patient with osteosarcoma received chemotherapy, patients with synovial sarcoma did not receive chemotherapy.
- The first prosthesis that the authors described in the study was a preliminary bypass prosthesis. This is the first prosthesis that a patient would wear to begin gait training, and it does not allow for weight-bearing through the ankle/knee. Patients must use an assistive device to ambulate with this prosthesis. In the study, all preliminary bypass prostheses were composed of a polypropylene, ischial WB, quadrilateral sockets with total elastic auxiliary suspension, a pylon and a Seattle LightFoot. With this prosthesis, patients are instructed to plantarflex during heel strike to become familiar with the feeling of the new knee extension moment.
- Here are pictures of the preliminary bypass prosthesis.
- After the preliminary bypass prosthesis, patients are given their 1st definitive prosthesis. In the study, all definitive prostheses were made of an acrylic laminate socket with polyproylene thigh section, had anatomic suspension with either a calcaneal strap or a removable calcaneal wedge, and a Seattle LightFoot.
- Here are examples of first definitive prostheses. The authors made sure to note that the boy on the left thought that the blue camoflauge on his prosthetic leg was “cool.”
- So how long did prosthesis fitting take for the patients in the study? In the 10 patients requiring chemotherapy, those with osteosarcoma, the average time to prosthesis fitting was 230.5 days Osteosarcoma required chemotherapy, synovial sarcoma did not (7.68 months). In the 2 patients that did not require chemotherapy, those with synovial sarcoma, mean time to prosthetic fitting only took a fraction of that time, 78.5 days, or a little bit under 3 months. As the children in the study were growing, they required subsequent prostheses as they grew. The time between first and second prostheses, on average, was 18.5 months.
- Some considerations to keep in mind when fitting prostheses for patients with rotationplasty are listed on this slide. Stops can be incorporated for knee flexion and extension. This compensates for a patient’s inability to control the knee flexion moment at heel strike and is easily adjusted as the patient gains range of motion. It is important to use the longest foot that can fit in the shoe, as this longer lever arm can assist in knee stability. Subsequent prostheses may incorporate carbon fiber and multiaxial foot options. Remember to choose a prosthesis that can be easily adjusted to compensate for growth if your patient is a growing child.
- I wanted to present a great example of thinking outside of the box and being innovative in prosthetic design. In this case study, and 18 year old patient was having difficulty cycling because his prosthesis regularly caused abrasion injuries at his foot and thigh. When cycling, the thigh cuff of the prosthesis can lead to perspiration, chaffing, and skin abrasion. Because of this, he was only able to cycle for a maximum distance of 35km, or 21 miles, which is a very short distance in cycling. His goal was to climb Mont Ventoux in France, which is an iconic climb that is regularly features in the Tour de France. At 21km with an average gradient of 7.4%, it is a challenge even for the best cyclists in the world to complete.
- Here is a picture of the design that the authors of the study came up with. As you can see, it is quite unique and incorporates a very important feature of the rotationplasty, the foot immediately distal to the new knee joint.
- The authors utilized two off-the-shelf cycling shoes, with a carbon fiber shank – important in cycling especially as it allows for decreased weight – and a SACH foot. A shimano SPD pedal system was used to prevent it slipping from the pedal, this is a pedal system that allows for a cleat to clip into the pedal. The prosthesis is NOT SUITABLE FOR WALKING, but the patient could lean on the bike and walk short distance in case of emergency. The patient perceived that he could generate more power, enabling him to climb Mont Ventoux and achieve his goal.
- Now we will talk briefly about relevant outcome measures.
- The functional motor assessment consist of six categories, and it is useful when clinician wants to document the patient’s actual physical abilities. Raw scores are converted to table scores ranging from 0 to 5, maximum score 70. Pain is measured on 0-10 scale. Function is measured with two measures, the timed up-and-down 12 stairs and timed up-and-go. Supports pertains to ADs, with questions that the patient answers. Satisfaction and participation are measured with questions specific to the lower extremities. Endurance is measured with a 9-minute walk-run test.
- The musculoskeletal tumor society rating scale is also known as the Enneking score. It assesses both the UE and LE. It is clinician administered and has an inherent level of subjectivity. It also examines 6 factors, and they are listed on the slide. Two examples of items are pain (where 0 is sever pain, with continuous narcotic use, and 5 is no pain, with no medication use) and supports (where 1 is the use of one cane or crutch, using a cane or crutch most of the time, and 4 represents an intermediate category in which a brace is used occasionally). You can appreciate the level of subjectivity that can be introduced with these example items.
- The toronto extremity salvage scale is a disease-specific measure that was developed for patients undergoing limb preservation surgery for tumors of the extremities. It evaluates physical disability based on patients’ reports of their function. A patient completing this measure may complete a task and report not having difficulty performing it because they have grown accustomed to expending more energy. The measure consists of a 29-item lower extremity and 28-item upper extremity questionnaire. Items are rated on a 5-point scale from not at all difficult to impossible to do, and are additionally rated on importance on a 4-point scale from totally unimportant to extremely important.
- There is an overall paucity of research relating to rotationplasty. A search on PubMed for the procedure returns only 154 results dating back to 1962. This is less than 3 articles per year. This is not extremely surprising, as rotationplasty is not an incredibly common procedure. The overall quality of the existing research is low, with many case studies and case series, and few, if any, RCTs. There is virtually no mention of rehabilitation in the research. At best, there are a few lines giving very general guidelines, and the bulk of the research seems to be concentrated in surgical techniques and complications, quality of life, and function or persons after rotationplasty.
- The most important thing to remember about patients who have undergone a rotationplasty procedure is that they tend to be very highly functioning individuals, thanks to the creation of a new knee joint which they can actively control. Individuals also often score very highly on quality of life measures, close to or surpassing the quality of life of healthy persons.
- Here are pictures of highly functioning persons after rotationplasty. Note that the wrestler is not wearing a prosthesis.