Lecture 18 Hepatitis and liver disorders
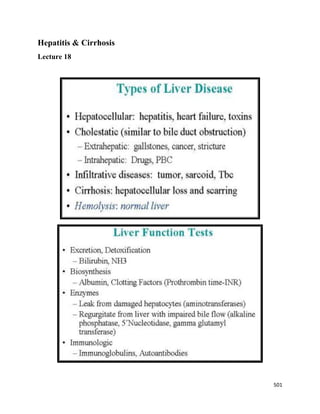
- 2. 502 Commonly Used Liver Tests Aminotransferases Aminotransferases are found in hepatocytes and are markers of liver cell injury or hepatocellular disease. Hepatocellular injury causes these enzymes to “leak” out of the liver cells, and increased levels of these enzymes are detected in the serum within a few hours after liver injury. The aminotransferases consist of alanine aminotransferase (ALT), also known as serum glutamic-pyruvic transaminase (SGPT), and aspartate aminotransferase (AST), also known as serum glutamic-oxaloacetic transaminase (SGOT). ALT is more specific for liver injury than AST. Although AST is found not only in hepatocytes but also in skeletal and cardiac muscle, markedly increased levels of muscle enzymes may be accompanied by increased levels of both AST and ALT. Alkaline Phosphatase Alkaline phosphatase is found on the hepatocyte membrane that borders the bile canaliculi (the smallest branches of the bile ducts). Because alkaline phosphatase is also found in bone and placenta, an isolated increase in the level of this enzyme should prompt further testing to determine whether the increase is from the liver or other tissues. Determination of alkaline phosphatase isoenzymes is one method of doing this. Another is the determination of γ-glutamyltransferase (GGT), an enzyme of intrahepatic biliary canaliculi that is more sensitive than alkaline phosphatase. Other than to confirm the hepatic origin of an increased level of alkaline phosphatase, GGT has little role in the diagnosis of diseases of the liver because its synthesis can be induced by many medications, thus reducing its specificity for clinically important liver disease. Bilirubin Bilirubin is a yellowish pigment found in bile (a fluid produced by the liver). 3000 mg of bilirubin is formed daily, 75% of which is from heme metabolism and 25% of which is from other proteins (ex. cytochrome P450 : contains a heme iron center). Bilirubin is the water-insoluble product of heme metabolism that is taken up by the hepatocyte and conjugated with glucuronic acid to form monoglucuronides and diglucuronides. Conjugation makes bilirubin water soluble, allowing it to be excreted in the bile.
- 3. 503 When bilirubin is measured in the serum, there are direct (conjugated) and indirect (unconjugated) fractions. Diseases characterized by overproduction of bilirubin, such as hemolysis or resorption of a hematoma, are characterized by hyperbilirubinemia that is less than 20% conjugated. Hepatocyte dysfunction or impaired bile flow produces hyperbilirubinemia that is usually more than 50% conjugated. Because conjugated bilirubin is water soluble and may be excreted in the urine, patients with liver disease and hyperbilirubinemia have dark urine. In these patients, the stools have a lighter color because of the absence of bilirubin pigments. Bilirubin Metabolism
- 4. 504 Prothrombin Time and Albumin Prothrombin time (PT) and serum level of albumin are markers of liver synthetic function. Abnormalities of PT and albumin imply severe liver disease and should prompt an immediate evaluation. PT is a measure of the activity of factors II, V, VII, and X, all of which are synthesized in the liver. Because these factors are also dependent on vitamin K for synthesis, deficiencies of vitamin K also produce abnormalities of PT. Vitamin K deficiency can result from the use of antibiotics during a period of prolonged fasting, small-bowel mucosal disorders such as celiac disease, and severe cholestasis, with an inability to absorb fat-soluble vitamins. True hepatocellular dysfunction is characterized by an inability to synthesize clotting factors even when stores of vitamin K are adequate. However, the serum level of albumin can decrease relatively quickly in a severe systemic illness such as bacteremia. This rapid decrease most likely results from the release of cytokines and the accelerated metabolism of albumin. A chronic decrease of albumin in a patient without overt liver disease should prompt a search for albumin in the urine. Bilirubin Normal ranges are: total bilirubin < 1.4 mg/dl direct bilirubin < 0.4 mg/dl urine bilirubin undetectable urine urobilinogen undetectable Pathophysiology of Jaundice The circulating concentration of bilirubin may become elevated as a consequence of increased rate of hemolysis, and/or deficient hepatic uptake, conjugation, or secretion biliary obstruction
- 5. 505 Acute Hepatitis Acute hepatitis is an inflammatory process causing liver cell death either by necrosis or by triggering apoptosis. Acute hepatitis is most commonly caused by infection with one of several types of viruses→ hepatitis A, hepatitis B, hepatitis C, hepatitis D, hepatitis E, hepatitis G. all produce clinically similar illnesses. Acute hepatitis is also sometimes caused by exposure to drugs (eg, isoniazid) or poisons (eg, ethanol). Hepatitis A & E having no chances of chronicity & liver cancer while hepatitis B,C & D having chances of chronicity & liver cancer. Viral Hepatitis Sign & symptoms of hepatitis Dark urine Prodrome o Flulike, anorexia, weakness, headache. Abdominal discomfort & Right upper abdominal pain
- 6. 506 Jaundice, Fever , Nausea, Anorexia, Diaharrea, Fatigue Hepatomegaly Elevated level of bilirubin Overt disease o Anorexia, weakness, nausea, ALT (SGPT), AST (SGOT) elevated 500 to several thousand units without marked increase in alkaline phosphatase. Bilirubin levels are variable. Hepatitis a virus (HAV) Hepatitis A virus is a RNA virus (enterovirus, picorna group, 25-28 nm particle) which is found primarily in feces and causes a transient viremia. The transmission is fecal/oral (rarely blood borne infection). HAV is common in children and young adults especially in areas of poor sanitary conditions. Epidemics can occur in situations of water contamination. There is a short incubation before the acute onset of symptoms (unless subclinical). This disease has a very good prognosis with mortality <1%.Most patients recover fully in several weeks. There Is No Chronic Disease Or Carrier State. The serological tests show a rising titer of anti-HAV (IgM or IgG). Approximately 40% of U.S. population and 80% in 3rd world countries have antibodies, most from subclinical infections. Prophylaxis can be achieved by giving immune serum globulin which prevents or modifies infection. Hepatitis A Vaccination A single 0.02-mL/kg dose of Ig is adequate for short trips (less than 3 months), but 0.06 mL/kg dose for every 5 months is necessary for longer visits.
- 7. 507 Hepatitis B Structure Hepatitis B virus is a DNA virus; a DANE particle (42 nm) composed of o an inner core and o lipoprotein envelope. It is found in greatest concentration in liver and less in blood. The nucleocapsid encloses the viral DNA and a DNA polymerase that has reverse transcriptase activity. A polymerase is an enzyme that synthesizes long chains or polymers of nucleic acids. DNA polymerase and RNA polymerase are used to assemble DNA and RNA molecules, respectively, by copying a DNA or RNA template strand using base-pairing interactions. In addition to the Dane particles, filamentous and spherical bodies lacking a core can be found in the serum of infected individuals. These particles are not infectious and are composed of the lipid and protein that forms part of the surface of the virion, which is called the surface antigens (HBsAg), and is produced in excess during the life cycle of the virus.
- 8. 508 Hepatitis B Transmission Transmission occurs via the inoculation of blood, blood products or other body fluids ( i.e., semen). High risk groups include medical personnel, male homosexuals, and dialysis patients. The disease symptoms follow a long incubation period and presents with an insidious onset. The symptoms last from 2-12 weeks although subclinical infections can occur. 10% of the cases go on to a chronic state. In addition, 0.1-1% of the U.S. population are asymptomatic carriers of HBV and 8-10% are AB positive. Hepatitis B Prophylaxis Prophylaxis consists of hyperimmune serum globulin in acutely exposed individuals or a vaccine for those at high risk. The vaccine, Hepatavax, is prepared from HBsAg+ blood from which many donors are homosexuals. HBV has a strong epidemiological association with Hepatocellular Carcinoma. Hepatitis B Serology HBsAg: Appears several weeks post exposure and disappears at 3 months if the patient recovers. If present beyond 6 months the patient is considered a carrier. ANTI-HBsAg: Appears at 3 months and confers immunity. HBeAg: Appears after HBsAg and disappears before it. It is associated with infectivity (blood HBeAg+ is 10 X more infective than HBsAg+). As with HBsAg persistence, its prolonged presence implies chronicity. ANTI-HBe (antibody to HBeAg ), begins to appear in the serum at about the time that HBeAg disappears, its appearance signals the onset of Resolution of the Acute Illness. HBcAg: Concentration too small to measure. Anti-HBcAg: IMPORTANT MARKER OF HBV INFECTION DURING THE “WINDOW PERIOD”, i.e. when HBsAg is absent and no anti-HBsAg antibody is yet detectable. High titers of Anti-HBcAg without HBsAg implies chronic illness. Diagnosis of HBV HBs Ag: used as a general marker of infection. HBs Ab: used to document recovery and/or immunity to HBV infection. anti-HBc IgM : marker of acute infection. anti-HBcIgG: past or chronic infection.
- 9. 509 HBeAg : indicates active replication of virus and therefore infectiveness. Anti-Hbe: virus no longer replicating. However, the patient can still be positive for HBsAg which is made by integrated HBV HBV-DNA: indicates active replication of virus, more accurate than HBeAg especially in cases of escape mutants. Used mainly for monitoring response to therapy Hepatitis C virus or Non-A/Non-B Hepatitis (NANB) The causative agent is RNA virus. 90% of post-transfusion hepatitis cases are due to NANB. HBV is less common since blood screening is able to detect contaminated blood. NANB is responsible for about 20-30% of sporadic cases of hepatitis. Endemic and epidemic NANB can occur. Symptoms follow a long incubation period (2-26 wk) and present with an insidious onset. Most cases are without jaundice (anicteric). There is a strong predilection for chronicity and a carrier state does exist. Hepatitis C is the most common cause of Chronic Hepatitis, Cirrhosis & Hepatocellular Cancer in the world The transmission is similar to HBV and fecal-oral spread has not been documented.
- 10. 510 Hepatitis C virus Diagnosis Diagnosis by detection of: o Hepatitis C antibody (Anti-HCV). o Alanine aminotransferase ↑ (ALT)=(SGPT) o Hepatitis C RNA (HCV RNA) or Polymerase Chain Reaction (PCR) The presence of anti-HCV antibodies in a person with a risk factor or evidence of liver disease strongly suggests the diagnosis of chronic hepatitis C. The absence of anti-HCV antibodies generally rules out the diagnosis. Tests for HCV RNA in blood should be done in those individuals with anti-HCV antibodies to confirm the diagnosis and in the rare patient who does not have anti-HCV antibodies but in whom the diagnosis is still strongly suspected on clinical grounds. Unlike hepatitis A & B, antibody to HCV is not protective, but they serve as Markers for the disease. Acute NANB classically produces a pattern of fluctuating enzyme elevation, i.e., remissions and exacerbations (While all forms of hepatitis show an increase in SGPT (ALT) and SGOT) Hepatitis C Prophylaxis Prophylaxis consists of SGPT (ALT) screening of donor. SGPT elevations are found in 1.5-3% of donor pop. 50% of patients with isolated SGPT elevations probably have NANB. At present, there is no Vaccine that protects against HCV infection. Hepatitis D virus or Delta Agent Delta is an RNA virus encapsulated in a coat of hepatitis B surface antigen. An ongoing infection of HBV is required before Delta agent is capable of replication. It is found only in blood which is HBsAg+. HBV infection and HBsAg synthesis are necessary for Delta replication and expression. Delta can coinfect with HBV, or superinfect HBV carrier. The host ability to clear HBV determines the duration of Delta infection. It is HBV infection, not HBV replication that provides environment conducive to Delta. The majority of patients with chronic Delta infection have circulating anti-HBe. The transmission similar to HBV found in chronic carriers or in persons infected simultaneously with HBsAg and Delta.
- 11. 511 Prognosis of Hepatitis D Extremely poor. The antigen may be detectable in the serum for a few days while total anti-delta antibody is a long-lasting antibody produced in response to a Delta infection. Therefore anti-Delta antibody is an excellent marker of Recent or Past infection. Delta agent produces severe disease and has an increased prevalence in IV drug addicts and hemophiliacs predominantly in Italy, southern Europe, and The Middle East. Serum Delta Markers DELTA Antigen o Detectable early and transiently in acute infection. Appears after HBsAg in simultaneous infection. Undetectable in chronic infection• ANTI-DELTA Antibody o Appearance follows disappearance of antigen. o Early antibody is IgM, often persists in chronic infection. o IgG anti-Delta often low-titered or undetectable in resolving HBV/delta infection. o High-titered IgG persists in chronic delta infection
- 12. 512 Chronic Hepatitis Chronic hepatitis is a category of disorders characterized by the combination of liver cell necrosis and inflammation of varying severity persisting for more than 6 months. It may be due to viral infection( About 5% of infections become chronic), drugs and toxins, genetic and metabolic factors, or unknown causes. The severity ranges from an asymptomatic stable illness characterized only by laboratory test abnormalities to a severe, gradually progressive illness culminating in cirrhosis, liver failure, and death. Based on clinical, laboratory, and biopsy findings, chronic hepatitis is often divided into two classes: chronic persistent chronic active hepatitis. Chronic Persistent Hepatitis (CPH), (1/3) A relapsing, remitting condition which may be associated with mild symptoms of fatigue and anorexia or may be asymptomatic. CPH does NOT progress to cirrhosis; The clinical course is relatively benign, often characterized by spontaneous resolution (eg, clearance of persistent viral infection) Typically there is elevation of one of the aminotranaminases (“transaminitis”) and HBsAg persists in about 1/3 of cases. Liver biopsy shows only “triaditis”, i.e., increased lymphocytes, plasma cells and macrophage with only a few eosinophils and neutrophils in the portal areas. Importantly, there is not significant hepatocyte necrosis, crossing of the limiting plate nor bridging or piecemeal necrosis. “Ground Glass” hepatocytes may be seen in HBsAg + cases, and are a marker for the carrier state; these cells stain positively with monoclonal antibodies for HBsAg. However, not all carriers have chronic hepatitis, i.e., there are “healthy carriers as well and their liver biopsies show only occasional groups of “Ground Glass” hepatocytes. Carrier status is most often seen in individuals who acquired the infection at an early age (especially during childbirth) or who have impaired immunity. Carriers are HBsAg+, which is why all blood donors are screened for HBsAg+. a flat hazy and uniformly dull appearing cytoplasm on light microscopy. The cytoplasm's granular homogeneous eosinophilic staining is caused by the presence of HBsAg.
- 13. 513 Chronic Active Hepatitis (CAH) (2/3’s) A chronic disorder associated with hepatocellular necrosis and fibrosis. It may result from HBV, HBV/HDV, HCV Virus, and other causes, including Chronic Autoimmune Hepatitis (Lupoid Hepatitis). It is a serious progressive disorder - usually progressing to Cirrhosis. o CAH is apt to be symptomatic and most cases show: elevation of transaminases with elevated globulin levels and persistence of HBsAg. Liver biopsy shows “triaditis” (with a predominance of lymphocytes) BUT unlike CPH, there is erosion of the limiting plate with extension of the inflammatory process into the surrounding hepatic lobules. This is called “piecemeal” necrosis. There is also “bridging” necrosis which involves the coalescence of areas of destroyed hepatocytes to create tracts where all the hepatocytes are missing and only the reticulin remains. Both piecemeal and bridging necrosis are associated with fibrosis—eventually leading to cirrhosis. Chronic Hepatitis Clinical Presentation Patients may present with fatigue, malaise, low-grade fever, anorexia, weight loss, mild intermittent jaundice, and mild hepatosplenomegaly.
- 14. 514 Others are initially asymptomatic and present late in the course of the disease with complications of cirrhosis, including variceal bleeding, coagulopathy, encephalopathy, jaundice, and ascites. In contrast to chronic persistent hepatitis, some patients with chronic active hepatitis- particularly those without serologic evidence of antecedent HBV infection-present with extrahepatic symptoms such as skin rash, diarrhea, arthritis, or various autoimmune disorders such as: Thyroiditis, hypothyroidism, Autoimmune hemolytic anemia, Polyarthrit Ulcerative colitis, Uveitis. Chronic persistent Vs chronic active hepatitis Fulminant Hepatic Failure Fulminant hepatic failure is defined as hepatic failure with encephalopathy developing less than 8 weeks after the onset of jaundice in patients with no history of liver disease. Poor prognostic markers include a drug-induced cause (other than acetaminophen), older age, grade 3 or 4 encephalopathy, acidosis, and international normalized ratio (INR) greater than 3.5. Treatment is supportive, and patients should be transferred to a medical center where liver transplantation is available.
- 15. 515 Common Causes of Fulminant Hepatic Failure Liver Anatomy Liver is the largest gland of the body. Under the diaphragm, within the rib cage in the upper right quadrant of the abdomen It is about 5% of body weight in the healthy neonate. The liver is about 2% of body weight in the adult. It weighs around 1400g in an adult female and about 1800g in the male. the liver is divided into right and left lobes by the external marking of the falciform ligament. The falciform ligament attaches the liver to the abdominal wall and diaphragm. It receives about 1.425 liter of blood every minute via the hepatic artery and portal vein.
- 16. 516 Hepatic lobule The internal structure of the liver is made of around 100,000 small hexagonal functional units known as lobules. Hepatic lobules consist of : 1) Central vein 2) Radiating hepatic cord cells 3) Portal triad (Hepatic artery, Portal vein and Bile duct) Structure of liver lobule The liver lobule is the basic hepatic unit consisting of the : Centrally located is the central vein with columns of hepatic cells arranged in radials separated by adjacent sinusoids. The liver differ from other capillaries in the body, because of the presence of open pores or fenestrae.
- 17. 517 These sinusoids are made up of fenestrated endothelium and Kupffer cells. Kupffer cells act as macrophages and destruct the old rbc’s thus form a reticuloendothelial system. At each of the six corners of a lobule is a portal triad. Blood from these vessels perfuse the sinusoids .Sinusoidal blood drains into hepatic veins through which blood leaves the liver, draining into the vena cava and the right heart. Hepatocytes produce bile. Bile flows through canals called bile canaliculi to a bile duct. Bile ducts leave the liver via the common hepatic duct Hepatocytes have a unique capacity to reproduce in response to liver injury. Liver regeneration can occur after surgical removal of a portion of the liver or after injuries that destroy parts of the liver. Kupffer cells & Stellate cells Kupffer cells (KC) constitute 80-90% of the tissue macrophages present in the body. They reside within the lumen of the liver sinusoids, and are therefore constantly exposed to gut-derived bacteria, microbial debris and bacterial endotoxins, known to activate macrophages. Hepatic stellate cells (vitamin A-storing cells, lipocytes, Ito cells) exist in the space between parenchymal cells and sinusoidal endothelial cells of the hepatic lobule and store 80% of retinoids in lipid droplets in the cytoplasm. Retinoids have many important functions including roles in vision, regulation of cell proliferation and differentiation, growth of bone tissue, immune function, and activation of tumor suppressor genes.
- 18. 518 Liver Diseases Definitions Ascites refers to abnormal accumulation of transudate in the peritoneal cavity. Bile acids are detergents synthesized from cholesterol in the liver. Cholic acid and cheno- deoxy-cholic acids are conjugated with glycine and taurine, whereby they become water- soluble. Cholelithiasis or gallstone disease is defined as a condition with gallstones within the lumen of the gallbladder, whether symptoms occur or not. Transudate: is an extravascular fluid with low protein content and a low specific gravity (< 1.012). Exudate: is an extracellular fluid of high protein content, with cell debris present and high specific gravity (>1.020). Liver Diseases Definitions 2 Cirrhosis refers to destruction of the normal hepatic lobular structure by fibrous septa, necrotic hepatocytes and regenerative nodules of hepatocytes. Cholestasis refers to intra- or extra-hepatic obstruction of the bile flow. Biliary cirrhosis is a progressive cholestasis with cirrhosis caused by destruction of bile ducts and bile ductules. Antibodies to mitochondria are found in the blood and the etiology probably includes immunological phenomena. Hepatitis is either infectious or toxic. Virus, bacteria or protozoa cause infectious hepatitis. Liver toxins, haemolytic toxins, metabolic toxins and drugs cause toxic hepatitis. Icterus refers to yellow coloration of skin, blood plasma, mucous membranes and tissues. The threshold for visible jaundice (icterus) is a Bilirubin in blood plasma above 1.8 mg/dl or 30 mM in most people. Liver functions The liver is a metabolically active organ responsible for many vital life functions. The primary functions of the liver are: Bile production and excretion Excretion of bilirubin, cholesterol, hormones, and drugs Metabolism of fats, proteins, and carbohydrates Enzyme activation Storage of glycogen, vitamins, and minerals Synthesis of plasma proteins, such as albumin, and clotting factors Blood detoxification and purification
- 19. 519 Most of the clinical consequences of liver disease may be due to: • A failure of one of the liver's functions or • A consequence of portal hypertension; the altered hepatic blood flow of cirrhosis. Liver Cirrhosis Definition: It is a chronic liver disease results from necrosis of hepatocytes followed by fibrous tissue deposition and formation of regenerating nodules. The liver architecture is diffusely abnormal and this interferes with liver blood flow and function. This disturbance produces the clinical features of portal hypertension and impaired liver cell function. Causes of Liver cirrhosis Alcohol is now the most common cause in the West, but viral infection is the most common cause world-wide. Young patients with cirrhosis must be investigated carefully as the cause may be treatable (e.g. Wilson’s disease: rare inherited disorder that causes copper to accumulate in the liver, brain and other vital organs).
- 20. 520 Cirrhosis Pathophysiology Long standing injury to the liver lead to inflammation, necrosis and eventually fibrosis (initiated by activation of stellate cells). These liver injuries e.g. (virus, alcohol, .... ) stimulate kupffer cells→ release of cytokines → stimulate into (stellate) cells → excessive release and deposition of collagen fibers → Destruction of hepatocytes, bile duct cells, vascular endothelial cells (loss of hepatic architecture “cirrhosis”). Repair thru cellular proliferation and regeneration
- 21. 521 Clinical Manifestations of cirrhosis
- 22. 522 Complications and Effects of Cirrhosis Portal hypertension. Ascites Splenomegaly Esophageal varices Infections (bacterial peritonitis) Malnutrition Hepatic encephalopathy Jaundice Bone disease (greater risk of fractures). Gallstones and bile duct stones. Blocked flow of bile can lead to irritation, infection and the creation of stones. Increased risk of liver cancer (Primary hepatocellular carcinoma) Acute-on-chronic cirrhosis (multiorgan failure) Natural history of cirrhosis Any chronic liver disease will lead to cirrhosis. Initially, cirrhosis will be compensated (median survival, 9 years), but once complications (ascites, variceal hemorrhage, encephalopathy, jaundice) develop, it becomes decompensated (median survival, 1.6 years). Hepatocellular carcinoma (HCC) can develop at any stage and precipitate decompensation and death.
- 23. 523 Portal Vein Measuring approximately 8 cm in length & contains no valves. the hepatic portal vein is located in the right upper quadrant of the abdomen, originating behind the neck of the pancreas. In most individuals, the hepatic portal vein is formed by the union of the superior mesenteric vein and the splenic vein. Sometimes the hepatic portal vein also directly communicates with the inferior mesenteric vein. Immediately before reaching the liver, the portal vein divides into right and left. It ramifies further, forming smaller venous branches and ultimately portal venules. Each portal venule courses alongside a hepatic arteriole and the two vessels form the vascular components of the portal triad. These vessels ultimately empty into the hepatic sinusoids to supply blood to the liver. Anatomy of Portal System The splanchnic circulation is composed of gastric, small intestinal, colonic, pancreatic, hepatic, and splenic circulations, arranged in parallel with one another. Anatomy of Portal System The splanchnic circulation is composed of gastric, small intestinal, colonic, pancreatic, hepatic, and splenic circulations, arranged in parallel with one another. The portal vein supplies 70% of the blood flow to the liver, but only 40% of the liver oxygen supply. The remainder of the blood comes from the hepatic artery (30%of blood supply), and blood from both of these vessels mixes in the sinusoids.
- 24. 524 Portal hypertension (PH) The portal vein is formed by the union of the superior mesenteric and splenic veins. Normal portal pressure is 5 to 10 mm Hg (7 to 14 cm H2O), which exceeds inferior vena caval pressure by 4 to 5 mm Hg (portal venous gradient). PH is defined as an increase in the pressure gradient between the portal vein and hepatic veins or the inferior vena cava (IVC) (Central vein of the liver lobule→ Hepatic vein→ IVC→ Rt. Atrium ) Portal hypertension can be classified according to the site of obstruction: Prehepatic – due to blockage of the portal vein before the liver Intrahepatic – due to distortion of the liver architecture, which can be presinusoidal (e.g. in schistosomiasis) or postsinusoidal (e.g. in cirrhosis) o Schistosomiasis (bilharzia) caused by parasitic worms of the Schistosoma type. Transmission through contaminated freshwater sources with excreta containing parasite eggs. It may infect the urinary tract or intestines causing abdominal pain, diarrhea, bloody stool, or blood in the urine. In those who have been infected a long time, liver damage, kidney failure, infertility, or bladder cancer may occur. In children it may cause poor growth and learning difficulty. Posthepatic – due to venous blockage outside the liver (rare).
- 25. 525 Portal hypertension: Definition Portal pressure gradient > 5mmHg o resulting from obstruction of portal blood draining from the splanchnic circulation back to the systemic circulation Portal pressure gradient (PPG) = Portal vein pressure – central venous pressure PPG portal perfusion pressure of the liver PPG > 10mmHg => ascites PPG > 12mmHg => variceal bleeding Portal Hypertension Causes Cirrhosis is the most common intrahepatic cause of portal hypertension
- 26. 526 Portal-systemic collateral pathways The PORTAL system of veins drain the venous blood from the intestine and the spleen to the liver via the portal vein. The SYSTEMIC system of venous drainage collects blood from the rest of the body to the right atrium of the heart. There are sites in the body where the two systems join (anastomosis) Distal esophagus: left gastric (coronary) vein & short gastric veins to distal esophageal veins Splenorenal (lienorenal) ligament: splenic vein to left renal vein - splenorenal shunt Retroperitoneum: superior mesenteric veins to retroperitoneal/lumbar veins to the inferior vena cava Anterior abdominal wall: paraumbilical vein to subcutaneous periumbilical veins (caput Medusae) Anal canal: superior rectal vein (from inferior mesenteric vein) to upper anal canal veins (haemorrhoids)
- 27. 527 Portal Hypertension Pathophysiology As portal pressure rises above 10–12 mmHg (portal hypertension), shunting of blood away from the liver into the systemic venous system provides a mechanism of reducing portal venous pressure. Spontaneous portal-systemic collateral pathways (also called varices) develop via enlargement of pre-existing anastomoses between the portal and systemic venous system. However these are not sufficient to normalize portal venous pressure. The Porto-systemic collaterals: o In normal conditions collapsed. o In portal hypertension engorged divert blood away from the portal circulation. Portal Hypertension Consequences The consequences of this portal-to-systemic shunting are o Loss of the protective and clearance functions of the liver; o Loss of functional abnormalities in renal salt and water homeostasis; o and a greatly increased risk of gastrointestinal hemorrhage from the development of engorged blood vessels carrying venous blood bypassing the liver (eg, esophageal varices). Even in the absence of any intrinsic parenchymal liver disease, portal to-systemic shunting of blood can produce or contribute to : o Encephalopathy (altered mental status due to failure to clear poisons absorbed from the gastrointestinal tract); o Gastrointestinal bleeding (due to esophageal varices); and Malabsorption of fats and fat-soluble vitamins (due to loss of enterohepatic recirculation of bile), with associated Coagulopathy.
- 28. 528 Treatment of cirrhosis Nutritional and vitamin supplementation. A reduced-protein diet is useful to decrease ammonia production. Diuretics to relieve fluid accumulation. Intubation or shunting to relieve bleeding from accessory blood vessels. Management of symptoms of liver failure. Liver transplantation :is the only effective treatment for end-stage liver disease. Liver cancer Tumors originating in the liver are rare but tend to be malignant when they arise and are usually symptomatic. More commonly, tumors arise outside of the liver and spread to it as a result of metastasis. Because of its rich blood supply, the liver provides an excellent site for growth of metastatic tumors. Lung, breast, colon and pancreatic tumors are the most common source of metastatic tumors to the liver. The clinical manifestations of liver cancer or metastasis will depend primarily on the rate of tumor growth. As more functional liver tissue becomes involved, the clinical manifestations tend to become more severe. Growing tumors may impair liver blood flow and bile outflow, leading to hepatomegaly and jaundice. Cachexia or lean tissue wasting tends to be severe with liver cancer or metastasis. Long term prognosis is poor. ___________________
