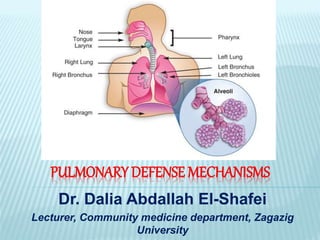
Pulmonary defense mechanisms
- 1. PULMONARY DEFENSE MECHANISMS Dr. Dalia Abdallah El-Shafei Lecturer, Community medicine department, Zagazig University
- 2. PARTICLES
- 3. Inhalable particles are small droplets or solids - organic or inorganic, viable or nonviable- that can become airborne and penetrate into the oral or nasal airways.
- 4. FACTORS AFFECTING PARTICLES’ EFFECTS: Diameter Shape Density Composition Concentration Dimensions of Air passages Pattern of air flow
- 5. DIAMETER Spherical particles: Mass median diameter (depend on physical diameter & density) Non-spherical particles: Aerodynamic diameter (depend on aerodynamic drag)
- 6. A particle falling through the air under the force of gravity (gravitational sedimentation) accelerates until it reaches a velocity at which the force of gravity is just balanced by the viscous resistive force exerted by the air (Stokes' law). This velocity is known as the terminal settling velocity. Thus, the aerodynamic diameter of a particle, however shaped, is taken as the diameter of a unit density sphere that would have the identical terminal settling (Stokes) velocity. AERODYNAMIC DIAMETER
- 7. AEROSOL SIZE DEFINITION Inhalable • >100µm Thoracic • >10µm Respirable • >5µm
- 8. EPA PARTICULATE MATTER (PM) Total PM TPM (Supercoarse) >10µm Coarse PM PM10 2.5-10µm Fine PM PM2.5 •1-2.5µm Ultrafine PM <1µm
- 10. SHAPE Fibrous (length : diameter) = (3:1)
- 11. PATTERN OF AIR FLOW Slow deep breathing: ↑ sedimentation in all RT. Rapid shallow breathing: ↑ impaction in LAWs (mainly in “hot spot” around bifurcation angle) & sedimentation in SAWs.
- 14. Perfect Lung Mechanisms of deposition of aerosol
- 16. IMPACTION Particles with sufficient mass will strike with resp.epith.surface at points of branching and curvature “Hot spots” As direction of air velocity change, particles’ inertial force will prevent them from changing directions at rate as that of air flow. The greater the mass, the less ability of particles to change direction with air flow.
- 17. SEDIMENTATION Particles which are of sufficiently small size to escape deposition by inertia, may deposit on resp.epith. Through sedimentation when velocity of air flow become slow. Gravity is the predominant force. Sedimentation rate α particle density. Sedimentation rate α (particle diameter)²
- 18. DIFFUSION For extremely small particles “Brownian motion” in which suspended particles bombarded by surrounding gaseous molecules. Rate of diffusion inversely proportionate to particle diameter.
- 20. Upper airway filter Lower airway filter Macrophage clearance to airways Macrophage clearance via lymphatics
- 23. UPPER AIRWAY FILTER Hairs & mucosal folds over turbinate direct airflow through nose so most particles > 15 µm diameter, hit surface and carried in mucus to pharynx then swallowed. If particles are irritant or allergic→ running eyes &nose + sneezing. At work a certain tolerance may develop. Heavy work or nasal obstruction → mouth breath → bypass UAW filter
- 24. LOWER AIRWAY FILTER Mucociliary epithelial lining (goblet cells, submucosal seromucus glands) act as a low resistance filter, which remove nearly all particles down to 5 µm. Particles carried in the mucus (viscoelastic) back to larynx, joining particles from UAW. 200 cilia per cell, each beat 1000 times/min in a wave-like pattern.
- 27. Goblet Cell
- 28. Ciliary action
- 29. Cilia just touching the gel layer
- 30. Gel layer of the mucus above the sol layer
- 31. Irritants → + nerve endings → Cough + Airway narrowing + Outpouring of secretions. → prolonged exposure → goblet cell proliferation + submucosal gland hypertrophy → Chronic bronchitis.
- 32. Normal airway (above); Enlarged mucous glands (below)
- 33. IMPAIRMENT OF NORMAL MUCOCILIARY FUNCTION Mucus: too much, or change in composition, e.g. chronic bronchitis, cystic fibrosis, asthma Cilia: paralysis by toxic gases bronchial epithelium destroyed congenital defect of ciliary motion
- 34. MACROPHAGE CLEARANCE TO AIRWAYS Particles getting beyond mucociliary clearance called “Respirable or Alveolar dust” Very small particles (<0.5 µm) sediment so slowly → + type II cells → surfactant → coat particles. Macrophages move out from wall →engulf coated particles → some moving back in when fully loaded →many of dust particles dissolve by lysosomal enzymes → when they are fully laden with insoluble material →migrate through interstitium to centers of lobules →enter mucus- lined airways →carried by mucus to larynx with rest of dust.
- 35. By this mechanisms, lungs can clear most retained dusts as results of regular exposure at work up to 4mg/m³ of respirable particles provided that macrophages not damaged. Above this level →system become overloaded →dust accumulate in lung
- 36. IMPAIRMENT OF NORMAL MACROPHAGE FUNCTION Inhaled gases (ozone, cigarette smoke) Toxic particles (silica) Alveolar hypoxia Radiation Corticosteroids Alcohol ingestion
- 38. Alveolar macrophage in the corner of an alveolus
- 39. MACROPHAGE CLEARANCE VIA LYMPHATICS Failure of dust clearance usually a result of combination of dust (overload + property) → damage macrophages → cell die → dust picked up by other macrophages which attempt to carry it to Hilar LNs via lymphatics (inter lobular septa & under pleura) Dust can get struck along either route or in hilar LNs Some carried on into blood stream to spleen, BM, or kupffer cells in liver, and so accumulate in body.
- 40. Clearance of deposited particles
- 41. LUNG IMMUNE DEFENSES AGAINST ENVIRONMENTAL AGENTS
- 42. PATHOGENS Pathogens enter the airways from two major sources: Inhalation of bioaerosols in the environment Aspiration of nasopharyngeal secretions.
- 45. ANTIMICROBIAL COMPONENTS Two of the most abundant antimicrobial proteins of airway secretions are: Lysozyme & Lactoferrin (0.1 - 1 mg/ml). Secretory leukoprotease inhibitor (SLPI) surfactant
- 46. Lysozyme: - Enzymatic lysis of bacterial cell walls, can also kill bacteria non-enzymatically. - Highly active against many Gram +ve species but is relatively ineffective against Gram -ve bacteria. - Produced by both epithelial cells & leukocytes. - It is about 10-fold more abundant in the initial "airway" aliquot than in later samples of BAL.
- 47. Lactoferrin: - Iron-binding protein highly abundant in the specific granules of human neutrophils & epithelial secretions. - Inhibits microbial respiration & growth, by sequestering essential iron. - Can also be directly microbicidal.
- 48. Secretory leukoprotease inhibitor (SLPI) - Antimicrobial activity against in vitro Gram - ve & +ve bacteria.
- 49. Surfactant - At the alveolar level, there are 2 components of the surfactant layer: Surfactant proteins A & D. - Bind to microorganisms & enhance adhesion & phagocytosis of microorganisms by agglutination & opsonization. - Also directly antimicrobial.
- 52. ANTIBODIES AND COMPLEMENT Potent immune system molecules present in airway & alveolar lining fluid. Mainly immunoglobulin A (IgA) & G (IgG). IgA “UAW” is predominantly found along the nasopharyngeal mucosa & in large airway; its relative concentration decreases progressively from larger to smaller airways. IgG “LAW” is the major antibody found in alveolar fluid.
- 53. ANTIOXIDANTS The first line of defense against inhaled oxidant gases (& particles) “O3 & NO2”, normally present in lung lining fluid. Glutathione & Ascorbate, Uric acid, & α- tocopherol. Achieving toxicity through intermediates formed when antioxidant defenses are overwhelmed.
- 55. SURVEILLANCE BY CELLULAR FIRST RESPONDERS Macrophages Include subsets in distinct anatomic compartments (Alveolar, interstitial, & airway macrophages). The most numerous & well studied is alveolar macrophage (AM). Normal adult lungs contain about 20*109 Ams (BAL routinely yields 10 to 20*106 ). AMs are ultimately derived from BM hematopoiesis. Injury → influx & differentiation of blood monocytes → Increases in macrophage number. Life span of AMs in normal individuals range from one to several months.
- 56. The main function of the AM is phagocytosis & clearance of inhaled material. The AMs can ingest, but fail to kill, certain microorganisms, as (Mycobacterium, Nocardia & Legionella) which are then capable of replicating intracellularly. Ultimate eradication of these pathogens requires the development of CMI.
- 57. The process of phagocytosis: 1- Recognition or binding of phagocytic targets. - AMs possess a broad array of membrane receptors that mediate binding of organisms and particles. - Phagocytosis is initiated by these specific receptors that either recognize serum components (opsonins) (opsonin-dependent) or directly recognize molecular determinants on the target(opsonin-independent).
- 58. 2- Internalization & killing: AM has considerable microbicidal machinery. Generates Reactive Oxygen Species (ROS) (using the "respiratory burst") that contribute to pathogen killing. Reactive Nitrogen Intermediates (RNI) can also contribute to pathogen killing.
- 59. 3- Movement of AMs to the Mucociliary escalator: After ingestion of particles, AM functions ultimately to remove offending material from lung. Movement of AMs to the mucociliary escalator & clearance to the oropharynx. Entry of macrophages into tissue compartments, lymphatics & migration to thoracic lymph nodes.
- 60. 4- Release of inflammatory mediators Include lipid mediators (e.g., LTB4) & chemokines (interleukin-8). AM recruit additional help {polymorphonuclear neutrophils (PMNs)}.
- 62. Ciliated Epithelial Cells Integral part of the mucociliary clearance system. Produce important components of the lining fluid in airway & alveolus {Mucus, Surfactant, Complement, Lysozyme}. Some direct antibacterial function. Secrete a large array of cytokines & other molecules (e.g., IL-1, -5, -6, -8, GM-CSF) which chemoattract & activate cells of the innate & adaptive immune system, which, in turn, immobilize and kill microorganisms.
- 63. Polymorphonuclear Neutrophils - The major 2nd cellular defense. - Up to 40% of blood PMNs are marginated or in transit through the lung, facilitating recruitment when needed. - Rapid & large movement of PMNs into the alveoli is achieved by influence of several chemotactic factors released by AMs & other lung cells (e.g., IL-8, leukotrienes, complement fragments). - Killing of ingested microorganisms by generation of NADPH oxidase-dependent ROS (e.g., superoxide, hydrogen peroxide) & by phagolysosomal fusion.
- 64. Mast Cells In intraepithelial locations or around blood vessels & bronchioles. Produce Tumor Necrosis Factor (TNF) & a wide range of cytokines & chemokines & important lipid mediators, such as LTC4 and LTB4.
- 65. Natural Killer Cells (NK) Arise from same hematopoietic lineage as T cells, (But not mature in thymus & not express re-arranged antigen receptors). Important in initial defenses against viral infection of lungs. Local release of IL-12 & IL-15 by dendritic cells & macrophages contributes to stimulation of NK cells. Recognize virus-infected (& neoplastic) cells because of their altered expression of leukocyte antigen (HLA) class I tissue antigens. Release Interferon-γ (IFN- γ), which, in turn, leads to recruitment of other immune cells.
- 67. Dendritic Cells (DCs) Characteristic long, branched processes. In airways, alveolar parenchyma, and thoracic lymph nodes. Specialized mononuclear phagocytes with important functions in antigen presentation & initiation of adaptive immune responses.
- 68. Acting as sentinels in airways, they sample incoming pathogens and antigens through by phagocytosis. When this is accompanied by a second, "danger" signal, they undergo a phenotypic & functional change from their basal immature state. This maturation promotes the processing of antigen and its presentation on the cell surface and the migration of the dendritic cell to T-cell rich areas of nearby lymph nodes. Here they can initiate or amplify adaptive immune responses by triggering proliferation and activation of antigen-specific T lymphocytes.
- 70. CYTOKINES Critical for successful orchestration of defense mechanisms against environmental agents & are also mediators of untoward outcomes such as acute injury & chronic inflammation & fibrosis. TNF & chemokines which function in both acute and chronic phases of these processes.
- 71. Tumor Necrosis Factor TNF- αis a protein. Monocytes express at least 5 different molecular forms of TNF-α. Macrophages are considered the most prolific sources. lymphoid cells, mast cells, endothelial cells, fibroblasts, and neuronal tissue. Two types of TNF receptors, TNF-R1 & TNF-R2, are present on virtually all cells except RBCs. Present during acute response to acute inflammatory responses to toxic environmental agents{silica, asbestos, air pollution particles, welding fumes, ozone}.
- 72. Chemokines Plays a critical role in this process of recruitment & maintenance of inflammatory cells in the lungs after environmental exposures. Produced by Ams, monocytes, neutrophils, T & B lymphocytes, NK cells, epithelial cells, fibroblasts, smooth muscle cells, mesothelial cells, and endothelial cells.
- 73. ADAPTIVE IMMUNITY The adaptive immune response to pulmonary pathogens includes (humoral & cellular components). Both B & T lymphocytes are present in normal lung. B cells are predominantly found in airway lymphoid aggregates, where they outnumber the T cells. In normal lavage samples, approximately 5-10% of cells are lymphocytes, which, in turn, can be further divided into functionally important subsets, for example, CD4+ T helpers & CD8+ cytotoxic T cells.
- 76. In response to certain infectious agents & persistent foreign material, & as part of a disease of unknown etiology (e.g., sarcoidosis). Chronic inflammation, dominated by mononuclear phagocytes “macrophages, epithelioid cells, & multinucleated giant cells”. Typically, these cells congregate & form well- demarcated focal lesions called granulomas. Admixture of other cells,(lymphocytes, plasma cells, & fibroblasts). Granuloma formation typically ends in fibrosis. Fibrosis serves to wall off the granuloma contents and limit spread of infection and organ damage.
