5 dermatological causes of white patches
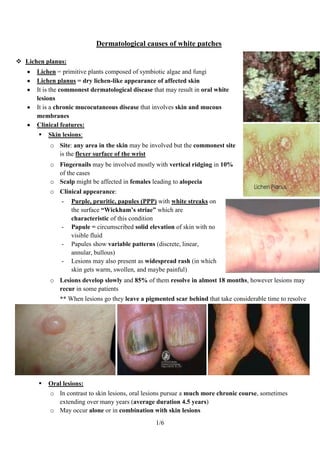
- 1. Dermatological causes of white patches Lichen planus: Lichen = primitive plants composed of symbiotic algae and fungi Lichen planus = dry lichen-like appearance of affected skin It is the commonest dermatological disease that may result in oral white lesions It is a chronic mucocutaneous disease that involves skin and mucous membranes Clinical features: Skin lesions: o Site: any area in the skin may be involved but the commonest site is the flexer surface of the wrist o Fingernails may be involved mostly with vertical ridging in 10% of the cases o Scalp might be affected in females leading to alopecia o Clinical appearance: - Purple, pruritic, papules (PPP) with white streaks on the surface “Wickham’s striae” which are characteristic of this condition - Papule = circumscribed solid elevation of skin with no visible fluid - Papules show variable patterns (discrete, linear, annular, bullous) - Lesions may also present as widespread rash (in which skin gets warm, swollen, and maybe painful) o Lesions develop slowly and 85% of them resolve in almost 18 months, however lesions may recur in some patients ** When lesions go they leave a pigmented scar behind that take considerable time to resolve Oral lesions: o In contrast to skin lesions, oral lesions pursue a much more chronic course, sometimes extending over many years (average duration 4.5 years) o May occur alone or in combination with skin lesions 1/6
- 2. o Site: lesions mostly affect buccal mucosa (90%), but may also affect the tongue, gingiva, palate, and lips. The floor of the mouth involvement is relatively uncommon o Lesions are often bilateral and show wide spectrum of presentations o Clinical appearance: - Non-erosive lesions: Reticular, annular, papular, plaque-like ** Reticular lesions have white streaks arranged in lace-like pattern ** Plaque-like lesions are white patches resembling leukoplakia clinically ** Papular lesions are small white papules that may coalesce ** Bullous lesions are subepithelial bullae They are usually asymptomatic They may show hyperkeratosis with NO atrophy & NO ulceration Reticular Annular Papular Plaque-like - Erosive/atrophic lesions: ** Erosive lesions are extensive areas of shallow ulceration ** Atrophic lesions are diffuse red lesions resembling Erythroplakia Erosion and atrophy are usually present together and lesions have a red glazed appearance with areas of superficial ulceration which may take several weeks to heal Occasionally, ulcers are preceded by bullae (bullous type) that then rupture Lesions are often associated with typical areas of non-erosive lichen planus They are usually symptomatic Pain and discomfort may be severe (especially when eating spicy/acidic foods) - Gingival lesions: Lichen planus involving the gingiva often presents as a desquamative gingivitis 2/6
- 3. Desquamative gingivitis is a clinical descriptive term that doesn’t infer any specific underlying pathology (so that it has many causes!) Gingival lesions may occur alone (in 10% of cases) or with other oral lesions Prevalence: o Lichen planus is a relatively common disease (affects 0.5-2% of general population) o There's a worldwide distribution o Peak incidence is found between ages 30-50 o Lesions are more common in females (60% of cases) o Oral lesions are detected in ~50% of patients with initial skin lesions o Skin lesions are detected in ~10-50% of patients with initial oral lesions!! This may be due to: - Asymptomatic nature of oral lesions in many cases - Inconstant relationship of oral and skin lesions (oral lesions may occur BEFORE, AFTER or AT THE SAME TIME as skin lesions) Histopathological features: o Orthokeratosis or Parakeratosis o Epithelial atrophy or acanthosis o Acanthosis results in irregular elongation and widening of the rete ridges in a “saw-tooth pattern” o Dense, well-defined band of subepithelial mononuclear infiltrate (mainly T-lymphocytes) o Liquefactive degeneration of the basal cell layer with edema and lymphocytic infiltration o The degenerating cells appear as hyaline shrunken bodies, called Civatte bodies o Basal cell degeneration may result in subepithelial bullae formation and ulceration because of the lack of cohesion between epithelium and lamina propria following the degeneration 3/6
- 4. o Oral lesions may show little superficial resemblance to skin lesions clinically even though the basic histological changes are similar, because of the modifying environment of the oral cavity by: - Continuous presence of saliva - Secondary infection by oral organisms - Repeated trauma o Almost all cases run a benign course o Malignant transformation has been described in a very small proportion (0.5%-2.5% over 5 years) o Some studies suggest that atrophic/erosive forms are more likely for such transformation because of the decreased barrier presented to potential carcinogens o Other studies found malignant transformation more likely with plaque lesions Etiology & pathogenesis: o It is NOT fully understood o In most cases the precipitating factors are unknown and the disease is Idiopathic o It is widely accepted that cell-mediated immune responses to an external antigen, or internal antigenic changes in epithelial cells, are involved since response resembles type IV hypersensitivity reaction which is T-cell mediated o Cytotoxic lymphocytes damage the basal epithelium ** Possible immunological mechanism in lichen planus: External antigen challenge and/or modified antigenic structure of epithelial cells induces cytokines release from langerhans cells & keratinocytes chemotaxis of lymphocytes which accumulate in the basement membrane zone & basal epithelium antigen presentation to CD4 helper cells activation of CD8 Cytotoxic cells basal cell degeneration o Lichen planus has been associated with some systemic diseases, in many of these, a cause-and- effect relationship has not been established (e.g. there is strong association of the disease with chronic liver disease especially hepatitis C virus) o Oral & skin lesions resembling lichen planus are also seen as a part of graft-versus-host reaction (immune reactions in patients receiving transplants), in such cases, the transplanted T cells react to antigens on host epithelial cells o Lichenoid reaction: - Lichenoid = lichen-like - In some patients, lesions similar to lichen planus may appear triggered by hypersensitivity reaction (IV) to certain drugs (NSAIDs) or dental materials (amalgam) - These lesions are clinically and histologically similar to Lichen planus, but tend to be reversible so that they resolve upon withdrawal of the offending agent ** Lichenoid reactions aren't idiopathic as lichen planus ** Lichenoid reactions are usually unilateral while lichen planus is usually bilateral 4/6
- 5. Lupus Erythematosus (LE): It is a chronic mucocutaneous disease that involves skin and mucous membranes and believed to be due to an autoimmune process It has two main forms: 1. Chronic discoid lupus erythematosus localized 2. Systemic lupus erythematosus disseminated Lesions are more common in females Clinical features: 1. Chronic discoid lupus erythematosus (DLE): o It is the localized form of the disease in which skin lesions occur without any systemic involvement o Site: lesions are usually restricted to the skin, and confined to the face o Clinical presentation: - Skin lesions: Lesions appear as scaly or crusted red patches that heal with scar Sometimes facial lesions have a symmetrical distribution over the nose and cheek, the so-called (butterfly rash) ** This butterfly rash can be seen in both forms Follicular plugging “hair follicles being plugged and prevented from going out and growing leading to hair loss) - Oral lesions: Lesions are found in up to 50% of cases Buccal mucosa is most frequently affected There's considerable variation in the usual presentation of oral lesions but the most common is a discoid area of Erythema or ulceration surrounded by white Keratotic border sometimes with radiating striae (resembling lichen planus) o Histopathology: - Orthokeratosis or Parakeratosis 5/6
- 6. - Epithelial atrophy or acanthosis - Keratin plugging - The subepithelial lymphocytes are aggregated in follicles and don’t show the clear band-like arrangement as in lichen planus - Liquefactive degeneration of basal cells - Circulating autoantibodies are found in one- third of patients 2. Systemic Lupus Erythematous (SLE): o It is the disseminated form of the disease in which skin lesions occur with systemic involvement o Site: skin lesions typically affect the face “cheeks” and the hands o Photosensitivity may be implicated in lesions eruption o May be fatal o Clinical presentation: - Skin lesions: Skin rashes (maculopapular) Sometimes facial lesions have a symmetrical distribution over the nose and cheek, the so-called (butterfly rash) - Oral lesions: They are variable Superficial erosions and erythematous patches on the buccal mucosa White Keratotic areas are not so frequently seen as in DLE o Histopathology: - Non specific diffuse inflammatory infiltrate - A variety of circulating autoantibodies are almost always present (e.g. antinuclear antibodies (ANAs)) 6/6
