Detailed approach to thyroid gland and parathyroid glands
- 1. 1 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 THYROID AND PARATHYROID DISORDERS BY DR. MAGDI AWAD SASI 2013
- 2. 2 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Thyroid Gland Anatomy Largest endocrine gland; high rate of blood flow Anterior and lateral sides of trachea o Two large lobes connected by isthmus Thyroid follicles o Filled with colloid and lined with simple cuboidal epithelial (follicular cells) that secretes two hormones, T3 and T4 . Thyroid Gland physiology: Synthesis and release of thyroid hormones is influenced by TSH from the pituitary. Two kinds of hormones are produce in the thyroid gland triiodothyronine (T3) and thyroxine (T4). Concern the regulation of the metabolic and oxidation rates in all the tissues of the body except the brain.
- 3. 3 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 At physiological levels, they stimulate growth and development with synthesis of many enzymes. At pharmacological levels, increased heat production and O2 consumption related in part to uncoupling of oxidative phosphoryiation. Many of the effects appear to be mediated by way of sympathetic nervous system. The sympathetic overactivity seen in many patients with anxiety states accounts for the frequent mistakes in diagnosis. Hypothalamus - the highest control of thyroid function((TRH)). Thyroid hormone o Body’s metabolic rate and O2 consumption o Calorigenic effect - heat production o heart rate and contraction strength o respiratory rate o Stimulates appetite and breakdown CHO, lipids and proteins o Alertness, bone growth/remodeling C (calcitonin or parafollicular) cells o Produce calcitonin blood Ca2+ , promotes Ca2+ deposition and bone formation especially in children What is Hyperthyroidism ? Increased synthesis and production of too much thyroid hormones is called hyperthyroidism. This leads to thyrotoxicosis. Thyrotoxicosis is the over production of thyroid hormones without increased synthesis. Thyrotoxicosis could be a result of thyroditis or too much intake of exogenous thyroid hormone.
- 4. 4 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 What Causes Hyperthyroidism? Hyperthyroidism can be that the whole gland is producing too much hormones or there is only a single nodule producing more than enough hormones. When this happens, the single nodule is called "hot nodule". causes of hyperthyroidism and thyrotoxicosis: 1. Too much iodine intake 2. Autoimmune --Graves' disease-the most common Thyroiditis-Hashimoto's, DeQuervain's, reidls thyroiditis. 3. Noncancerous growths of thyroid or pituitary gland 4. Toxic thyroid adenoma 5. Toxic multinodular goiter 6. Postpartum thyroiditis 7. TSH-secreting tumors (pituitary) 8. HCG-producing tumors 9. Hyper functioning ovarian teratoma. 10.Overmedicating with synthetic thyroid hormone. 11.Drugs—Amidarone. 12.Thyrotoxicosis factitia Symptoms of thyrotoxicosis: Hyperthyroidism can either be symptomatic or asymptomatic. It can be acute or chronic depending on the length with which the thyroid gland has been producing more than normal amounts of the hormones. The symptoms usually begin slowly and are not noticeable as can be largely attributed to stress only. As time goes , the symptoms will become more pronounced. The paradoxical association of loss of weight with normal or increased appetite is particularly suggestive of hyperthyroidism.
- 5. 5 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 D/D Diabetes mellitus--------Defective alimentary absorption. The weight is gained if increased appetite is more than the metabolic rate I. Heat production increased: Heat intolerance increased sweating II. CNS--- pt can’t keep still. Undue fatigability , proximal muscle weakness( thyrotoxic myopathy) ,hyperkinesias—exaggerated and purposeless movements ,Difficulty concentrating ,tremors , Emotion liability.(mysthenia gravis association 10% ). III. Psychiatric: Nervousness and anxiety, Irritability, sleep disturbance, Psychosis , insomnia. IV. CVS--- palpitation , dyspnea on exertion , chest pain,CCF The elderly patient usually present with cardiovascular symptoms ((predominant or alone)). Unexplained heart failure after middle age should always arouse suspicion of hyperthyroidism. Failure of digitalis in normal dosage to control the rapid heart rate is very suggestive. Many of the effects appear to be mediated by way of sympathetic nervous system sensitivity. Difficulty in stabilizing a diabetic patient is sometimes the first clue to the thyroid disorder. V. GIT---Weight loss despite an increased appetite, diarrhea, heartburn. For weight variation according to age, Young –increased weight /// Elderly- weight decreased. VI. Musculoskeletal system and growth: Pain in the back—thyrotoxic kyphosis resulting from osteoporosis Hypercalcemia with its clinical squeal is very rare, arthralgia , proximal muscle weakness.
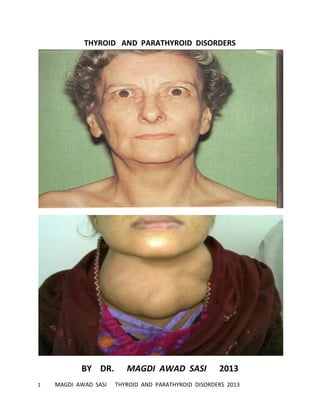
- 6. 6 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 VII. Integument: Loss of hair. Nails may show recession from the nail bed. Polyuria and polydypsia—less common. NECK---- A visible enlargement of the thyroid gland in the neck (goiter) EYES---Exophthalmos - protruding eyes, diplopia, chemosis, swelling Menstrual cycle variations – lightening of menstrual flow and less frequent periods. CLINICAL FINDING : If there is neck swelling (GOITER) ,it is a must to pass through 4 steps. 1. Inspection---site,size ,shape,skin changes,surface . ASK THE PATIENT TO SWALLOW—PATHOGNOMIC 2. Palpation- contirm , temperature, borders, consistency,tendenrness 3. Percussion----for retrosternal extension 4. Auscultation--- for bruit Exam the eyes for eye signs --is it Graves. Skin –feels warm , moist skin with fever. CVS— PULSE—collapsing , sleeping heart rate 80/min , atrial fibrillation BLOOD PRESSURE--- systolic HTN with high pulse pressure.
- 7. 7 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 CCF--- raised JVP , pedal edema, systolic murmurs CNS---hyperactive reflexes CLINICAL SIGNS IN GRAVES DISEASE: Increase in thyroid gland size Soft to slightly firm Non-nodular / nodular Bruit and/or thrill Mobile Non-tender Without prominent adenopathy EYE SIGNS: Ophthalamic Graves disease: 1. Swelling of the eyelids- Due to overfilling of orbit. The lids appear congested and edematous –congestive ophthalmopathy. 2. Irritation of the conjunctivae: .Grittiness and soeness of the eyes. .Edema of conjunctiva( chemosis)
- 8. 8 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 .It may ulcerate and may prolapse between the lids. .Corneal Damage may occure. .The appearance of prominent vessels at the lateral canthi is usually a sign that the ocular manifestation are going to be trouble some. 3. Exophthalmos: Appearance of sclera B/W the lower lid and limbus of cornea . Means protrusion of the eye ball. Symmetrical in Graves disease with hyperthyroidism. Caused by increased bulk of orbital contents. The fat is increased and the muscles enlarged, infiltrated with lymphocytes and contain increased amounts of water and mucopolysccharides. Usually alters little with treatment and may be remarkably persistent. In some, it is progressive and may cause loss of vision if effective treatment not given ((malignant exophthalmos )). Unilateral exophthalmos causes: 1.Retro-orbital aneurysm 2.Retro-orbital tumor 3. Involvement from outside 4. Chronic myopia 4. Lid retraction: Recognized by the appearance of sclera B/W The upper lid and the limbus of the cornea when the patient is looking straight a head and not staring. 2types: 1.Spastic lid retraction: It is diagnostic of Graves disease. It is present in all positions of gaze
- 9. 9 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 It is one of the commonest eye signs of Graves disease It is due to spasm of the elevator palpebrae superioros and sympathetic stimulation of the superior orbital muscle of muller. 2.Paralytic lid retraction: Not specific for Graves disease. Occurs only in the presence of limitation of upward gaze I. Disorders of the muscles-Graves disease, ocular myopathy II. Mysthenia gravis III. Upper brain stem lesions It is thought to be caused by over innervations of elevator palpebrae superioros when an attempt is made to look up. Lid retraction is the cause of a conjunctival irritation and keratitis. 5. Lid lag: NORMAL LID LAG Occurs when the sclera B/W upper eye lid and cornea becomes visible as the patient gaze follows the examiner fingers down ward from the position of maximum elevation. The eye moves not in close contact with eye lid as a delay in lid movement.
- 10. 10 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 6.Ophthalmoplegia: Paresis of one or more of extraocular muscles usually causes diplopia. Upward and outwards movements reduced 4 times. Limitation of upward gaze may be due to tethering and adhesions of inferior oblique and superior rectus muscle when they decussate. It is pathognomic in Graves disease . It is one of the most unpleasant ocular complication of graves . 7.Congestive ophthalmopathy: malignant exophthalmos IT IS A MEDICAL EMERGENCY REQUIRING IMMEDIATE ADMISSION. The patient complain of severe pain in the eye or failure of vision. It is a sever and progressive ocular changes in Graves characterized by: 1. Prominent eyes 2. Lids and conjunctiva swollen and inflamed 3. Marked ophthamoplegia 4. Retinal veins may be prominent. 5. Papilloedema may develop. 6. Oular tensions may be high. 7. Keratitis 8. Pressure on the optic nerve may be sudden and complete which causes loss of vision even with normal fundus.
- 11. 11 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Clinical Differentiation of Lid Retraction from Proptosis Measurement using prisms or special ruler (exophthalmometer) OR with sclera seen above iris : Observing position of lower lid (sclera seen below iris = proptosis, lid intersects iris = lid retraction) Normal position of eyelids Proptosis Lid retraction SKIN SIGNS---PRETIBIAL MYXEDEMA 5% of patients. Usually affects the shins frontal area The swelling often extends over the dorsum of the feet and toes where it is associated with tissue growth. The skin is coarse ,purplish –red , peaud orande appearance ,raised surface Thick, leathery consistency, with coarse hair in the affected area.
- 12. 12 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 The superficial layer of the skin is infiltrated with the mucopolysaccharide hyaluronic acid. Nodularity, sometimes. Sharply demarcated margins,Non-tender. It tends to develop after hyperthyroidism has been treated by surgery or with radioactive iodine. The latent period take 4- 32months. Soft tissue swelling that is pigmented and hyperkeratotic. Thyroid Acropachy Clubbing of fingers. Painless. Periosteal bone formation and periosteal proliferation . The subperiosteal new bone formation resembles soap bubbles on the surface of bone with coarse spicules.
- 13. 13 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Onycholysis of Thyrotoxicosis Distal separation of the Nail plate from nail bed Plummer’s nails) Frequency of Neuromuscular Disorders Associated with Thyrotoxicosis: Myopathy due to thyrotoxicosis >50 Usually proximal and mild to moderate Hypokalemic periodic paralysis <1 Myasthenia gravis <1 Thyrotoxic Periodic Paralysis: Most common cause of hypokalemic periodic paralysis Flaccid paralysis Lower extremities affected most often Ocular and bulbar muscles uninvolved, respiratory muscles rarely involved Most often starts during sleep Precipitated following exercise, high salt intake or high carbohydrate diet Hypokalemia during the paralysis .
- 14. 14 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Differential Diagnosis of a Painful Thyroid: Subacute granulomatous thyroiditis Most common Hemorrhage into a goiter, tumor or cyst with or without demonstrable trauma Less common Acute suppurative thyroiditis <1% Anaplastic (inflammatory) thyroid carcinoma <1% Hashimoto’s thyroiditis <1% TB, atypical TB, amyloidosis <1% Metastatic carcinoma Diagnosis Many symptoms of hyperthyroidism are the same as those of other diseases, so hyperthyroidism usually cannot be diagnosed based on symptoms alone. With suspected hyperthyroidism, you have to take a medical history and perform a thorough physical exam. Several blood tests confirm the diagnosis of hyperthyroidism and find its cause: 1. **TSH test** The first test , The most accurate measure of thyroid activity available. The TSH test is especially useful in detecting mild hyperthyroidism. Generally, a TSH reading below normal means a person has hyperthyroidism and a reading above normal means a person has hypothyroidism. 2. **T3 and T4 test** With hyperthyroidism, the levels of one or both of these hormones in the blood are higher than normal 3. Thyroid-stimulating immunoglobulin (TSI) test ((Thyroid stimulating antibody test)) measures the level of TSI in the blood. Most people with Graves’ disease have this antibody.
- 15. 15 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 4. Ultrasound neck- U/S more sensitive than physical examination , particularly for nodules that are < 1 cm or located posteriorly in the gland. U/S also more sensitive than thyroid scan Thyroid U/S Benign Characteristics Malignant Characteristics Regular border Halo (sonolucent rim) Irregular border No Halo Hyperechoic Hypoechoic (more vascular) Egg shell calcification Microcalcification N/A Intranodular vascular spots (color doppler) 5. **Radioactive iodine uptake test** low levels of iodine uptake might be a sign of thyroiditis, whereas high levels could indicate Graves’ disease.
- 16. 16 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Causes of Thyrotoxicosis Divided by Degree of Radioiodine Uptake High I123 Uptake Graves’ disease Toxic nodular goiter TSH-mediated thyrotoxicosis Pituitary tumor Pituitary resistance to thyroid hormone HCG-mediated thyrotoxicosis Hydatidiform mole Choriocarcinoma Other HCG-secreting tumors Thyroid carcinoma (very rare) I123 Low I123 Uptake Subacute thyroiditis Hashitoxicosis Drug-induced Iodide Thyroid hormone Struma ovarii Factitious I123 6. **Thyroid scan** A thyroid scan shows how and where iodine is distributed in the thyroid. The images of nodules and other possible irregularities help to diagnose the cause of a person’s hyperthyroidism. Thyroid Scan Thyroid nodule: risk of malignancy 6.5% Cold nodule 16-20% malignant “Warm” Nodule (indeterminant) 5% malignant Hot Nodule Tc-99m < 5% malignant I123 < 1% malignant only 5-10% of nodules
- 17. 17 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 7. FINE NEEDLE ASPIRATION • 25G Needle, 10cc syringe • Done in Office • NOT INDICATED IN TOXIC PATIENTS . • +/- Local anaesthesia • 3-5 passes • SEN 95-99% (False Negative rate 1-5%) • SPEC > 95% • Benign: macrofollicular or "colloid" adenomas, chronic autoimmune (Hashimoto's) thyroiditis • Suspicious or Indeterminant: microfollicular or cellular adenomas (follicular neoplasm) Treatment: Hyperthyroidism is treated with medications, radioiodine therapy, or thyroid surgery. The aim of treatment is to bring thyroid hormone levels to a normal state, thus preventing long-term complications, and to relieve uncomfortable symptoms. No single treatment works for everyone. Treatment depends on the cause of hyperthyroidism and how severe it is. When choosing a treatment, consider 1. Patient’s age 2. Side effects of the medications 3. Pregnancy or heart disease 4. The availability of an experienced thyroid surgeon. Medications 1. Beta blockers Beta blockers act quickly to relieve many of the symptoms of hyperthyroidism, such as tremors, rapid heartbeat, and nervousness, but do not stop thyroid hormone production. Most people feel better within hours of taking these medications.
- 18. 18 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 2. Antithyroid medications : Treatment of hyperthyroidism Antithyroid drugs Carbimazole 10 mg tid Reduce to maintenance after 4 weeks Rash, GI, agranulocytosis Graves – withdraw drugs after course of treatment Carbimazole, thiouracil ,methimazol Antithyroid medications interfere with thyroid hormone production but don’t usually have permanent results. Antithyroid medications are not used to treat thyroiditis. Once treatment with antithyroid medications begins, thyroid hormone levels may not move into the normal range for several weeks or months. The average treatment time is about 1 to 2 years, but treatment can continue for many years. Side effects in some people, including: 1. Allergic reactions such as rashes and itching 2.Agranuloctosis- decrease in the number of white blood cells in the body. 3. Liver failure, in rare cases Ask the patient to stop antithyroid medication if he develop: 1. Fatigue & weakness 3.Vague abdominal pain & Loss of appetite 5. Skin rash or itching & Easy bruising 7. Jaundice 8. . Fever & persistent sore throat.
- 19. 19 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Antithyroid medications and pregnancy Radioiodine therapy is contraindicated . propylthiouracil (PTU), is available for women in this stage of pregnancy or for women who are allergic to methimazole and have no other treatment options. Some women are able to stop taking antithyroid medications in the last 4 to 8 weeks of pregnancy due to the remission of hyperthyroidism that occurs during pregnancy. However these women should continue to be monitored for recurrence of thyroid problems following delivery. Methimazole: Advantage –1.less frequent doses , fewer pills & more convenient. 2. lower incidence of acute hepatic necrosis. Complications: Serum sickness Cholestatic jaundice Hypoglycemia Loss of taste Alopecia Nephritic syndrome Dose (10mg) 30---60 mg once daily Indications : 1. Toxic Goiter 2. Preparing hypetthyroid for surgery 3. Preparing elderly fo RAI 4. Mild toxicosis
- 20. 20 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 3. Radioiodine Therapy In radioiodine therapy, patients take radioactive iodine-131 by mouth. Because the thyroid gland collects iodine to make thyroid hormone, it will collect the radioactive iodine from the bloodstream in the same way. The radioactive iodine gradually destroys the cells that make up the thyroid gland but does not affect other body tissues. Treatment of hyperthyroidism Radio-iodine Inflammatory response followed by fibrosis May be used for Graves, TMG or TA ? Need for drug treatment before and after May need retreatment Long term risk of hypothyroidism Treatment with beta blockers can control symptoms. women wait a year after treatment before becoming pregnant. 4. Thyroid Surgery((least-used)) Surgery may be used to treat: 1.Pregnant women who cannot tolerate antithyroid medications 2.Large goiters and Cancerous thyroid nodules Before surgery, we may prescribe antithyroid medications to temporarily bring a patient’s thyroid hormone levels into the normal range. This presurgical treatment prevents a condition called thyroid storm—a sudden, severe worsening of symptoms—that can occur when hyperthyroid patients have general anesthesia.
- 21. 21 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Treatment of Hyperthyroidism Surgery Rarely used nowadays Need to be rendered euthyroid before surgery Lugol’s iodine 0.1-0.3 mls tid for 10 days before surgery DRUGS USED IN THYROTOXICITY
- 22. 22 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 After surgery: A. When part of the thyroid is removed, T3T4 levels may return to normal B. Some patients may still develop hypothyroidism, need thyroxine. C. If the entire thyroid is removed, lifelong thyroxine is necessary. D. After surgery, patients’ thyroid hormone levels should be monitored. Facts TO REMMEBER: Hyperthyroidism is a disorder that occurs when the thyroid gland makes more thyroid hormone than the body needs. Hyperthyroidism is most often caused by Graves’ disease, an autoimmune disorder. Hyperthyroidism is much more common in women than men. Hyperthyroidism is also more common in people older than age 60 and is often caused by thyroid nodules. Hyperthyroidism in this age group is sometimes misdiagnosed as depression or dementia. For people older than age 60, subclinical hyperthyroidism increases their chance of developing atrial fibrillation , heart failure. Hyperthyroidism is treated with medications, radioiodine therapy, or thyroid surgery. No single treatment works for everyone. Treatment by medication- antithyroid and B blockers . Hyperthyodism will not cause carcinoma. Exophthalmos is characteristic for graves disease. After RAI therapy, hypothyroidism is the rule and TR is thyroxine lifelong. Treatment of Hyperthyroidism IN USA: Make diagnosis, get RAI uptake. Beta block (inderal 40-80 mg tid). If RAI uptake is high – treat with RAI. If RAI is low – symptomatic
- 23. 23 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Graves Eye Disease Usually mild – Tx, protective glasses, elevate head of bed, conjunctival lubricants High dose steroids External radiotherapy Orbital decompression Toxic Solitary Adenoma Rare cause (< 2% of patients with hyperthyroidism) Younger people 30’s and 40’s Scan Benign follicular adenomas
- 24. 24 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Toxic solitary nodule Less than 40year more than 40year 1.Make pt euthyrod by: 1.Radioactive iodine Propraolol, thiourea A.Permenant hypothyroid 2.Before 10 days of O.T. Iodine therapy. 1/3 of pt by 8 yr afterRAI 3.Surgery B. Nodule remain in50% C.10% of pt may grow. Post operative hypothyroidism -Trsnsiet.14% become hypothyroid By 6 years after surgery. MULTINODULAR GOITER: Older Usually less severe hyperthyroidism May have subclinical hyperthyroidism. May have long history of goitre A thyroid containing multiple nodules is likely to be benign MNG. Fine needle biopsy is performed on any nodule that is growing / dominant/ hard inconsistency.
- 25. 25 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Larger retrosternal goiter rarely harbor a malignancy but can be followed by CT. 1.Surgical resection=compression 2 .Thyroxine useful in pt TSH or Continuous growth Thyroxine should not be prescribed 3.Pt found be toxic may have RAI scan For pt w suppressed TSH since may IF I123 is a therapeutic consideartion Add to autonomous secretion and cause thyrotoxicosis Uss guided FNA biopsy is reserved for pts with nonpalpable nodules 1.5cm in diameter with H/O head-neck irradiation. TOXIC MULITNODULAR GOITER 1.Symptomatically with propranolol/thiourea 3.PT follow a low iodine diet to Enhance thyroid uptake of RAI 95% recurrence rate after they are stopped. Which may be relatively low . 2. RAI should be given after stopping T.U./ 3days 4.High doses 0f RAI required. And reender patient euthyroid. 5.Pt should be followed closely Hyper and hypo are common 6.SURGERY FOR COSMOTIC AND PRESSURE SYMPTOMS
- 26. 26 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 EMERGENCY THYROID STATUS ((THYROID STORM)) It is an exacerbation of hyperthyroidism. IT is an acute life threatening , hypermetabolic state which may be the initial presentation of thyrotoxicosis. Less than 10% of hospitalized thyrotoxicosis. Mortality 20---30% Can be caused by all causes of hyperthyroidism but Graves the most common. Precipitating event: I. Systemic insult—surgery, trauma ,myocardial infarction ,pulmonary embolism, severe infection, DKA. II. Discontinution of antithyroid drugs III. Excessive iodine ( amiodarone , radiocontrast dyes) IV. Radioiodine therapy Symptoms: o Increased all vital signs o Increased body temperature, sweating o Tachycardia, Arrythmia, atrial fibrillation o Vomiting/ nausea, dyspnea, tacchypnea o Diarrhea, epigastric discomfort o Heart failure/ pulmonary odema o Confusion LABORATORY: o Increased free T4 AND T3 o Decreased TSH o Hyperglycemia , elevated alkaline phosphatase, leukocytosis, Mild hypercalcemia , and elevated liver enzymes. o Cortisol increase (( NORMAL LEVEL = ADRENAL INSUFFICIENCY))
- 27. 27 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Treatment: A. TREATMENT DIRECTED AT THYROID GLAND AND HORMONES-- Inhibition of new hormone synthesis with Thioamide drugs such as PTU and methimazole. Inhibition of hormone release with Iodine & potassium iodide(Lugols solution) & Lithium carbonate. B. TREATMENT DIRECTED AT PREVENTING HORMONES AFFECTS ON THE BODY PTU , Corticosteroids ,B blockes( propanolol),Amiodarone, Plasmapheresis. C. TREATMENTS DIRECTED AT MAINTAINING HOMEOSTASIS Hyperthermia—acetaminophen , cooling , blankets Fluid and electrolyte testing / replacement Glucose Vasopressors Digoxin and diuretics if appropriate. BETA BLOCKERS—decrease adrenergic hyperactivity PTU------------------blocks the peripheral conversion of T4 TO T3. GLUCOCORTICOIDS—inhibit hormone production and decrease peripheral conversion from T4 to T3. SODIUM IODIDE SOLUTION(LUGOLS)—high levels of iodide will initially suppress release of thyroid hormone Treat cardiac symptoms , fever and hypertension. “Apathetic Hyperthyroidism” Common symptoms: Weight loss, anorexia Constipation despite thyrotoxic Tachycardia, Atrial fibrillation , Heart failure, angina Cognitive Dysfunction
- 28. 28 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Hypothyroidism Definition: Hypometabolic state due to deficiency of thyroid hormones . Hypothyroidism results specially from glandular destruction and underproduction of thyroid hormones. It is characterized by Accumulation of mucopolysaccharides in the SC tissue ((non pitting edema )). Incidence : middle -50s female:male ratio → 10:1 ETIOLOGY A. PRIMARY : THYROID FAILURE (95%) B. SECONDARY : PITUITARY TSH DEFICIT C. TERTIARY : HYPOTHALAMIC DEFICIENCY OF TSH D. PERIPHERAL RESISTANCE TO THE ACTIONS OF THYROID HORMONES • Autoimmune hypothyroidism: -Hashimoto’s thyroiditis - Atrophic thyroiditis • Iatrogenic: -Radio-iodine therapy - Thyroidectomy - External radiation to the neck (lymphoma/CA) • Drugs : -Antithyroid drugs, amiodarone, lithium, interferon • Congenital hypothyroidism: -Thyroid agenesis - Dyshormogenesis - TSH-R mutation PRIMARY CAUSES • Iodine deficiency • Infiltrative disorder Infiltrative disorders: amyloidosis, sarcoidosis, hemochromatosis…
- 29. 29 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Transient hypothyroidism: 1. Silent thyroiditis , including postpartum thyroidtis 2. Subacute thyroiditis 3. Withdrawal of thyroxine trt B. Secondary hypothyroidism: 1. Hypopituitarism: tumors, pituitary surgery or irradiation, infiltrative disorders, Sheehan’s syndrome, trauma C.3ry -Hypothalamic disease: tumors, trauma, infiltrative disorders . Clinical manifestations: There will be systemic symptoms which may delay the diagnosis. It is diagnosed either at first sight or not at all. Myxedema enters into D/D of unexplained heart failure not responding to diuretics and digoxin. Myxedem enters into D/D unexplained ascitis(protein content high). The pituitary is often quite enlarged in 1ry hypothyrodism due to reversible hyperpalsia of TSH- secreting cells. The concomitant hyperprolactinemia seen in hypothyrodism can lead to mistaken diagnosis of pituitary adenoma. CNS—Tiredness ,weakness, Difficulty concentrating and poor memory thought and movements are retarded, parasthesia , thyroid maddness,speech is slow , hoarse voice , depression, psychosis, confusion, Perceptive deafness(40%)of all cases. CVS—Fatigue , Dyspnea , lose of effort , legs swelling , syncopy Angina pectoris , CCF,pericardial sffusion. GIT---lose of apetite , abdomenal distention ,constipation .
- 30. 30 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 SKIN- Dry skin , feeling cold , thick coarse skin. Endo----Weight gain , cold intolerance , hair loss MENSTRAUL CYCLE----menorrhagia , Dysmenorrhea. Amenorrhea may be the presenting feature in young patients. They have a tendency for fluid collection in negative spaces even in the absence of bilateral leg swellings. The patient may present with unexpained symptomatic pleural effusion or ascitis or pericardial effusion .Hypothyrodism can be subclinical for long time as the patient may be at risk of coronary heart disease as low thyroid hormones elevate the cholestrol . Pericardial effusion may be huge and result into cardiac tymponade with heart failure symptoms . The commonest presentation: 1. Tingling and numbness in the fingers due to carpel tunnel syndrome. 2. Muscular aches & pains is a prominent feature following thyrodectomy. 3. Too much reliance should not be placed on thining of outer third of the eyebrows---------------uncommon in normal people Rare presenting features: 1.Hoffmans syndrome: Patient presents with stiff,aching ,swollen muscles
- 31. 31 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 2.CNS disorders: Epilepsy ,drop attacks ,dementia ,cerebellar ataxia ,peripheral neuropathy. All of which may in large part recover with thyroxine treatment. 3.Coma with hypothermia: Especially elder patient living alone with inadequate blanket. Precipitated by phenothiazine. In mild hypothyrodism, the symptoms are usually minor and non specific. Tiredness, Depression ,Puffiness of face , Periorbital swelling and constipation. May be present singly or in combination with out H/O thyroid diseases. CLINICAL SIGNS: Dry skin ,coarse ,thick and rough, distinict yellowish tint. Malar flush, cool peripheral extremities &cyanosis of ears Enlarged tongue D/D Amyloidosis. Puffy face,periorbital edema,pallor. Puffy hands and feet (non pitting thickning of S/C tissue) . Diffuse alopecia-dry ,brittle, sparse,come out easily. Hands –reynauds phenomena Bradycardia Delayed tendon reflex relaxation Carpal tunnel syndrome
- 32. 32 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013
- 33. 33 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Delayed Deep Tendon Reflex • Achilles’ tendon reflex time most commonly sought but may also be effectively tested on brachioradialis or biceps • Achilles’ tendon reflex timing is best elicited with patient kneeling. COMPLICATIONS OF HYPOTHYRODISM: 1. Mostly cardiac----CAD , CCF 2. Increased susceptibility to infections 3. Megacolon in long standing hypothyroidism 4. Organic psychosis with paranoid delusions (madness) 5. Infertility (rare cause) 6. Adrenal crisis may be precipitated by thyroid therapy. 7. Convulsions 8. Deep stupor & coma 9. Refractory hyponatremia in sever myxedema. 10 .Myxedematous pt are sensitive to opiates. 11. Inappropriate secretion of ADH has been observed 12. Sellar enlargement & TSH secreting tumors may develop in untreated pt which decrease in size after replacement therapy. LABORATORY INVESTIGATION: Suspicion of hypothyroidism in the appropriate clinical context is the key to diagnosis. A. Family history of thyroid disease, Goiter , vitiligo ,autoimmune disease.
- 34. 34 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 B. H/O previous destructive therapy • Diagnosis : serum TSH : serum T4 total or free? : thyroid autoantibodies • In outpatient setting → serum TSH !!! Dyslipidemia with elevated cholesterol and triglycerides Anemia CNOCLUSION: TSH ↑ and FT4 normal: subclinical hypothyroidism TSH ↑ and FT4↓:clinical hypothyroidism TSH normal or ↓ and FT4 ↓:secondary hypothyroidism MANAGEMENT: • Aim: to make patient euthyroid clinically & biochemically. • Treatment with L-thyroxine is life-long → ensure compliance!! Monitoring: • Clinically & biochemically • Measure TSH and free T4 2-3 month after initiation of therapy → determine maintenance dose.
- 35. 35 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 OVERT HYPOTHYROIDISM • Starting dose : 50-100 ug/d →→ 100-200ug/d within 2 weeks • IHD / grossly hypothyroid / elderly: • Start at 25 ug/d • ↑ slowly within 2-4/52 according to pt response • Angina: withhold / ↓ dose. Proper Management of IHD • Hypopituitarism: • Cortisol: to avoid adrenal crisis SUBCLINICAL HYPOTHYROIDISM: • L-thyroxine to ↓ risk of CAD • 50-100 ug/d →→ adjust to maintain TSH at normal level • Most asymptomatic & don’t need Rx (monitor TSH q2-5y) • Treatment Indications: A. Increased risk of progression B. TSH > 10, Female > 50 year old. C. Anti-TPO Ab titre > 1:100,000 ? D. Goitre present ? E. Dyslipidemia? F. Total cholesterol (TC) 6-8% if TSH > 10 and TC > 6.2 nM G. Symptoms? H. Pregnancy, Infertility, Ovulatory Dysfunction.
- 36. 36 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 PREGNANCY: • ↑ dose, especially in 2nd / 3rd trimester Levothyroxine (T4) • Eltroxin (GSK) • Synthetically made • 50 ug white pill no dye (hypoallergenic) • Most commonly prescribed treatment for hypothyroidism • No T3 (but 85% of T3 comes from T4 conversion) • All patients made euthyroid biochemically • Most (but not all) patients feel normal • Average dose 1.6 ug/kg • Age > 50-60 or cardiac disease: must start at a low dose (25 ug/d) • Recheck thyroid hormone levels every 4-6 weeks after a dose change • Aim for a normal TSH level • Medical situations where T4 medication may be affected.ex: A. Estrogen: Pregnancy, OCP, HRT i. Need to increase T4 dose! B. Drugs that interfere with T4 absorption i. Iron, Calcium ii. Cholestyramine (cholesterol resin Rx) At least 4h between T4 and these drugs!
- 37. 37 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Liothyronine (T3) • Cytomel (Theramed) • Shorter half-life • Fluctuating levels (i.e. need a slow-release pill) • Twice daily dosing often needed • 10x more potent: palpitations & other cardiac side effects • High T3 levels, low T4 levels (not physiologic either!) HYPOTHROID MEDICAL EMERGECY((MYXEDEMA COMA)) • Severe, uncompensated form of prolonged hypothyroidism. • Precipitated by stress / infection / drug • Complication: signs of hypothyroidism with 1 Hypoventilation 2. Cardiac failure 3. Fluid & electrolyte imbalance 4. Coma 50% of cases
- 38. 38 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 PLAN OF MANAGEMENT 1. Treat precipitating cause 2. Gradual rewarming → blanket 3. Accurate core T° → rectal thermometer – Aim for slow ↑ in core T° : 0.5 °C/hr 4. Cardiac monitoring 5. Correction of electrolyte abnormalities 6. Adequate hydration & nutrition (dextrose) 7. L-thyroxine (300-400 ug oral/iv) & tri-iodothyronine 10 ug 8 hrly 8. Hydrocortisone : blood cortisol THYROIDITIS CLASSIFICATION: SUBACUTE, NONSUPPURATIVE UNKNOWN CAUSE ASSOC. WITH VIRAL URT INFECTIONS CHRONIC, HASHIMOTO’S IMMUNOLOGICAL FACTORS PRESENCE OF IMMUNOGLOBULINS & ANTIBODIES DIRECTED AGAINST THE THYROID
- 39. 39 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Inflammation of the thyroid gland (thyroiditis) comprises many common disorders of the thyroid gland. Thyroiditis affects mainly women and can occur at any age. Affected patients can be euthyroid, hypothyroid or hyperthyroid depending on the cause. Many patients ultimately develop permanent hypothyroidism. Key learning points Hashimoto’s thyroiditis is the most common form of thyroiditis. Subacute or De Quervain’s thyroiditis is most likely due to a viral infection Thyroiditis can often lead to hypothyroidism developing. Amiodarone can cause hyperthyroidism or hypothyroidism An enlarging or hard thyroid could also be due to a carcinoma. Hashimoto’s Disease(( chronic lymphocytic thyroditis )): Most common cause of hypothyroidism in North America (not idodine defeciency!)& most common form of thyroditis. Autoimmune Its frequency is increased by dietary iodine. Females > Males 6 times , Runs in Families. Antithyroid antibodies: Thyroglobulin Ab ,Microsomal Ab ,TSH-R Ab (block) First preceded by subclinical hypothyroidism with normal thyroid hormones levels and elevated TSH Later ,FT4 levels fall and TSH levels rise further Auto antibodies can be induced by amidarone, interferon ,IL 2,GCSF. Anti TPO +++ C/F: Diffusely enlarged ,firm, finely nodules One lobe may be asymmetrically enlarged (D/D neoplasm) Pt c/o neck tightness, pain &tenderness are not present. 10% of cases are atrophic ,fibrotic particularly in elderly female. LAB.: antiperoxidase (95%) & antithyroglobulin(60%).
- 40. 40 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Treatment: Thyroid Hormone Replacement Levothyroxine (T4) No benefit to giving iodine! In fact, iodine may decrease hormone production Variety : 1.Subclinical thyroditis: Very common 40% female , antibodies 13% female 2.Postpartum thyroditis: Transient hyperthyroidism followed by hypothyroidism. Recovery is the rule. Subacute thyroditis: Common disorders De quervains thyroditis Granulomatous thyroditis Gaint cell thyroditis Presented by acute painful enlargement of thyroid gland and dysphagia . The pain may radiate to the ears. Silent thyroditis -----no pain Young and middle aged women are most commonly affected. Viral infection has been suggested as the cause. Clinically; the manifestation may persist for weeks or months and associated with thyrotoxicosis. LAB.: ESR increased and antithyroid antibodies decreased. I123 radioactive uptake is low Fine needle aspiration-----Gaint multinucleated cells.
- 41. 41 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Suppurative thyroditis: Rare disorder C/F-Severe pain, tenderness& redness, fluctuation in thyroid gland region. Caused by pyogenic organisms. Occurs in the course of systemic infection. Riedlels thyroditis(chronic fibrous thyroditis): It is called woody thyroiditis, ligamentous thyroiditis,riedles struma. It usually causes hypothyroidism and may cause hypoparathyrodism . Age –middle age or elder women. Enlargement is often asymmetric. The gland is stony hard and adherent to the neck structures. This leads to compression signs-Dysphagia, Dyspnea& hoarsness. It is usually a manifestation of a multifocal systemic fibrosis with: 1.Retroperitoneal fibrosis 2.Mediastinal fibrosis 3.Biliary tract sclerosis NOTES IN Thyroiditis: Painful (subacute, de Quervain’s) Painless (post partum) Hyperthyroid, hypothyroid and euthyroid phases Anti thyroid drug therapy does not work.
- 42. 42 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 THYROID TUMORS: 1. Follicular cancer: Common , 15% of thyroid malignancies. Age-50 year Female—72% More likely to have distant metastases Invasion juxtanodal + Blood vessels +++ Distant sites +++ Classified as differentiated thyroid carcinoma. Death 24% Resemble to normal thyroid +++ I 123 uptake +++ Degree of malignancy +++ C/F thyroid nodule =thyrotoxicosis LAB.----------thyroglobulin levels high in metastatic follicular carcinoma. Less common than papillary Imaging –extensive bones and soft tissue metastases may develop. Total thyroidectomy (or near total). Routine remnant ablation with RAI due to increased risk of metastatic disease 2. Papillary Cancer Most common (70% of all) and least aggressive. Differentiated thyroid carcinoma. Age –40year// female --- 70% Death --- 7% Invasion --juxtanodal ++++ Blood vessels + Distant sites + Resemble to normal thyroid + I123 uptake -cold nodule + C/F thyrotoxicosis with nodule
- 43. 43 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 LAB—thyroglobulin levels are high in most metastatic papillar ca. Imaging--- extensive bone and soft tissue metastasis may be detected on radioisotope scans. USS neck – solid lesion // CXR-------puntate calcification. Extent of surgery (near total thyroidectomy). Follow up with sTSH, thyroglobulin exam and US. Radioactive iodine ablation for high risk tumours. Follow up with RAI scans plus the above. Anaplastic carcinoma Rare ,1% thyroid carcinoma Age –57year// female 56% Deaths ---98% C/F: thyroid nodule Signs of pressure or invasion of surrounding structures Recurrent laryngeal nerve pulsy Invasion -- juxta nodal +++ Blood vessel +++++ Distant sites ++++ I123 uptake O Degree of malignancy +++++ Highly aggressive –locally and systematically Medullary carcinoma: Uncommon , less than 5% of thyroid cancer Average age—50year // female 56% Death 33% Invasion –tend to metastases locally Juxta nodal ++++ Blood vessels +++ Distant ++ Of all cases- 1/3 sporadic , 1/3 familial , 1/3 MEN type II
- 44. 44 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 I123 uptake O C/F: thyroid nodule --- firm non tender Anterior cervical lymph nodes may be enlarged. 1/3 Frequently secrete serotonin and PG leading to diarrhea and fatigue. LAB.:TFT--- normal except in thyroditis 2ry to cancer. Calcitonin levels may be elevated ,especially after stimulation by PG infusion. 2/3 Familial—children and siblings of patient with MC are advised to have genetic testing to detect RET-PROTO-ONCOGENE mutation. Imaging – tend to calcify Metastases may be detected by PET scan and MRI. Degree of malignancy--------- ++++ Worse prognosis if tissue stains heavily with calcitonin or MM AG LEU M1. Solitary Thyroid Nodule FNA Benign no further intervention Malignant or suspicious– papillary or follicular. Non-thyroidal illness patients may have low T3 and/or T4 usually with a normal sTSH Psychotic patients may have elevated T3 and/or T4. Simple non-toxic goiter Normal TFT’s No treatment required Surgery if obstructive symptoms
- 45. 45 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 SOLITARY THYROID NODULE Call for fine needle aspiration biopsy. 1.NODULAR WITH BENIGN CYTOLOGY 2.SOLITARY THYROID NODULE IN PT In a pt with H/O radiation therapy Need to be followed by 1.Periodic palpation At high risk of malignancy-resection 2.Rebiopsied if further growth occurs 3.Cystic nodules can be managed by 4.Solitary nodule in thyrotoxic pt removal of Fluid for cytology to are an indication of RAI scan deflate the cyst. To differentiate adenoma/graves Cysts recur and need repeated aspirations Thyroxine suppression therapy is ineffective In shrinking nodules unless the pt has primary a hot nodule is usually benign Hypothyroidism with increased TSH but resected to cure toxicity.
- 46. 46 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 NON-TOXIC GOITER COMMON IN WOMEN: ADOLESCENT PREGNANT LACTATING MENOPAUSE TREATMENT: IODIZED OIL IM IODINE TABLETS SALT FORTIFICATION WITH IODINE EDUCATE ABOUT INTAKE OF: SEAWEEDS SHELLFISH FISH- TAMBAN, HITO, DALAG
- 47. 47 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013
- 48. 48 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 PARATHYROID GLAND
- 49. 49 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 4 GLANDS SECRETES PARATHORMONE (PTH) IN RESPONSE TO SERUM Ca & Ph LEVELS REGULATE CALCIUM & PHOSPHORUS METABOLISM ORGANS AFFECTED: BONES - resorption KIDNEYS Ca reabsorption Ph excretion GIT – enhances Ca absorption DIAGNOSTIC TESTS: HEMATOLOGICAL SERUM CALCIUM SERUM PHOSPHORUS SERUM ALKALINE PHOSPHATASE URINARY STUDIES URINARY CALCIUM URINARY PHOSPHATE - TUBULAR REABSORPTION OF PHOSPHATE HYPOPARATHYROIDISM DECREASED PTH PRODUCTION HYPOCALCEMIA CALCIUM IS:
- 50. 50 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 DEPOSITED IN THE BONE EXCRETED CAUSE: HEREDITARY IDIOPATHIC SURGICAL - most common (transient, permenant) PARATHYROID ADENOMA RESECTION suppression of PTH AND accelerated remineralization of skeleton (Hungry bone syndrome) CONGENITALLY ABSENT HEAVY METALS- hemochromatosis, hemosiderosis, wilson disease DYSEMBRYOGENESIS---Dogeorgs syndrome INFECTION , GRANULOMA , SECONDARY FUNCTIONAL DECREASE PTH BY MG DEFICIENCY—maabsorption. NECK RADIATION POLYGLANDULAR AUTOIMMUNE Type1-----APECED Autoimmune poly endocrinopathy Candidiasis Ectodermal Dystrophy Present in childhood with 2/3: 1.Candidiasis 2.Addison disease 3. Hypoparathyrodism PT may develop cataract ,vitiligo, alopechia, uveitis, immune thyroid disease.
- 51. 51 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 S/SX: It is ionized calcium which under physiological regulation , is necessary for muscle contraction and nerve function. Hypocalcemia is a manifestation of reduced rate of bone resorption in the absence of sufficient PTH. Ca in blood Neuro excitibility and Tetany Ca in ECF Affect the neuromuscular and cardiovascular sites. It can manifested acutely as a medical emergency or chronic cold case. Hypocalcemic tetany is manifested by: 1. Numbness and tingling in the fingers and toes and around the lips 2. Laryngeal stridor with crowing inspiration. 3. Dyspnea and cyanosis. ACUTE HYPOCALCEMIA TINGLING OF THE FINGERS CHEVOSTEK’S, TROUSSEAU’S In sever tetany , cramps of individual muscle groups occurs in the hands and feet as carpopedal spasm.
- 52. 52 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 There may be convulsions , abdominal pain , nausea and vomiting. The seizures are of : Grand mal type/ no aura / no loss of consciousness /no incontinence& trauma Epileptiform attacks are striking and frequently described symptoms of hypocalcemia. CHRONIC HYPOCALCEMIA Mental abnormalities IRRITIBILITY & CONFUSION PERSONALITY CHANGES EMOTIONAL LIABILITY- DEPRESION MEMORY IMPAIREMENT.
- 53. 53 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Papilloedema and increase intracranial pressure may accompany it. CARDIAC ARRHYTHMIA FATIGUE, WEAKNESS CATARACT Cataract is a characterized consequence of chronic hypoparathyrodism. Ectopic calcifications –lens, subcutaneous tissues, thickened calvarium. XRAY: INCREASED BONE DENSITY In idiopathic hypoparathyrodism, Abnormalities of ectoderm- nails ,teeth , hairs , dry scaly coarse skin Blunting of roots of teeth and dysplasia of tooth enamel Nails- malformed ,brittle, transverse grooves D/D OF TETANY: 1.HYPOCALCEMIA: Ca Po4 PH Hypovitamniosis D N Resistance vit D N Malabsorption N hypoparathyroism N 2.Metabolic alkalosis----normal CA, PO4 , INCRESED PTH Persistent vomiting Hypokalemic alkalosis Excessive alkali treatment
- 54. 54 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 CRF over correction of acidosis Hypokalemic alkalosis(( hyperaldosteronism/ corticosteroid analogue)) 3. K Deficiency 4. MG Deficiency D/D OF HYPOCALCEMIA: 1. Hypocalcemia – hypercalciuria 2. Acute pancreatitis 3. Osteoblastic metastases-----prostate, breast 4. Chemotherapy for leukemia and lymphoma. LABORATORY: Ca in blood and urine Blood phosphate Phosphate clearance 1. SERUM CALCIUM: low 9mg/dl S.Ca is largely bound to albumin. The depressed level of S.Ca must be correlated with the simultaneous concentration of serum albumin. Low albumin ==== S.Ca is depressed. (0.8—1 mg of Ca to 1gm of albumin). Corrected S.Ca = S.Ca mg/dl + (0.8 X{4---ALBUMINg/dl}) Urine Ca approaches zero as the conc. Of Ca in blood less than 7mg/100ml. 2.SERUM CA low, SERUM PO4 high, ALP normal Why increased phosphate? B/C lack of hormone effect on phosphate clearance by the kidney. The rate of excretion of urinary excretion of 3 5 AMP is reduced.
- 55. 55 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 3.SERUM MG --low Hypomagnesemia reduces both PTH RELEASE AND TISSUE RESPONSIVNESS TO PTH---------HYPOCALCEMIA. 4. ECG-prolonged QT + T wave abnormalities. 5. SLIT LAMP EXAMINATION ---post. Lenticular cataract 6. IMAGING-----CT scan of skull ----basal ganglia calcification Bones denser than normal Spine showed the presence of lines parallel to the cortex of the vertebral bodies giving rise to an image of a small copy of the vertebral body within the body, a sign called “bone within a bone”.
- 56. 56 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 COMPLICATION: 1) Acute tetany with stridor 2) Ossifications of paravertebral ligaments 3) Convulsions 4) Parkinsonism symptoms 5) Treatment related – nephrocalcinosis and CRF D/D OF HYPOCALCEMIA: I. Decrease intake or absorption: 1.Malabsorption—no diarrhea 2.Small bowel bypass, short bowel 3. VIT D deficiency - absorption , 25 hydroxycolecalciferol II. Loss 1.Alcoholim
- 57. 57 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 2.Chronic renal insufficiency 3.Diuretic III. Endocrine disease 1.Hypoparathyrodism 2.Sepsis 3.Pseudohypoparathyrodism IV. Physiological 1.Decrease albumin 2.Decrease end organresponse to VIT D 3.Indued by loop diuretic,aminoglycoside, plicamycin D/D OF HYPOPARATHYRODISM: V. Ideopathic epilepsy VI. Choreoathetosis VII. Asthma VIII. Brain tumors( convulsion and calcifications) MANAGEMENT: 10% 20 - 30 ml 500- 1500 N/S VIT D 50,000—10,000U daily by mouth 1---2 gm Ca by mouth Ca SUPPLEMENT Ca carbonate (40%Ca) 500mg/ 5 times a day Ca salts should be given orally as soon as possible to supply 1-2 gm Ca/d. VIT D SUPPLEMENT – LIQ FORM: WITH WATER, JUICE OR MILK. Should be started as soon as oral Ca started.
- 58. 58 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Treatment of choice for chronic hypocalcemia is VIT D. Ergocalciferol—250,000-150,000U/D, slow acting Toxicity takes weeks to disappear (6-18weeks). Gives more stable serum Ca level. Dihdrotachysterol—faster in onset, 3 times more potent Daily dose 0.125—1mg/d , expensive Calcitriol (1, 5 DHCC)- RAPID , HIGH COST , TOXICITY 2 WKS USED IN ACUTE HYPOCALCEMIA 4 MICOGM/D Calcifedrol—intermediate onset and duration of action 20mico/d SEIZURE LISTEN FOR STRIDOR OR HOARSENESS TRACHEOSTOMY SET AT BEDSIDE CaGLUCONATE AT BEDSIDE HYPERPARATHYROIDISM Increase PTH production. Hypercalcemia with Hypophosphatemia. Age-50year, sex- 3times in female more than male PRIMARY – adenoma OR hyperplasia or CA of the parathyroid gland. Can be familial 5%( hyperplasia or adenoma) Multiple endocrine neoplasia MEN I IIA IIB
- 59. 59 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 SECONDARY – compensatory over secretion of PTH in response to hypocalcemia from : CHRONIC RENAL DISEASE RICKETS MALABSORPTION SYNDROME OSTEOMALACIA TERTIARY-enlarged gland and become autonomus CRF-----bone disease ---renal dystrophy. PHYSIOLOGY OF PTH: 1. Renal tubule reabsorption of CA 2. Inhibits the net absorption of PO4 &HCO3 by renal tubule. 3. Stimulate the synthesis of 1,25 DHCC by the kidney. 4. Cause excretion of CA and PO4 by the kidney PATHOLOGY OF INCREASED PTH: 1. Calculus formation within urinary tract- 5% of renal stones. 2. Diffuse parenchymal calcification (Nephrocalcinosis). 3. Osteoclastic activity in bone and increase CA delivery may produce diffuse demineralization and pathological fractures cystic bone lesions throughout the skeleton ===Osteitis fibrosa cystic D/D OF HYPERCALCEMIA: I. Intake or absorption a. Milk alkali syndrome b. VIT D or A excess – 25 HCC helpful to confirm DX. II. Endocrine disorders 1.HPT (1RY OR 2RY) 2.Acromegally
- 60. 60 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 3.Adisson disease. 4.Hyperthyrodism III. Neoplastic diseases a. Tumor secreting PTH related proteins(ovary, kidney, lung) b. Metastases to bone (breast ) c. Multiple myeloma ,leukemia ,lymphoma d. Secretions of PG and osteolytic factors. IV. Miscellaneous 1. Thiazide 2. Sarcoidosis 3. Pagets disease 4. Immobilization 5. Hypophosphatasia 6. Acute ill patient (ICU) 7. Renal transplant 8. Familial hypocalcemic hypocalcinuria Leprosy , Tuberculosis, Berylliosis, Cocidomycosis, Histoplasmosis. 1,25Dihydrocholecalciferol---------CA S/SX: Most patients are asymptomatic. Hypercalcemia is usually discovered accidently by blood biochemistry. Nodules are almost never palpable. Polyuria and constipation are the most characteristic symptoms. 1. Skeletal manifestation: 1-4%of patients Osteitis fibrosa cystic may cause brown tumors. Cysts of the jaw. Pathological fractures -back. Patients have bone pain, arthralgia ,diminished bone density (hip/radius).
- 61. 61 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 2.Urinary tract manifestation Polyuria and polydypsia may be present and due to increased CA Kidney stones are seen in 18% of pts Nephrocalcinosis Renal failure 2. Hypercalcemic manifestation Sever cases Thirst SOME PATIENT PRESENT W NEUROMUSCULAR Polyuria muscle weakness Anorexia easy fatigability Nausea parasthesia Vomiting depression Constipation sleeping tendency Anemia pruritis Weight loss psychosis HTN coma CARDIAC ARRHYTHMIAS, HTN XRAY: BONE DEMINERALIZATION IMAGING: I - To localize the gland: Preoperative processes unsuccessful B/C so small 1 cm 1. USS neck 2. CT scan neck 3. MRI NECK 4. T C- 99m seastamibi 5. Thallium/technetium subtraction scan ii- Angiography and selective venous sampling of PTH
- 62. 62 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 iii- Bone x rays are normal and not required to make diagnosis. There may be Demineralization Subperiosteal resoption of bone (radial aspects of fingers) Loss of lamina dura of teeth Pathological fracture Mottling of the skull(salt and pepper appearance). Chondrocalcinosis(articular cartilage calcification). Iv- patient with renal osteodystrophy: Have ectopic calcifications around joints and soft tissues. Dissiminated calcification in the X ray changes Skin, soft tissues , arteries Osteopenia Osteitis fibrosa Calciphylaxis Osteosclerosis
- 63. 63 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 Painful ischemic necrosis Osteosclerosis of the vertebral Of skin and gangrene bodies is called Cardiac arrhythmia RUGGER JERSEY SPINE Respiratory failure Ca may precipitate in the cornea(band keratopathy) & soft tissues(calciphylaxis) COMPLICATIONS OF HYPERCALCEMIA: 1. Peptic ulcer 2. Pancreatitis 3. Coma 4. Azotemia 5. Arrhythmia 6. Fractures Laboratory: The hall mark of hypercalcemia is s.ca more than 10.5mg/dl In hyperproteinemic state, total s.ca may be increased but ionized ca normal where as in 1ry HPT , ionized calcium increased. S O4 is often low 2.5 Urinary ca excretion may be high or normal (250mg/g creatinine) An excessive loss of phosphate in urine In 2ry HPT, s po4 is high. ALP is elevated only if bone disease is present. Plasma CL and uric acid levels may be elevated. Elevated levels of PTH confirm the diagnosis. Assay ---- immune radiometric assay (IRMA).
- 64. 64 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 ECG----short QT SUMMARY: S.Ca , Urinary Ca, CL & Uric acid, Urinary PO4, S.PO4 and PTH. MANAGEMENT: TX OF CHOICE : SURGICAL REMOVAL OF HYERPLASTIC TISSUE INDICATIONS- 1. S.Ca 1mg above upper limit of normal / U.Ca excretion more than 50mg/24hr. 2.U.Ca excretion 400mg/24hr 3.Cortical bone density 2SD below normal 4.Relative youth 30-60year 5.Symptomatic HPT 6.Difficult follow up After surgery,pt. may develop parasthesia ,tetany as a result of rapid fall of blood calcium .(although sCa normal). So, frequent periodic monitoring of Ca and albumin recommended. S.PTH postoperatively misleading//Transient thyrotoxicosis may occure. MEDICAL TREATMENT: Intensive hydration with normal saline. Bisphonates-Pamidronate , Alendronate 30-90mg/o.9N/S over 4-12 hours Preparing for surgery. Estrogen replacement—postmenopausal Avoid digoxin and give propranolol Glucocorticoid is ineffective. Renal osteodystrophy –avoid hyperphosphatemia—Ca acetate &calcitriol
- 65. 65 MAGDI AWAD SASI THYROID AND PARATHYROID DISORDERS 2013 LOW Ca, HIGH Ph DIET NO MILK, CAULIFLOWER & MOLASSES STRAIN URINE FOR STONES TO AVOID 1. Immobilization 2. Thiazid 3. VIT A/D 4. Ca. antaacids CARE FOR PARATHYROIDECTOMY FOLLOW UP: CA, ALBUMIN---twice yearly RFT +U.Ca--------once yearly BONE DENSITY---1-2year FAMILIAL HYPOCALCIURIC HYPERCALCMIA: Autosomal dominant Characterized by 1. Decrease urine CA 50 micro/24hr 2.Variable increase MG 3. Minimal PTH increase DX family history + urinary Ca clearance No surgery Excellent prognosis
