Disorders of Purine Metabolism Lecture
- 1. Disorders of Purine Metabolism Lecturer: Dr. G. K. Maiyoh Department of Medical Biochemistry, School of Medicine, MU March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 1
- 2. Overview • Introduction • Purine (types) • Purine functions • Sources of purines • Metabolic disorders • Nucleotide degradation • Uric acid and hyperuricemia • In-born errors of Uric acid metabolism • Disorders due to purine catabolism • Disorders due to salvage pathway March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 2
- 3. WHAT ARE PURINES? • Purines are heterocyclic compound consisting of a pyrimidine ring fused to an imidazole Ring March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 3
- 4. Purines • Other minor purine base include: 1. Xanthine 2. Hypoxanthine 3. Uric acid • The above occur in free state in the cells 4 N6 –Methyladenine 5 N6 N6 Dimethyladenine 6 N7-Methylguanine • Occur in mamalian RNA March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 4
- 5. PURINES 7 1,3-Dimethylxanthine(theophylline) found in TEA 8 3,7-Dimethylxanthine(theobromine)found in COCOA 9 1,3,7-Trimethylxanthine(caffiene ) found in coffee This are pharmacologically important March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 5
- 6. Functions Key functions include; Provision of Energy e.g. ATP, GTP Building blocks for DNA and RNA (along side pyrimidines) Basic conenzymes i.e. NAD and NADH Play role in signal transduction e.g GTP, cAMP, cGMP March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 6
- 7. Sources of purine ENDOGENOUS • They may be synthesized DE NOVO from small molecules EXOGENOUS • They may be derived from the breakdown of ingested nucleic acid,mostly from cell-rich meat • Plant diets generally poor in purines March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 7
- 8. Metabolic disorders of purines • They cover a broad spectrum of illnesses with various presentations. Examples of presentations include; • Hyperuricemia • Acute renal failure • Gout • Unexplained neurologic defects (seizures, muscle weakness e.tc) • Developmental disorders • Compulsive self injury and aggression • Immune deficiency • Deafness March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 8
- 9. Major Categories of Disorders Two major types of disorders occur; i. Those that arise from a Blockage in purine nucleotide degradation pathway ii. Arising from increased activity of nucleotide degradation pathway March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 9
- 10. Nucleotide degradation • Nucleic acids can survive the acid of the stomach • They are degraded into nucleotides by pancreatic nucleases and intestinal phosphodiesterases in the duodenum. • Components cannot pass through cell membranes, so they are further hydrolyzed to nucleosides. • Nucleosides may be directly absorbed by the intestine or undergo further degradation to free bases and ribose or ribose-1-phosphate by nucleosidases and nucloside phosphorylase. nucleosidase Nucleoside + H2O Nucleoside base + ribose phosphorylase Nucleoside + Pi base + ribose-1-P
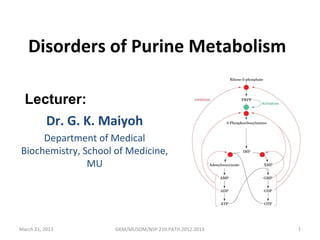
- 11. Catabolism of purines ADA Major pathways of purine catabolism in animals. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 11
- 12. Catabolism of purines •Purine nucleotide degradation refers to a regulated series of reactions by which purine ribonucleotides and deoxyribonucleotides are degraded to uric acid in humans. •As indicated earlier, two major types of disorders occur in this pathway; • A block of degradation occurs with syndromes involving;- • immune deficiency. •myopathy or •renal calculi. •Increased degradation of nucleotides occurs with syndromes characterized by;- • hyperuricemia and gout, •renal calculi, •anemia or acute hypoxia. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 12
- 13. Uric Acid (2,6,8-trioxypurine) • This is the end product of purine metabolism in humans • Accumulation of uric acid in blood is reffered to as hyperuricemia • Uric acid is highly insoluble therefore a very slight alteration in the production or solubility will increase levels in blood. • Due to poor solubility, levels in blood are usually near the maximal tolerable limits March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 13
- 14. Excretion of uric acid • Uric acid is filtered through the glomeruli and most is reabsorbed in the proximal tubules. • More than 80% of uric acid formed in the urine is derived from distal tubular secretion • Urinary excretion is slightly lower in males than females,which may contribute to the higher incidence of hyperuricaemia in men • Renal secretion may be enhanced by uricosonic drugs(e.g probenecid or sulfinpyrazone),which block tubular urate reabsorption
- 15. Excretion of uric acid • 75% urate leaving the body is in urine • The remaining 25% passes into the intestinal lumen,where it is broken down by intestinal bacteria(URICOLYCIS)
- 16. HYPERURICAEMIA • This is increase in blood levels of uric acid that is greater than 0.42 mmol/l in men and more than 0.36mmol/l in women • It can occur by two mechanisms: • 1 Increased production(Over Production) • 2 Decreased Excretion (under excretors)
- 17. Conditions that lead to Increased Uric acid Production – Malignancies – Reyes Syndrome – Downs Syndrome – Sickle cell anemia – Glycogen storage diseases types I,III, IV and V – Hereditary fructose intolerance – Gout – AcylCoA dehydroginase defficiency March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 17
- 18. Factors contributing to Hyperuraecimia • Increased synthesis of purines(primary Gout) • Secondary GOUT (Other disorder in which there is rapid tissue break down or rapid cellular turnover) • Increase intake of purines • Increase turnover of Nucleic Acids • Increased rate of urate formation • Reduced rate of Excretion
- 19. Factors contributing to Hyperuraecimia • Sex(plasma uric acid is higher in male than females) • Obesity (Obese people tends to high plasma level of urate) • Diet (subject with high protein diet ,which is also rich in NUCLIEC acids and who do have high alcohol consumption have high levels of plasma urate • Genetic factor(These are very important factor in high plasma urate levels)
- 20. Other causes may include: • Eclampsia • Lead toxicity • Chronic alcohol ingestion • NOTE Hypouricaemia is not an important chemical disorder in itself
- 21. Management of disorders Management of disorders of purine nucleotide degradation is dependent upon modifying the specific molecular pathology underlying each disease state. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 21
- 22. Common treatment for gout: allopurinol Allopurinol is an analogue of hypoxanthine that strongly inhibits xanthine oxidase. Xanthine and hypoxanthine, which are soluble, are accumulated and excreted. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 22
- 23. In born errors of Uric Acid Metabolism 1. Phosphorybosylpyrophosphate synthase (PRS) superactivity There are two form; i. The severe form which appears in infancy ii. The mild form which presents in adolescence • In both forms, kidney or bladder stone is often the first symptom. • Gout and impairment of kidney function may develop if the condition is not adequately controlled with medication and dietary restrictions. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 23
- 24. 2. Adenylosuccinase deficiency • Due to lack of the enzyme adenylosuccinate lyase • In general, affected individuals may have a mix of neurological symptoms, which usually includes abnormalities with cognition and movement, autistic features, epilepsy, muscle wasting, and feeding problems. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 24
- 25. Disorders due to purine catabolism March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 25
- 26. Myoadenylate Deaminase Deficiency • Also called muscle adenosine monophosphate deaminase deficiency • This is a genetic disease that interferes with the muscle cell's processing of ATP, the key energy molecule of a cell. • The lack of an enzyme that converts ATP to inosine and ammonia may present no symptoms or it may cause exercise-induced cramping. • The disorder is diagnosed through the accumulation of ammonia or inosine monophosphate in muscle tissue • Treatment typically consists of exercise modulation. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 26
- 27. Xanthine Oxidase Deficiency (XANTHINURIA) • This is a rare hereditary disorder in which there is a deficiency of liver xanthine oxidase • The catabolism of purine stops with xanthine- hypoxanthine stones. • The blood uric acid is very low and there is a high level of urinary excretion of xanthine • There is reduced excretion of urinary uric acid
- 28. Xanthine Oxidase Deficiency (Xanthinuria) •Xanthine oxidase deficiency, is an inherited metabolic disorder in which there is deficiency of an enzyme needed to process xanthine, a substance found in caffeine and related substances. •If left untreated, xanthinuria can lead to kidney stone formation and subsequent urinary tract diseases. •Additionally, this condition can lead to muscle disorders, due to deposits of xanthine in muscle tissue. •Treatment of the condition involves avoiding foods and drinks that contain xanthine derivatives, such as coffee, tea and colas and maintaining a high fluid 28 March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013
- 29. Adenosine Deaminase Deficiency • This is a genetic disorder that impairs the immune system and is the basis of severe combined immunodeficiency, or SCID. • Children diagnosed with SCID are typically deficient in almost all immune protection from pathogens and are vulnerable to chronic infections caused by "opportunistic" organisms that ordinarily do not cause disease in healthy people with a normal immune response. • Symptoms of SCID include pneumonia and chronic diarrhea, with impeded growth compared to healthy children. • Additionally, neurological problems such as developmentalGKM/MUSOM/NSPmotor function disorders and March 21, 2013 delay, 210:PATH.2012.2013 29
- 30. Disorders due to salvage pathway A salvage pathway is a pathway in which nucleotides (Purine and pyrimidine) are synthesized from intermediates in the degradative pathway for nucleotides. There are two critical enzyme defficiencies; I. Hypoxanthine guanige phosphorybosyltransferase (HPRT) defficiency – May be total (Lesch-Nyhan syndrome ) or partal defficiency Partial HPRT-deficient patients present with symptoms similar to total but with a reduced intensity, and in the least severe forms symptoms may be unapparent. I. Adenine phosphorybosyltransferase (APRT) defficiency – The disorder results in accumulation of the insoluble Purine 2,8- dihydroxyadenine. – It can result in nephrolithiasis (kidney stones), acute renal failure March 21, 2013and permanent kidney damage. GKM/MUSOM/NSP 210:PATH.2012.2013 30
- 31. Lesch-Nyhan Syndrome • Lesch-Nyhan syndrome is a metabolic disorder caused by a deficiency of an enzyme (HPRT) produced by mutations in a gene located on the X chromosome. • The disease is marked by a buildup of uric acid in all body fluids that results in conditions known as hyperuricemia and hyperuricosuria. • Symptoms often include severe gout, impaired muscular control, moderate mental retardation and kidney problems. • These complications frequently emerge in the first year of life. Neurological symptoms can include March 21, 2013 grimacing, GKM/MUSOM/NSP 210:PATH.2012.2013 facial involuntary writhing and repetitive31
- 32. Gout • Characterised by the accumulation of monosodium urate crystal deposits which result in inflamation in joints and surrounding tissues. • Presentation – Hyperuricemia – Uric acid nephrolithiasis – Acute inflamatory arthritis March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 32
- 33. Gout • Commonly monoarticular (Affecting the metatarsophalangeal joint of the big toe. • However deposits of sodium urates may aslo occur in; – The elbows – Knees – Feet – Helix of the ear March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 33
- 34. Figure 28-29 The Gout, a cartoon by James Gilroy (1799). Page 1097 Gout is a disease characterized by elevated levels of uric acid in body fluids. Caused by deposition of nearly insoluble crystals of sodium urate or uric acid. March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 34
- 35. Types of Gout • Primary Gout – Occurrence: Middle aged men (mostly) – Cause: Overproduction of Uric Acid Decreased renal excretion or both Biochemical Etiology: Not clearly known and is considered a polygenic disease March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 35
- 36. Types of Gout • Secondary Gout – Occurrence: Children – Cause: other condition in which there is rapid tissue breakdown or cellular turnover – Such condition leads to either; • Increased production of Uric acid • Decreased clearance of Uric acid March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 36
- 37. Other conditions that could lead to gout • Any other condition that may lead to either; – Decreased uric acid clearance or – Increase in production These may include; Also; • Malignancy therapy •Excessive purine intake •Alcohol intake • Dehydration •Carbohydrate ingestion • Lactic acidosis • Ketoacidosis • Stavation • Diuretic therapy • Renal failure March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 37
- 38. Hereditary disorders associated with gout • These include 3 key enzymes resulting in hyperuricemia • These are; 1. Severe HPRT defficiency (Lesch-Nyhan syndrome) • Also Partial HPRT defficiency 1. Superactivity of PP-ribose-p synthetase 2. Glucose -6-phosphatase defficiency (glycogen storage disease type 1) March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 38
- 39. Hereditary disorders associated with gout - cnt • 1st two are caused by hyperuricemia due to purine nucleotide and uric acid overproduction • The 3rd due to excess uric acid production and impaired uric acid secretion March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 39
- 40. Familial Juvenile Gout (Familial Juvenile Hyperuricemic Nephropathy (FJHN) • Due to severe renal hypoexcretion of uric acid • Presentation usually occurs at puberty to the 3rd decade – Has also been reported in infancy Characteristics – Hyperuricemia – Gout – Familial renal disease – Low urate clearance relative to GFR March 21, 2013 GKM/MUSOM/NSP 210:PATH.2012.2013 40
