Urinary Tract Infection in Pregnancy.pptx
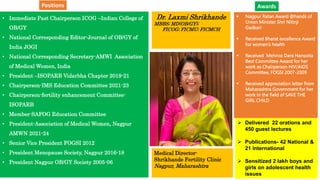
- 1. • Immediate Past Chairperson ICOG –Indian College of OB/GY • National Corresponding Editor-Journal of OB/GY of India JOGI • National Corresponding Secretary-AMWI Association of Medical Women, India • President –ISOPARB Vidarbha Chapter 2019-21 • Chairperson-IMS Education Committee 2021-23 • Chairperson-fertility enhancement Committee- ISOPARB • Member-SAFOG Education Committee • President-Association of Medical Women, Nagpur AMWN 2021-24 • Senior Vice President FOGSI 2012 • President Menopause Society, Nagpur 2016-18 • President Nagpur OB/GY Society 2005-06 Dr. Laxmi Shrikhande MBBS; MD(OB/GY); FICOG; FICMU; FICMCH Medical Director- Shrikhande Fertility Clinic Nagpur, Maharashtra Nagpur Ratan Award @hands of Union Minister Shri Nitinji Gadkari Received Bharat excellence Award for women’s health Received Mehroo Dara Hansotia Best Committee Award for her work as Chairperson HIV/AIDS Committee, FOGSI 2007-2009 Received appreciation letter from Maharashtra Government for her work in the field of SAVE THE GIRL CHILD Delivered 22 orations and 450 guest lectures Publications- 42 National & 21 International Sensitized 2 lakh boys and girls on adolescent health issues Awards Positions
- 2. UTI in Pregnancy Dr Laxmi Shrikhande Senior Consultant- Shrikhande Fertility Clinic Nagpur, Maharashtra
- 3. Definition of Urinary tract infection UTI is defined as the presence of at least 100,000 organisms per milliliter of urine in an asymptomatic patient, or as more than 100 organisms/mL of urine with accompanying pyuria (> 7 white blood cells [WBCs]/mL) in a symptomatic patient. A diagnosis of UTI should be supported by a positive culture for a uropathogen, particularly in patients with vague symptoms.
- 5. Classification of UTI’s Clinical: • Asymptomatic (8%) • Symptomatic (1-2%) Anatomical: • Lower tract : asymptomatic bacteriuria and acute cystitis • Upper tract : acute pyelonephritis
- 6. Definition of Asymptomatic bacteriuria Asymptomatic bacteriuria is commonly defined as the presence of more than 100,000 organisms/mL in 2 consecutive urine samples in the absence of declared symptoms. Untreated asymptomatic bacteriuria is a risk factor for acute cystitis (40%) and pyelonephritis (25-30%) in pregnancy. This usually occurs in early pregnancy. Risk factors include prior UTIs, pre-existing diabetes, increased parity, and low socioeconomic status.
- 7. Definition of Cystitis Acute cystitis involves only the lower urinary tract; it is characterized by inflammation of the bladder as a result of bacterial or nonbacterial causes.. Acute cystitis develops in approximately 1- 2% of pregnant patients, of whom 60% have a negative result on initial screening. Signs and symptoms include haematuria, dysuria, suprapubic discomfort, frequency, urgency, and nocturia. These symptoms are often difficult to distinguish from those due to pregnancy itself. Acute cystitis is complicated by upper urinary tract disease (ie, pyelonephritis) in 15-50% of cases.
- 8. Acute pyelonephritis Pyelonephritis is the most common urinary tract complication in pregnant women, occurring in approximately 0.5-2% of all pregnancies. Acute pyelonephritis is characterized by fever, flank pain, and tenderness in addition to significant bacteriuria. Other symptoms may include nausea, vomiting, frequency, urgency, and dysuria. Most cases of pyelonephritis occur in the second and third trimester.
- 9. Types of UTI Recurrences Relapse: same organism within 2-3 wks secondary to perineal colonization or inadequate Rx Reinfection: new organism within 12 wks 2ndry to recurrent bladder bacteriuria Superinfection: new organism while on Rx Prevention: Prenatal screening for ASB in pregnant women
- 11. Etiology E coli is the most common cause of UTI, accounting for approximately 70-80% of cases in pregnancy. It originates from fecal flora colonizing the periurethral area, causing an ascending infection. Other pathogens include the following : Klebsiella pneumoniae (5%) Proteus mirabilis (5%) Enterobacter species (3%) Staphylococcus saprophyticus (3%) Group B beta-hemolytic Streptococcus (GBS; 2-5%) Proteus species (2%)
- 12. The differential diagnosis of UTI in pregnancy : Cervicitis Chlamydial Genitourinary Infections Nonbacterial and Noninfectious Cystitis Ectopic Pregnancy Interstitial Cystitis Nephrolithiasis Trichomoniasis Trigonitis Urethritis Vaginitis Vaginal infections can cause or mimic UTIs, which are common in women of reproductive age, affecting 25-35% of women aged 20-40 years. Discriminating between the 2 depends on the results of vaginal and urinary cultures.
- 13. Clinical Presentation-History The presentation varies according to whether the patient has asymptomatic bacteriuria, a lower urinary tract infection (UTI; ie, cystitis) or an upper UTI (ie, pyelonephritis). Burning with urination (dysuria) is the most significant symptom in pregnant women with symptomatic cystitis. Other symptoms include frequency, urgency, suprapubic pain, hematuria, and pyuria in the absence of systemic symptoms. The usual complaints of increased frequency, nocturia, and suprapubic pressure are not particularly helpful, because most pregnant women experience these as a result of increased pressure from the growing uterus, expanding blood volume, increased glomerular filtration rate, and increased renal blood flow. Pyelonephritis signs and symptoms often include fever (> 38°C), shaking chills, anorexia, nausea, vomiting, and costovertebral angle tenderness.
- 14. Physical Examination Physical examination findings should be considered in relation to the duration of pregnancy. The differential diagnoses may change from one trimester to the next, and the increasing size of the gravid uterus may mask or mimic disease findings. A thorough physical examination is recommended, with particular attention to the abdomen. Suprapubic or costovertebral tenderness may be present. In asymptomatic bacteriuria, no physical findings are typically present. Symptoms may arise intermittently, only to be overlooked because of lack of persistence or severity. Pelvic examination is recommended in all symptomatic patients (with the exception of third-trimester patients with bleeding) to rule out vaginitis or cervicitis. In patients with cystitis, tenderness can often be elicited with isolation of the bladder on pelvic examination. Patients with pyelonephritis have fever (usually > 38°C), flank tenderness upon palpation, and an ill appearance. Flank tenderness occurs on the right side more frequently, and is present in more than half of patients. Pain may also be found suprapubically with palpation. Assessment of the fetal heart rate on the basis of gestational age should be included as part of the evaluation. Often, owing to maternal fever, the fetal heart rate is elevated to more than 160 beats/min.
- 15. Workup Laboratory studies can include blood studies and urine studies, including culture, urinalysis, dipstick testing, and other tests (eg, urine cytology, sulfosalicylic acid [SSA] testing). Imaging tests can include ultrasonography and intravenous pyelography.
- 16. Blood Studies The following blood tests should be ordered at the physician’s discretion, though the results do not aid in the diagnosis or change treatment unless they are markedly abnormal: Complete blood count (CBC) Serum electrolytes Blood urea nitrogen (BUN) Serum creatinine In pregnant women who are showing signs of sepsis, it is reasonable to obtain blood cultures and a lactic acid assay. Although there is no evidence that positive blood cultures are associated with worse prognosis, elevated lactic acid levels have been associated with adverse maternal outcomes in presumed sepsis.
- 17. Urine culture Urine culture is the standard method for evaluating for urinary tract infection (UTI) during pregnancy. Indications for performing a urine culture include the following: New onset of symptoms of cystitis with positive urinalysis or dipstick testing Recurrent UTI Pyelonephritis Failure to respond to initial treatment regimens History of recent instrumentation Hospital admission A voided specimen with a bacterial growth of 100,000 colony-forming units (CFUs) per milliliter or higher is the standard definition of a positive urine culture. Counts lower than 100,000 CFU/mL usually indicate specimen contamination rather than infection. Patients with pyelonephritis often have white blood cell (WBC) casts. Culture results can be used to identify specific organisms and antibiotic sensitivities, but results are often unavailable at the time of treatment.
- 18. Urinalysis by microscopy Positive results for nitrites, leukocyte esterase, WBCs (pyuria), red blood cells (RBCs), and protein suggest UTI. Pyuria is present in almost all women with cystitis. Bacteria found in the specimen can help with the diagnosis. The presence of bacteria without pyuria usually represents contamination of the urine. Urinalysis has a specificity of 97-100%, but it has a sensitivity of only 25-67% when compared with culture in the diagnosis of asymptomatic bacteriuria. Clumping WBCs and WBC casts are indicative of kidney inflammation and are consistent with upper tract infection or pyelonephritis. RBC casts are characteristic of acute glomerulonephritis, which should be suspected after a recent or concurrent streptococcal infection. Renal involvement usually leads to proteinuria. Nephrotic syndrome includes high proteinuria (> 3.5 g/24 h), edema, hypercholesterolemia, and hypoalbuminemia; however, this can be confused with preeclampsia. Oval fat bodies and fatty casts can suggest membranous glomerulonephritis.
- 19. Dipstick testing Several reports describe the use of urine dip for nitrites and leukocyte esterase in the evaluation of asymptomatic bacteriuria. In comparison with culture, sensitivity ranges from 50% to 92% and specificity from 86% to 97%. In the evaluation of symptomatic patients, dipstick testing is useful and inexpensive. However, the leukocyte esterase test may be unreliable in patients with low-level pyuria (5-20 WBCs/HPF). The addition of protein and blood increases the sensitivity and specificity of the test in the evaluation of UTI. A positive nitrite test is reliable for bacteriuria, but a negative test does not exclude bacteriuria. The reason for this is that bacteria converts the dietary metabolite nitrate to nitrite in the urine. As suggested by Kodikara et al, nitrite dipstick testing may be a reasonable and cost-effective screening strategy for women who otherwise may not undergo screening for bacteriuria, as is often the case in developing countries.
- 20. Renal Ultrasonography and Intravenous Pyelography Unless an anatomic abnormality or renal disease is suspected, initial routine imaging studies are not necessary. Patients with suspected pyelonephritis who are not responsive to appropriate antibiotic therapy after 48- 72 hours should undergo imaging. In pregnant patients, the recommended imaging study to perform first is a renal ultrasound, to avoid contrast and radiation unless necessary. Renal ultrasound is helpful to visualize kidney or ureteral stones, renal abscess formation, or hydronephrosis. Renal ultrasonography (or limited intravenous pyelography [IVP] if the benefits of a definitive diagnosis outweigh the minor risk of radiation) may be helpful in patients with recurrent urinary tract infection (UTI) or symptoms that suggest nephrolithiasis . Confusion about the diagnosis of urolithiasis, pyelonephritis, or both is an indication for obtaining imaging studies.
- 21. Treatment of bacteriuria and cystitis Because of the dangers of maternal and fetal complications, acute care should focus on identifying and treating asymptomatic and symptomatic bacteriuria, along with ensuring that an alternative process is not the cause of the symptoms. Treatment of asymptomatic bacteriuria has been shown to reduce the incidence of low birth weight and preterm birth. Behavioral practices Any discussion of treatment should be prefaced with a discussion of behaviors that may be used to ensure good hygiene and reduce bacterial contamination of the urethral meatus, thereby preventing inadequate treatment and recurrent infection. Behavioral methods include the following: Wipe front-to-back after urinating or defecating Wash hands before using the toilet Use washcloths to clean the perineum Use liquid soap to prevent colonization from bar soap Clean the urethral meatus first when bathing
- 22. Antibiotic therapy Oral antibiotics are the treatment of choice for asymptomatic bacteriuria and cystitis. Treatment is most commonly initiated empirically before culture and susceptibility results return.
- 23. Treatment Regimens for Pregnant Women with Asymptomatic Bacteriuria or UTI Nitrofurantoin monohydrate/macrocrystals 100 mg orally twice daily for 5-7 days or Amoxicillin 875 mg orally twice daily (alternative: 500 mg orally three times daily) for 5-7 days or Amoxicillin-clavulanate 500/125 mg orally three times daily for 5-7 days (alternative: 875/125 mg orally two times daily for 5-7 days) or Cephalexin 500 mg orally four times daily for 5-7 days or Fosfomycin 3 g orally as a single dose with 3-4 oz. of water
- 24. Antibiotic therapy Although 1-, 3-, and 7-day antibiotic courses have been evaluated, 10-14 days of treatment is usually recommended to eradicate the offending bacteria. Treatment success depends on eradication of the bacteria rather than on the duration of therapy. A test-for-cure urine culture should show negative findings 1-2 weeks after completion of therapy. A nonnegative culture result is an indication for a 10- to 14-day course of a different antibiotic.
- 25. Antibiotic therapy Recurrent cystitis Pregnant women who have three or more episodes of cystitis or bacteriuria should be started on daily antibiotic prophylaxis for the remainder of pregnancy. Daily antibiotics should also be considered in pregnant women after one episode of pyelonephritis. Regimens for daily prophylaxis includes nitrofurantoin 100 mg nightly, or cephalexin 250-500 mg nightly. In patients who are immunosuppressed or have medical conditions that would increase the risk of complications from cystitis, it is reasonable to consider antibiotic prophylaxis after one episode of cystitis.
- 26. Treatment of pyelonephritis The standard course of treatment for pyelonephritis consists of hospital admission and intravenous (IV) administration of antibiotics until the patient has been afebrile for 48 hours. The recommended IV antibiotic would be a broad spectrum beta-lactam, such as ceftriaxone. Once culture results with susceptibilities become available and the patient is clinically improved, treatment can be transitioned to an oral antibiotic regimen. For women with a history of extended-spectrum beta-lactamase (ESBL) Enterobacter, a carbapenem is recommended. Patients should be discharged with 10-14 days of antibiotic treatment, and then will need daily prophylactic antibiotics for the remainder of pregnancy.
- 27. Treatment of pyelonephritis IV fluids must be administered with caution. Patients with pyelonephritis can become dehydrated because of nausea and vomiting and need IV hydration, but they are at high risk for the development of pulmonary edema and acute respiratory distress syndrome (ARDS). Fever should be managed with antipyretics (preferably, acetaminophen) and nausea and vomiting with antiemetics. If fever persists beyond 24 hours, urine and blood cultures should be repeated and a renal ultrasound should be performed. Preterm labor and delivery are additional risks associated with pyelonephritis. These risks must be evaluated and treated early in the course of admission with tocolysis as necessary per the preterm labor guidelines. If the patient is septic, tocolysis is not recommended.
- 28. Surgical treatment Surgical care is rarely indicated. Cystoscopy may aid in establishing the diagnosis of urethral or bladder diverticulum, bladder stones, urethral syndrome, lower urinary tract trauma, interstitial cystitis, or bladder cancer. A retrograde stent or a percutaneous nephrostomy tube should be placed to relieve ureteral colic or decompress an obstructed infected collecting system. More invasive procedures, such as ureteroscopic stone extraction, are rarely indicated. Extracorporeal shock wave lithotripsy (ESWL) is contraindicated in pregnancy. In the rare patient for whom invasive surgical therapy is indicated, the operation should be planned for the second trimester. Surgical intervention during the first trimester is associated with increased risk of miscarriage; surgery in the third trimester is associated with increased risk of preterm labor. Urgent surgical intervention in the third trimester should coincide with delivery of the fetus.
- 29. Obstetric management — Pyelonephritis is not itself an indication for delivery. If induction of labor or cesarean delivery for standard obstetrical indications is planned in a patient on treatment for pyelonephritis, wait until the patient is afebrile, as long as delaying the delivery is relatively safe for the mother and fetus. Since pyelonephritis is associated with preterm birth, an important obstetric consideration is whether tocolysis should be used when pyelonephritis triggers preterm labor at various gestational ages. Tocolysis is typically not administered after 34 weeks gestation. If a woman with pyelonephritis prior to that gestational age experiences preterm labor, administration of tocolysis and steroids is reasonable to attempt to prolong the pregnancy. However, if the patient is septic, tocolysis is generally avoided. Pregnant women with pyelonephritis are at increased risk of pulmonary edema and acute respiratory distress syndrome (ARDS), which may be exacerbated by administration of tocolysis with or without corticosteroids.
- 30. Preventing recurrence — Recurrent pyelonephritis during pregnancy occurs in 6 to 8 percent of women . As a result, after an initial episode of pyelonephritis, low-dose antimicrobial preventive therapy with an agent to which the original organism is susceptible for the remainder of the pregnancy is a reasonable strategy; but there are no randomized trials to inform the optimal approach. If preventive therapy is utilized, reasonable options include nitrofurantoin (50 to 100 mg orally at bedtime) or cephalexin (250 to 500 mg orally at bedtime) . For individuals who use preventive antibiotics following pyelonephritis, do not perform surveillance urine cultures to ensure effective prophylaxis.
- 31. Prevention in women with history of recurrent UTI A separate issue is the management of pregnant women with a history of recurrent urinary tract infections (UTIs) prior to pregnancy, which is often related to sexual intercourse. It is reasonable to use postcoital prophylaxis in pregnant women who have recurrent UTIs that appear to be temporally related to sexual intercourse. The preferred regimen is a single postcoital dose of either cephalexin (250 mg) or nitrofurantoin (50 mg).
- 32. Antibiotic safety in pregnancy Penicillins (with or without beta-lactamase inhibitors), cephalosporins, the carbapenems meropenem and ertapenem, aztreonam, and fosfomycin are generally considered safe in pregnancy . Nitrofurantoin is typically avoided during the first trimester because of uncertain associations with congenital anomalies , although overall evidence suggests it is a reasonable alternative during this period if other options cannot be used. Trimethoprim-sulfamethoxazole is also often avoided during the first trimester because of a potential association with congenital abnormalities and near term because of a theoretical risk of kernicterus ; however, it remains a reasonable alternative during these periods given the uncertainty of the evidence if other options cannot be used.
- 33. Antibiotic safety in pregnancy Aminoglycosides have been associated with ototoxicity following prolonged fetal exposure , and fluoroquinolones are generally not used during pregnancy. Much of the information regarding the safe use of antibiotics during pregnancy was obtained decades ago, before pregnant women were excluded from drug studies because of concerns about risk to the fetus. Thus, there is little direct information about the safety of many newer antibiotics (including many antibiotics that are used for UTI) in pregnancy, and concern about the use of certain antibiotics generally arises from indirect evidence (eg, animal studies) or observational studies that may have numerous confounders. Overall, the safest course is to use the antibiotics that have well-established safety profiles in pregnancy and limit the use of antibiotics of potential concern to cases in which no safer alternative exists.
- 34. Complications The primary complication of bacteriuria during pregnancy is cystitis, though the primary morbidity is due to pyelonephritis. Complications may include the following: Perinephric cellulitis and abscess Septic shock Renal dysfunction (usually transient, but as many as 25% of pregnant women with pyelonephritis have a decreased glomerular filtration rate) Hematologic dysfunction, including anemia or thrombocytopenia Hypoxic fetal events due to maternal complications of infection that lead to hypoperfusion of the placenta Preeclampsia Preterm labor, and possible subsequent preterm delivery, leading to increased infant morbidity and mortality Pregnant women with pyelonephritis can become critically ill very quickly. It has been estimated that approximately 20% of pregnant women with severe pyelonephritis develop complications that include septic shock variants. Pulmonary injury may also complicate UTI in pregnancy. Approximately 2% of women with severe pyelonephritis during pregnancy have evidence of pulmonary injury due to systemic inflammatory response syndrome and respiratory insufficiency. Endotoxins that alter alveolar-capillary membrane permeability are produced; subsequently, pulmonary edema and acute respiratory distress syndrome develop.
- 35. Prognosis In most cases of bacteriuria and urinary tract infection (UTI) in pregnancy, the prognosis is excellent. Maternal UTI has few direct fetal sequelae because fetal bloodstream infection is rare; however, uterine hypoperfusion due to maternal dehydration, maternal anemia, and direct bacterial endotoxin damage to the placental vasculature may cause fetal cerebral hypoperfusion. Untreated upper UTIs are associated with low birth weight, prematurity, premature labor, hypertension, preeclampsia, maternal anemia, and amnionitis. Preeclampsia- A meta-analysis of 19 studies demonstrated an increased odds (1.31-fold) of preeclampsia in women with any UTI during pregnancy versus those without UTI.
- 36. Summary and recommendations Asymptomatic bacteriuria • Screening – Screen all pregnant women at least once for asymptomatic bacteriuria. Screening for asymptomatic bacteriuria is performed at 12 to 16 weeks gestation with a midstream urine for culture. The diagnosis is made by finding high-level bacterial growth (≥105 colony-forming units [cfu]/mL) on urine culture in the absence of symptoms consistent with UTI. • Management – Management of asymptomatic bacteriuria in pregnant women includes antibiotic therapy tailored to culture results, which reduces the risk of subsequent pyelonephritis and is associated with improved pregnancy outcomes. Potential options include beta-lactams, nitrofurantoin, and fosfomycin . Do not routinely perform follow-up culture to rescreen for asymptomatic bacteriuria.
- 37. Summary and recommendations Cystitis (bladder infection) – Acute cystitis should be suspected in pregnant women who complain about new onset dysuria, frequency, or urgency. The diagnosis is made by finding of bacterial growth on urine culture in this setting. Management of acute cystitis in pregnant women includes empiric antibiotic therapy that is subsequently tailored to culture results. Potential options for empiric and directed therapy include beta- lactams, nitrofurantoin, and fosfomycin . Do not routinely perform follow-up culture to confirm sterilization of the urine. For those with recurrent cystitis, prophylactic or suppressive antibiotics may be warranted in addition to retreatment.
- 38. Summary and recommendations • Pyelonephritis • Clinical features and diagnosis – Acute pyelonephritis during pregnancy is suggested by the presence of flank pain, nausea/vomiting, fever (>38°C), and/or costovertebral angle tenderness, with or without the typical symptoms of cystitis, and is confirmed by the finding of bacteriuria in the setting of these symptoms. • Pregnant women may become quite ill and are at risk for both medical (eg, sepsis, respiratory failure) and obstetrical complications from pyelonephritis. • Management – Management of acute pyelonephritis in pregnant women includes hospital admission for parenteral antibiotics, preferably broad spectrum beta-lactams . • Antibiotic therapy can be converted to an oral regimen tailored to the susceptibility profile of the isolated organism following clinical improvement. Oral options are generally limited to beta-lactams or, if in the second trimester, trimethoprim-sulfamethoxazole. Following the treatment course, preventive antibiotics are a reasonable strategy for the remainder of the pregnancy to prevent recurrence.
- 39. Summary and recommendations • Antibiotic safety – It is generally accepted that penicillins (with or without beta-lactamase inhibitors), cephalosporins, aztreonam, and fosfomycin are safe in pregnancy. • Because of possible but uncertain associations with adverse birth outcomes, avoid nitrofurantoin during the first trimester and trimethoprim-sulfamethoxazole during the first trimester and near term, but they are appropriate alternatives during those periods if other options cannot be used.
- 40. for your attention and dedication towards women health
- 41. My World of sharing happiness! Shrikhande Fertility Clinic Ph- 91 8805577600 / 8805677600 shrikhandedrlaxmi@gmail.com
- 42. The Art of Living Anything that helps you to become unconditionally happy and loving is what is called spirituality. H. H. Sri Sri Ravishakar
