Update of hie treatment
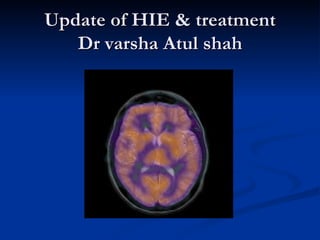
- 1. Update of HIE & treatment Dr varsha Atul shah
- 2. Definition Neonatal encephalopathy due to hypoxic-ischemic brain injury. 1-2 cases in 1000 births Many causes Different severity levels Moderate encephalopathy carries a 10% mortality and 30% risk of severe disability for survivors Severe encephalopathy carries a 60% mortality with nearly 100% severe neurological morbidity in survivors
- 3. Causes of asphyxia Metabolic Infections Structural brain anomalies Intracranial hemorrhage Maternal toxins Interruption of umbilical circulation Inadequate placental circulation Impaired fetal or maternal circulation Impaired maternal oxygenation
- 4. Pathology Severity and distribution is dependent on several factors Certain vulnerable areas - cerebral cortex , hippocampus , basal ganglia, thalamus, brain stem, subcortical and periventricular white matter In full term infants gray matter structures affected and in premature infants white matter Four basic and clinically important lesions - Neuronal necrosis, status marmoratus, para-sagittal cerebral injury, periventricular leucomalacia
- 5. Overview of the pathogenesis Evolving process - Brain injury after experimental HI insult is an evolving process. The nature and severity of the injury dictates the magnitude of the initial damage. Latent phase - After the initial reperfusion period, brain oxidative metabolism often recovers partially or completely Delayed phase of injury - an ominous phase of secondary deterioration following the latent phase - during which neurons and oligodendroglia continue to die for longer periods.
- 6. The processes of cell injury and death during the initial HI insult appear to be a predictable phenomenon: - deprivation of oxygen and nutrients leads to a shift to anaerobic glycolysis - depletion of high-energy phosphate reserves - loss of cell membrane functions, - accumulation of lactic acid, calcium, free radicals and neurotoxic, excitatory neurotransmitters such as glutamate in the extracellular milieu - deterioration of cell function If the insult is not interrupted, this cascade ultimately leads to acute or “primary” cell death.
- 7. However, the biochemical processes involved in evolving cell death that develops after reperfusion are more complex. A series of interrelated mechanisms may be responsible for perpetuating the initial injury, some of which include the following: - cytosolic accumulations of calcium and exposure to free radicals, including formation of nitric oxide, - injury from inflammatory mediators - mitochondrial dysfunction. These and other processes trigger apoptotic pathways contributing to continued neuronal and oligodendroglial injury and death - may evolve over hours, days, or possibly weeks and months after an HI injury.
- 8. Although the sequence of evolution of the phases of energy failure and cellular damage and dysfunction after HI injury are strikingly consistent across animal species and among subjects, the duration of these phases (especially that of the latent and secondary deterioration) and the degree of continuing damage can vary considerably. The factors that might affect the length of the reperfusion and latent phases of injury are not well known but likely include the following: - the nature, magnitude, and the pattern or repetition of the initial HI insult - the maturational stage of the brain - the subject’s general health and nutritional status - regional cerebral blood flow and metabolic characteristics
- 10. HI damage caused an inciting event leads to a cascade of disturbances the foremost of which is neuronal energy failure and loss of endothelial integrity. Loss of ATP dependant ion pumps leads to increase cellular sodium and calcium which in turn leads to edema and neuronal lysis. Build up of intracellular calcium leads to glutamate release and neuronal excitation which may progress to seizure activity and also causes the release of lipase, proteases and endonucleases that contribute to free radical formation and cellular death. The release of nitric oxide and subsequent free radical formation causes lipid peroxidation and loss of cellular integrity. It also cause increased release of glutamate and thereby further incites excitotoxity caused by this neurotransmitter.
- 11. Prognosis based on Apgars Score at 1, 5 minutes does not give prognosis indicator The longer the score remains lower, the greater its significance 0-3 @ 1min has mortality of 5-10% may be increased to 53% if at 20min apgars score 0-3 0-3 @ 5min , CP risk app. 1% may be increased to 9%if for 15min dramatic rise to 57% CP risk if for 20min
- 12. Newborn neurological assessment Staging system of Sarnat and Sarnat Means of recording severity of insult to brain, to initiate med management and to predict ultimate prognosis Infants occasionally sustain insult to brain arising from complication of systemic disease Seizures in 50-70%
- 14. Mild HIE Muscle tone may be increased slightly Deep tendon reflexes may be brisk during the first few days. Transient behavioral abnormalities, such as poor feeding, irritability, or excessive crying or sleepiness, may be observed. By 3-4 days of life, the CNS examination findings become normal.
- 15. Moderate HIE Lethargic, significant hypotonia Diminished deep tendon reflexes. Grasp, Moro, and sucking reflexes may be sluggish or absent. Occasional periods of apnea. Seizures may occur within the 1st 24 hours of life. Full recovery within 1-2 weeks is possible and is associated with a better long-term outcome.
- 16. Severe HIE Stupor or coma is typical. may not respond to any physical stimulus. Breathing may be irregular, and the infant often requires ventilatory support. Generalized hypotonia and depressed deep tendon reflexes are common. Neonatal reflexes (e.g., sucking, swallowing, grasping, Moro) are absent. Disturbances of ocular motion, such as a skewed deviation of the eyes, nystagmus, bobbing, and loss of "doll's eye" (i.e., conjugate) movements may be revealed by cranial nerve examination. Pupils may be dilated, fixed, or poorly reactive to light.
- 17. Seizures occur early and often, may be initially resistant to conventional treatments. The seizures are usually generalized, and their frequency may increase during the 2-3 days after onset, correlating with the phase of reperfusion injury. As the injury progresses, seizures subside and the EEG becomes isoelectric or shows a burst suppression pattern. At that time, wakefulness may deteriorate further, and the fontanel may bulge, suggesting increasing cerebral edema. Irregularities of heart rate and BP are common during the period of reperfusion injury, as is death from cardiorespiratory failure
- 18. Intervention Brain injury begins with the hypoxic-ischemic event and evolves after resuscitation interval of several hours after resuscitation when therapies might be applied to lessen the severity of the evolving brain damage. HIE is a progressive syndrome Initially show transient recovery with a secondary failure of cerebral energy metabolism 6-15 hours after birth. The severity of this second deterioration is highly predictive of neurodevelopmental outcome at 1-4 years of age.
- 19. Therapies, to be effective, must be applied in this latent phase of the disease in order to modulate long term outcome
- 20. Management Prevention, prevention, prevention !!! Ensure physiological oxygen & CO2 levels - hyperoxia causes ↓ in CBF or exacerbate free radical damage - hypercapnia causes cerebral vasodilation - hypocapnia can decrease CBF Acid-base balance Maintain environmental temp and humidity Correct caloric, fluid and electrolyte disturbances - watch for hypoglycemia & hypocalcemia Seizures - treated with phenobarb, phenytoin or lorazepam
- 21. Newer modalities Antagonists of excitotoxic neurotransmitter receptors - NMDA receptor blockers Free radical inhibitors / scavengers - vitamin E, superoxide dismutase Ca channel blockers Nitric oxide synthetase inhibitors Hypothermia
- 23. Hypothermia as a Treatment for HIE Studies have shown that hypoxic ischemic injury can be reduced by brain cooling. Favorable effect on many of the pathways contributing to brain injury Excitatory amino acids Cerebral energy state Cerebral blood flow and metabolism Nitric oxide production Apoptosis
- 24. Mechanism of Action Hypothermia modulates all these areas in the cascade of Hypothermia acts to: neuronal damage and death - Block NMDA activation - Decrease neurotransmitter release - Limit formation and activity of nitric oxide - Decrease depletion of ATP stores * N-methyl-D-aspartic acid
- 28. Cooling for newborns with hypoxic ischaemic encephalopathy The standard search strategy of the Neonatal Review Group as outlined in the Cochrane Library (Issue 2, 2003) was used. Randomised controlled trials evaluating therapeutic hypothermia in term newborns with hypoxic ischaemic encephalopathy were identified by searching the Oxford Database of Perinatal Trials, the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library Issue Issue 2, 2003), MEDLINE (1966 to July 2003), previous reviews including cross-references, abstracts, conferences, symposia proceedings, expert informants and journal hand searching.
- 29. Selection criteria Randomised controlled trials comparing the use of therapeutic hypothermia with normothermia in encephalopathic newborn infants with evidence of peripartum asphyxia and without recognisable major congenital anomalies were included. The primary outcome measure was death or long-term major neurodevelopmental disability. Other outcomes included adverse effects of cooling and 'early' indicators of neurodevelopmental outcome.
- 30. Main results Two randomised controlled trials were included in this review, comprising 50 term infants with moderate/ severe encephalopathy and evidence of intrapartum asphyxia. There was no significant effect of therapeutic hypothermia on the combined outcome of death or major neurodevelopmental disability in survivors followed. No adverse effects of hypothermia on short term medical outcomes or on some 'early' indicators of neurodevelopmental outcome were detected.
- 31. Data collection & analysis Three reviewers independently selected, assessed the quality of and extracted data from the included studies. Authors were contacted for further information. Meta-analyses were performed using relative risk and risk difference for dichotomous data, and weighted mean difference for continuous data with 95% confidence intervals.
- 32. Reviewers' conclusions Although two small randomised controlled trials demonstrated neither evidence of benefit or harm, current evidence is inadequate to assess either safety or efficacy of therapeutic hypothermia in newborn infants with hypoxic ischaemic encephalopathy. Therapeutic hypothermia for encephalopathic asphyxiated newborn infants should be further evaluated in well designed randomised controlled trials.
- 34. Hypothermia and perinatal asphyxia: Executive summary of the National Institute of Child Health and Human Journal of Pediatrics. Vol 148 (2). Feb 2006 Development (NICHD) workshop
- 35. NICHD held a workshop on hypothermia as a potential treatment modality for perinatal hypoxic- ischemic encephalopathy (HIE) in May 2005. A panel of experts summarized the current evidence on the efficacy and safety of hypothermia and reviewed knowledge gaps. The panel concluded that mild, therapeutic hypothermia offered a potential for short-term benefits (up to 18 months of age) when used under strict experimental protocols in term infants. However, these findings have not been tested in preterm infants or severely growth-restricted infants with asphyxia. Many questions still remained about the optimal use of hypothermia for HIE in term infants, including the incidence of possible rare, short-, and long-term side effects.
- 36. The longer-term benefits in neurodevelopmental outcomes after hypothermia for HIE remain to be shown. Because of these and other reasons, the panel concluded that at the current time, therapeutic hypothermia for perinatal HIE should be considered an evolving therapy, the longer-term safety and efficacy of which are still to be established. The panel offered a framework for patient care emphasizing the need for standardized protocols for treatment and follow-up, including school-age outcome assessments. Research priorities were also recommended. The panel strongly urged that the ongoing hypothermia trials should be continued to enable assessment of its efficacy and safety. It recommended the formation of national and international HIE registries, so that scientific progress in this field can be assessed continuously to develop,
- 37. Hypothermia & Neuroprotection Studies in fetal sheep, neonatal piglets, rat, and other models showed that: - brain cooling to about 32° and 34° C beginning 90 minutes or 5.5 hours after HI injury - continuing for 48 to 72 hours - diminished the extent of parasagittal neuronal damage (the effect of cooling was observed in other regions of brain as well). Improved neurologic outcomes were confirmed by use of quantitative neuropathologic methods, imaging studies, and tests of learning and memory functions.
- 38. Conclusions from the animal studies Brain cooling should be initiated as early as feasible after the brain injury, preferably within 2 hours, but not later than 6 hours Rectal temperature should be reduced to between 32° to 34° C for effective brain cooling with whole-body hypothermia Smaller reductions in rectal temperature (34°-35° C) may be needed for head cooling Cooling should be continued for about 48 to 72 hours Slow rewarming optimal methods for rewarming were not tested in newborn animals, adult animal studies indicated that slow rewarming was to be preferred.
- 39. Translating the results of animal studies to human trials Many limitations had to be noted before extrapolating the potentially beneficial effects seen in animal models of HIE and hypothermia to human HIE. In human beings, HIE is not a single disease entity, but a condition resulting from diverse causes manifesting signs of brain injury at different phases of its evolution. The cause(s) of HIE is rarely obvious, and the timing, nature, or severity of the HI injury is almost never known.
- 40. The underlying status of the human brain, such as its maturity, nutritional and hormonal status, inflammatory, and preexisting developmental abnormalities may alter the responses to acute insults. Moreover, one can only offer therapy for HIE in human infants at a known postnatal age - not after a known interval from brain injury. However, in only about 25% of HIE cases can one discern signs of a sentinel event in the peripartum period indicating the time of injury. There is considerable variability in the neuronal (and other brain cellular) responses to HI injury and to hypothermia among the experimental species, and in human infants. Thus one cannot determine with precision how late after an ischemic injury one can provide cooling and
- 41. Initial Pilot Trials In 1955, Westin et al showed that hypothermia was beneficial in perinatal asphyxia. However, systematic pilot studies were not done until Gunn et al, Azzopardi et al, and Thoresen and Whitelaw described simple approaches to cooling the head and the whole body for up to 72 hours without serious, short-term adverse effects. Findings from these studies showed that although bradycardia occurred commonly, other acute complications, such as severe hypotension, acute deterioration in pulmonary function, increased rates of infection, or imbalances in blood viscosity, electrolytes, and clotting did not occur with mild therapeutic hypothermia for 72 hours. Shankaran et al also confirmed the feasibility of providing whole-body cooling for 72 hours without
- 42. In a pilot study of whole-body cooling to a rectal temperature of 33° ± 0.5° C for 48 hours in infants with severe HIE, Eicher et al reported a higher incidence of bradycardia and a greater use of inotropic agents during cooling in the hypothermia group (n = 33) compared with in the control subjects (n = 32). The hypothermia group also had longer prothrombin times and lower platelet counts than the control subjects, but all of the values were within normal range. Thus the cumulative evidence from numerous animal studies and the reassuring conclusions about the short-term safety and feasibility of providing therapeutic hypothermia in human infants led to the development of larger randomized controlled trials.
- 43. Hypothermia for Neonates with Hypoxic-Ischemic Encephalopathy Versus Whole Body Hypothermia Selective Head Cooling
- 44. What’s the difference? The brain can be cooled by cooling the body, cooling the head selectively, or cooling the head and body together. The majority of studies in animals have used whole-body cooling, but some have used selective head cooling. Whole-body cooling provides homogeneous cooling to all brain structures, including peripheral and central brain regions. Selective head cooling provides greater cooling to the periphery of the brain than to the central brain structures Head cooling combined with some body cooling minimizes temperature gradients across the brain and facilitates the cooling of central regions. Given the propensity for hypoxic–ischemic injury to affect deep- brain structures such as the thalamus, internal capsule, and basal ganglia in the human neonate, whole-body cooling may achieve a consistent reduction in brain temperature in such structures.
- 45. Large Scale Clinical Trials First completed multicenter trial (CoolCap) conducted in 25 centers in New Zealand, Great Britain, and the United States 234 infants with acute perinatal HIE were enrolled Criteria for entry: >36 weeks gestation an Apgar score <5 at 10 minutes after birth or a continued need for resuscitation at 10 minutes after birth or a pH <7.0 or base deficit > 16 mmol/L in the umbilical blood or venous blood sample within 60 minutes of birth and a modified Sarnat score and amplitude-integrated EEG (aEEG) criteria consistent with a diagnosis of moderate to severe HIE
- 46. CoolCap Infants in the experimental group (n = 116) received selective head cooling with mild systemic hypothermia induced with a cooling cap device in which cold water was circulated. The rectal temperature was maintained between 34° to 35° C for 72 hours, and the infants were rewarmed at a rate <0.5° C per hour. Conventional intensive care with normal body temperature was provided for infants in the control
- 47. CoolCap - Results Children followed-up for 18 months 50% of cooled infants had unfavorable primary outcomes (death or severe neurologic disability) while 2/3 of control group had unfavorable outcomes. Overall no statistically significant improvement between cooled group and control, however… When controlling for most severely effected it was found that selective head cooling of those with moderate HIE there was a significant difference between the study group and the controls. The collaborative group suggested that selective head cooling of those infants with moderate HIE was likely to be beneficial in the reduction of
- 48. Second large randomised controlled clinical trial - Whole-Body Hypothermia Shankaran et al
- 49. 208 infants from 16 Neonatal Research Network centers randomized within 6 hours after birth Infants in hypothermia group placed on 2 cooling blankets and esophageal temperatures were kept at 33.5o C for 72 hours. Eligibility criteria included: gestational age ≥ 36 weeks, a pH of 7.0 or less or a base deficit of 16 mmol/L or more in a sample of umbilical cord blood or any blood during the first hour after birth. If, during this interval, pH was between 7.01 and 7.15, a base deficit was between 10 and 15.9 mmol/L, or a blood gas level was not available, additional criteria were required. These included an acute perinatal event and either a 10-minute Apgar score of 5 or less or assisted ventilation initiated at birth
- 50. Same eligibility criteria were used for this study as the cool cap study, however no AEEG was used. All surviving infants were followed up between 18-22 months of age with developmental assessments. Growth, vision, and hearing characteristics were obtained and neurologic and developmental testing was performed. Cognitive outcome was assessed with the use of Bayley scales of infantile development. Significant differences were not found in rates of mental retardation, blindness, hearing deficits, or cerebral palsy. This evidence suggests that hypothermia did not cause an increased rate disability amongst survivors.
- 51. Death or moderate/severe disability occurred in: 44% (45/102) of the hypothermia group 62% (64/103) of the control group Mortality rate 24% in the hypothermia group 37% in the control group For the hypothermia group versus the control group, respectively the risk of disabling cerebral palsy was 19.2% and 30.0% blindness 7% versus 14% hearing impairment requiring a hearing aid was 4% and 6% The frequency of adverse event rates during cooling was similar: 19% in the hypothermia group 15% in the control group
- 52. OTHER ONGOING TRIALS TOBY ICE
- 53. Total Body Cooling Trial (TOBY) England Infants with moderate-to-severe HIE are randomized to receive whole-body cooling or standard intensive care. Thus far, 206 of the planned 239 (86%) infants (as of January 26, 2006) have been enrolled, and the study is continuing. The trial design features and the entry criteria for the TOBY trial are similar to those of the CoolCap trial. Thus, upon completion, the findings from the TOBY trial can be effectively compared with those of CoolCap to assess the relative benefits from whole-body versus selective head cooling in HIE. Such comparisons would be of great value, since these trials will constitute 2 of the largest cohorts of infants
- 54. ICE (Infant Cooling Evaluation) 15 participating centers in Australia, New Zealand, and Canada in this ongoing trial. The trial aims to enroll infants from a wide geographic region, using simplified protocols. Hypothermia is achieved by turning off the ambient heating systems and by applying “Hot-Cold” gel packs (at 10° C) around the infant’s head and over the chest, so that the rectal temperature is reduced to 33° to 34° C. After demonstrating the feasibility of this approach in 17 infants, the investigators have enrolled 96 of the planned 276 infants from
- 55. Major Gaps in Knowledge In spite of rapidly accumulating clinical and laboratory data related to hypothermia as a neuroprotective strategy for HIE, the speakers and discussants at the workshop underscored numerous gaps in knowledge in this field. They noted that with only 2 completed studies providing information on follow-up for only up to 18 months of age, the longer-term impact of hypothermia for HIE remains unknown. This, they concluded, should lead to an overall measure of caution in applying the new therapy of hypothermia indiscriminately for all cases of HIE.
- 56. Is It Safe? No significant differences in adverse events between control and hypothermic infants in either large trial. More studies need to be conducted before widespread applicability and safety can be ascertained.
- 57. Late at night, and without permission, Reuben would often enter the nursery and perform experiments in static electricity.
- 58. Adverse effects Electrolyte & Renal Dysfunction metabolic derangements metabolic acidosis Renal dysfunction Cardiac adverse events Bradycardia Significantly lower mean blood pressures Cardiac echocardiograms indicated worsening right ventricular function in two hypothermia patients. Greater and longer cardiac inotropic support was required in the hypothermia group compared with the normothermia group
- 59. Coagulopathy & Thrombocytopenia required plasma and platelet transfusions than normothermia patients Mean lowest platelet counts were significantly lower in the hypothermia group The median highest prothrombin time values were significantly higher in the hypothermia group However, clinical manifestations of coagulopathy were uncommon.
- 60. Pulmonary Hypertension Pulmonary vascular resistance has been demonstrated to be increased with hypothermia, but may also be present under normothermic conditions after hypoxic-ischemia. Although pulmonary vascular resistance cannot be measured directly in neonates, nitric oxide treatment and extracorporeal membrane oxygenation are surrogate measures of the severity of pulmonary hypertension Significantly more hypothermia patients required nitric oxide than normothermia patients, but only one normothermic patient required extracorporeal membrane oxygenation as an adverse event
- 61. Other Significant Adverse Events Seizures significantly more common in the hypothermia group as an adverse event than in the normothermia group For this variable, all infants who had not seized before or during enrollment were considered to have the adverse event of seizures, which were largely clinically identified, as continuous electroencephalographic recording was not routinely performed. There was also a trend toward more abnormal electroencephalograms at 72 hours in the hypothermia group Stridor more common, perhaps related to reduced ventilator temperature of humidified air. This condition may have increased the transient tracheal swelling after extubation, but stridor was quickly dispelled with inhalation of racemic epinephrine, and no infant
- 62. Moderate hypothermia in neonatal encephalopathy: Safety outcomes Pediatric Neurology, Vol 32 (1) January 2005
- 63. Multicenter, randomized, controlled pilot trial of moderate systemic hypothermia (33°C) vs normothermia (37°C) for 48 hours in infants with neonatal encephalopathy instituted within 6 hours of birth or hypoxic-ischemic event. A total of 32 hypothermia and 33 normothermia neonates were enrolled in seven centers. Adverse events observed were significantly more commonly in the hypothermia group: more frequent bradycardia and lower heart rates during the period of hypothermia longer dependence on pressors higher prothrombin times lower platelet counts with more patients requiring plasma and platelet transfusions. Seizures as an adverse event were more common in the hypothermia group.
- 65. 1. Implementing hypothermia for HIE lacks long term safety and efficacy data (at the present time) Institutions choosing to offer hypothermia should implement studied and reported protocols from existing or ongoing trials, and incorporate longer-term follow up plans. knowledge gaps, uncertain longer term outcome parents of infants with HIE offered hypothermia should be appropriately appraised National and international registries need to be organized for ongoing assessment of the global burden of HIE, its treatment and outcomes. International interest groups of scientists, practitioners, and others involved in public policy need to be formed for continued evaluation of accumulating evidence Countries with limited resources the role of therapeutic hypothermia in HIE for children born in these countries needs to be studied in the context of regional issues of
- 66. 2. Identification of infants for offering hypothermia Value of standardized clinical examinations, scoring systems (e.g., modified Sarnat score), and aEEG should be studied to assess eligibility for hypothermia. Hypothermia in premature infants, severe IUGR infants has not been studied. although it has been tested in term infants and to a lesser extent in late preterm, (>35 weeks gestation) infants The risk benefit ratio for these infants cannot be assessed at this time due to lack of data. The severity of HIE at which the risk versus benefit ratio favors hypothermia remains unknown. whether developmental outcomes are affected by the type and timing of HI injury needs to be studied. “how late is not too late” the latest postnatal age at which initiation of therapeutic hypothermia might still be effective is unknown.
- 67. 3. Cooling and rewarming Optimal degree and duration of cooling is unknown although it is postulated that deeper, longer, and earlier therapy with hypothermia is to be preferred whether the degree and duration of therapy should be based on the cause, severity, stage of brain injury, and the age at starting of hypothermia is unknown. Optimal mode of cooling (whole body or selective head) is unknown, differential protective effects on various regions of the brain (generalized cortical versus deep brain nuclei), has not been established. optimal/safe pace of re-warming is unknown. The frequency of uncommon and rare systemic side effects, and the method of monitoring for these need to be studied
- 68. 4. Long-term outcome Role of MRI or other anatomic or functional imaging modalities in prognosis and during follow-up remains to be studied. Assessing outcome duration of follow-up and the appropriate tests to assess outcome should be similar so that outcomes under differing protocols can be compared. Longer-term follow-up of infants who participated in the completed and ongoing and future hypothermia trials should be strongly supported.
- 69. So should we be using it? Pediatrics Vol. 117 No. 3 March 2006 The Committee on Fetus and Newborn concluded that: Therapeutic hypothermia should be considered investigational until the short-term safety and efficacy have been confirmed. Long-term safety and efficacy remain to be defined. Additional trials are needed that would define the most effective cooling strategies. Registries of infants with perinatal encephalopathies should be established to facilitate data collection regarding diagnoses, treatments, and outcomes. Longer-term follow-up at least through early school age is essential
- 70. Summary & Conclusions Based on the available data and large knowledge gaps, hypothermia appears to be a potentially promising therapy for HIE, long-term efficacy and safety are yet to be established. Clinicians choosing to offer this treatment should therefore understand all of the limitations of the available evidence, be prepared to keep up-to-date on evidence on this topic as it evolves, and counsel parents and family about the limitations of the current evidence.
- 71. Thank You!
- 72. with mild systemic hypothermia after neonatal encephalopathy: multicentreVol 147 No. 1 July 2005 Journal of Pediatrics randomised trial
- 73. Objective To determine the efficacy of selective head cooling with mild systemic hypothermia on survival free of severe disability at 18 months of age in newborn infants with moderate or severe hypoxic-ischemic encephalopathy. Design Multi-center, international, unmasked, randomized controlled trial. Setting Twenty-five perinatal centers in the United States, United Kingdom, New Zealand, and Canada Enrolled term newborn infants of at least 36 weeks gestation (n=234) with clinical evidence of moderate to severe neonatal encephalopathy (based on modified Sarnat criteria) and/or seizures, and clinical evidence of perinatal hypoxia-ischemia (Apgar score of 5 or less at 10 minutes, continued resuscitation or respiratory support at 10 minutes, or severe acidosis within one hour of birth) and with moderately or severely abnormal background activity or seizures on amplitude integrated electroencephalography (aEEG). Interventions Infants were randomly assigned within 6 hours of birth to either head cooling (cooling cap with water circulated at 8-12°C [Olympic Medical Cool Care System]) with concomitant mild systemic hypothermia (rectal temperature 34-35°C) for 72 hours, or to conventional care (rectal temperature 36.8-37.2°C). Main Outcome Primary outcome was death or severe disability at 18 months of age. Secondary outcomes consisted of potential adverse effects of cooling and complications of hypoxia-ischemia including death, arrhythmia, coagulopathy,
- 74. Results Baseline clinical and aEEG characteristics were similar in the two groups. In the 218 (93%) infants followed to 18 months, there was no significant difference in the primary outcome of death or severe disability in the infants treated with hypothermia (unadjusted: 55% vs 66%, P=0.10, OR 0.61 [95% CI 0.34-1.09]; adjusted [for baseline aEEG amplitude, presence of seizures, and age at randomization]: P=0.05, OR 0.57 [95% CI 0.32-1.01]), or on any secondary outcome measures. Two predefined subgroup analyses based on pre-randomization background aEEG amplitude abnormalities demonstrated: a) no apparent effect of delayed cerebral hypothermia on outcome in infants with severe aEEG abnormalities (n=46: 79% vs 68%, P=0.51, OR 1.8 [95% CI 0.49-6.4]), and b) benefit in infants with intermediate (moderate) aEEG abnormalities (n=172: 48% vs 58%, P=0.021, OR 0.47 [95% CI 0.26-0.87]; adjusted P=0.009, OR 0.42 [95% CI 0.22-0.88]) and the number needed to treat was six infants (95% CI 3-27). Conclusions Selective head cooling with mild systemic hypothermia is a feasible therapeutic maneuver without clear-cut evidence of benefit in selected infants with moderate or severe hypoxic-ischemic encephalopathy. It may, however, improve the outcome for encephalopathic newborn infants with intermediate (moderate) abnormality on aEEG background amplitude.
- 75. Treatment of Term Infants With Head Cooling and Mild Systemic Hypothermia (35.0°C and 34.5°C) PEDIATRICS Vol. 111 No.Asphyxia After Perinatal 2 February 2003
- 76. Modest Hypothermia as a Neuroprotective Strategy in High-Risk Term Infants Clinics in Perinatology Volume 33 • Number 1 • March 2006
- 77. Hypothermia: A Neuroprotective Therapy for Neonatal Hypoxic-Ischemic Encephalopathy PEDIATRICS Vol. 117 No. 3 March 2006, pp. 942-948
- 78. Selective Head Cooling in Newborn Infants After Perinatal Asphyxia: Pediatrics Vol. 102 (4) October 1998 A Safety Study University of Auckland, Auckland, New Zealand.
- 79. Study group infants 37 weeks' gestation, who had an umbilical artery pH 7.09 or Apgars 6 at 5 minutes, plus evidence of encephalopathy. Infants were randomized to either: no cooling (controls; rectal temperature = 37.0 ± 0.2°C, n = 10) or sequentially, either minimal systemic cooling (rectal temperature = 36.3 ± 0.2°C, n = 6) or mild systemic cooling (rectal temperature = 35.7 ± 0.2°C, n = 6). Head cooling was accomplished by circulating water at 10°C through a coil of tubing wrapped around the head for up to 72 hours. All infants were warmed by servo-controlled overhead heaters to maintain the allocated rectal temperature. The rectal, fontanelle, and nasopharyngeal
- 80. No adverse effects because of cooling were observed. No infants developed cardiac arrhythmias, hypotension, or bradycardia during cooling. Thrombocytopenia occurred in 2 out of 10 controls, 2 out of 6 minimal cooling infants, and 1 out of 6 mild cooling infants. Hypoglycemia (glucose <2.6 mM) was seen on at least one occasion in 2 out of 10 controls, 4 out of 6 minimal cooling infants, and 1 out of 6 mild cooling infants. Acute renal failure occurred in all infants. The metabolic acidosis present in all infants at the time of enrollment into the study progressively resolved despite cooling, even in the mild hypothermia group.
- 81. Moderate hypothermia in neonatal encephalopathy: Efficacy outcomes Pediatric Neurology Vol 32 (1) January 2005
- 82. Multicenter, randomized, controlled, pilot trial of moderate systemic hypothermia (33°C) vs normothermia (37°C) for 48 hours in neonates initiated within 6 hours of birth or hypoxic- ischemic event. The trial tested the ability to initiate systemic hypothermia in outlying hospitals and participating tertiary care centers, and determined the incidence of adverse neurologic outcomes of death and developmental scores at 12 months by Bayley II or Vineland tests between normothermic and hypothermic groups.
- 83. Thirty-two hypothermic and 33 normothermic neonates were enrolled. The entry criteria selected a severely affected group of neonates, with 77% Sarnat stage III Ten hypothermia (10/32, 31%) and 14 normothermia (14/33, 42%) patients expired Controlling for treatment group, outborn infants were significantly more likely to die than hypoxic-ischemic infants born in participating tertiary care centers Severely abnormal motor scores (Psychomotor Development Index < 70) were recorded in 64% of normothermia patients and in 24% of hypothermia patients. The combined outcome of death or severe motor scores yielded fewer bad outcomes in the hypothermia group (52%) than the normothermia group (84%) Although these results need to be validated in a large clinical trial, this pilot trial provides important data for clinical trial design of hypothermia treatment in neonatal hypoxic-ischemic injury.
- 84. Improvement in the most serious outcomes of death or severe motor scores at 12 months of age. Severely abnormal motor outcomes alone were decreased in the hypothermia group compared with the normothermia group, even with the predominantly Sarnat stage III neonates, who were expected to be less responsive to treatment. Cognitive scores in this pilot trial did not seem as sensitive to hypothermia treatment effects as motor scores. The incidence of death and severe motor scores at 12 months in this pilot trial indicate that hypothermia may be helpful even in severe neonatal hypoxic-ischemic injury. The efficacy, optimal length of hypothermia therapy, and an assessment of the risk-benefit of hypothermia will be determined in future clinical trials. The favorable results of this pilot trial offer important considerations for the design of hypothermia trials in neonatal hypoxic-ischemic injury.
- 85. Whole-Body Hypothermia for Neonates with Hypoxic– Ischemic Encephalopathy NEJM Oct 05, Vol 353(15): 1574-1584
- 86. Randomized trial of hypothermia in infants with: a gestational age of at least 36 weeks who were admitted to the hospital at or before six hours of age with either severe acidosis or perinatal complications and resuscitation at birth and who had moderate or severe encephalopathy. Infants were randomly assigned to usual care (control group) or whole-body cooling to an esophageal temperature of 33.5°C for 72 hours, followed by slow rewarming (hypothermia group). Neurodevelopmental outcome was assessed at 18 to 22 months of age.
- 87. Of 239 eligible infants, 102 were assigned to the hypothermia group and 106 to the control group. Adverse events were similar in the two groups during the 72 hours of cooling. Primary outcome data were available for 205 infants. Death or moderate or severe disability occurred in 45 of 102 infants (44%) in the hypothermia group and 64 of 103 infants (62%) in the control group Twenty-four infants (24%) in the hypothermia group and 38 (3%) in the control group died There was no increase in major disability among survivors; the rate of cerebral palsy was 15 of 77 (19%) in the hypothermia group as compared with 19 of 64 (30%) in the control group Whole-body hypothermia reduces the risk of death or disability in infants with moderate or severe hypoxic–ischemic encephalopathy.
- 88. A concern with any therapy that reduces mortality among infants at high risk of death and disability is the possibility of an increase in the number of infants who survive with disabilities. In this study, there was no evidence of increased rates of moderate or severe disability at 18 to 22 months of age among infants treated with hypothermia. The rates of disabling cerebral palsy were: 19 percent in the hypothermia group 30 percent in the control group, The rates of a Mental Development Index below 70 were: 25 percent in the hypothermia group
- 89. Neurodevelopmental Outcome of Infants Treated With Head Cooling and Mild Hypothermia After Pediatrics Vol. 107 (3) March 2001 National Women's Hospital & Perinatal Asphyxia University of Auckland, Auckland, New Zealand.
- 90. Infants 37 weeks' gestation, who had an umbilical artery pH 7.09 or Apgar score 6 at 5 minutes, plus clinical encephalopathy. Infants with major congenital abnormalities were excluded. Infants were allocated to either: no cooling (rectal temperature = 37.0 ± 0.2°C, n = 15) or, sequentially, to head cooling accompanied by different levels of systemic hypothermia, including minimal cooling, rectal temperature 36.5°C to 36°C (n = 6) and mild cooling, to either 35.9°C to 35.5°C (n = 6) 35 ± 0.5°C (n = 6) or 34.5 ± 0.5°C (n = 7) Head cooling was accomplished by circulating cooled water through a coil of tubing wrapped around the head for up to 72 hours. Survivors were followed up with regular neurologic examination by a neonatologist until 18 months of
- 91. Results A total of 40 term infants were enrolled from 2 to 5 hours after birth. The control and the cooled groups were not significantly different for gestation, birth weight, Apgar score, and initial pH. There were 6 early neonatal deaths (3 normothermic and 3 cooled), and 1 death in infancy associated with severe spastic cerebral palsy in a normothermic infant. Six normothermic, 1 minimally cooled, and 4 mildly cooled infants had early stage 1 encephalopathy; all but 1 had a good outcome. Among infants with early stage 2 or 3 encephalopathy, an adverse outcome was found in 4 of 9 normothermic infants (44%) and 4 of 5 minimally cooled infants (80%), whereas in the combined mildly cooled groups, an adverse outcome was found in 4 of 15 infants (26%, odds ratio 0.46 [0.08, 2.56] vs normothermia).
- 92. Conclusions The present study supports the safety of hypothermia, with no evidence of late adverse effects in any infant. Among infants with moderate to severe encephalopathy at enrollment, there was a tendency toward better outcome. These results emphasize the relatively wide range of outcomes using purely clinical criteria for enrollment. Therapeutic hypothermia should not be used outside of stringent, multicenter trials.
Notes de l'éditeur
- Adverse reactions to cooling might be – Cardiac arrhythmia, major venous thrombosis, severe hypotension despite maximal support, abnormal renal function, coagulopathy, electrolyte imbalance, bone marrow depression,increased LFT’s, metabolic acidosis
- If therapeutic hypothermia is to be implemented outside of an RCT, clinicians should follow published protocols, ensure systematic follow-up of survivors validated neurodevelopmental tests, and submit patient data to national or international registries as they are established. Parents should be informed of the current status of hypothermia therapy and consent for the procedure obtained.