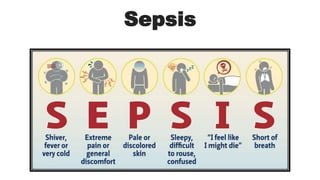
Sepsis
- 1. Sepsis
- 2. 1. Early sepsis a. Infection and Bacteremia b. Identification of Early sepsis (qSOFA, NEWS) 2. Sepsis 3. Septic shock 4. Others 1. Multiple organ dysfunction syndrome (MODS) 2. Systemic inflammatory response syndrome (SIRS) Sepsis
- 3. 1- Early sepsis Infection and bacteremia may be early forms of infection that can progress to sepsis. No formal definition of early sepsis. Despite the lack of definition, monitoring those suspected of having sepsis is critical for its Prevention.
- 4. 1- Early sepsis a. Infection and Bacteraemia All patients with infection or bacteraemia are at risk of developing sepsis and represent early phases in the continuum of sepsis severity: 1. Infection is defined as the invasion of normally sterile tissue by pathogenic microorganisms that proliferate, resulting in tissue injury that can progress to disease. 2. Bacteremia is the presence of viable
- 5. 1- Early Sepsis b. Identification of early sepsis (qSOFA, NEWS) Societal guidelines place emphasis on the early identification of infected patients who may go on to develop sepsis as a way to decrease sepsis-associated mortality. The two most commonly used scores are : 1. The quick Sequential (Sepsis-related) Organ Failure Assessment score (qSOFA) score 2. The National Early Warning Score (NEWS) score.
- 6. 1- Early Sepsis b.Identification of early sepsis (qSOFA, NEWS) 1. qSOFA score is easy to calculate since it only has three components, each of which are readily identifiable at the bedside and are allocated one point: 1. Respiratory rate ≥22/minute 2. Altered mentation 3. Systolic blood pressure ≤100 mmHg This qSOFA score is a modified version of the SOFA score. A score ≥2 is associated with poor outcomes due to sepsis.
- 7. 1- Early Sepsis 2. NEWS score is an aggregate scoring system derived from six physiologic parameters: 1. Respiration rate 2. Oxygen saturation 3. Systolic blood pressure 4. Pulse rate 5. Level of consciousness or new confusion 6. Temperature The aggregate score represents the risk of death from sepsis and indicates the urgency of the response: 1. 0 to 4 – low risk (a score of 3 in any individual parameter is low-medium) 2. 5 to 6 – medium risk 3. 7 or more – high risk
- 8. Sepsis is a clinical syndrome that has physiologic, biologic, and biochemical abnormalities caused by a dysregulated host response to infection. Sepsis and the inflammatory response that ensues can lead to multiple organ dysfunction syndrome 2- Sepsis 1. Early sepsis a. Infection and bacteremia b. Identification of early sepsis (qSOFA, NEWS) 2. Sepsis 3. Septic shock 4. Others 1. Multiple organ dysfunction syndrome 2. Systemic inflammatory response syndrome
- 9. 2- Sepsis • A 2016 SCCM/ESICM task force has defined sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection (Sepsis-3):
- 10. Pathogenesis of sepsis (a) Sepsis is defined as a dysregulated host response to infection, leading to life-threatening organ dysfunction. (b) Once a pathogen has succeeded to cross the mucosal barrier of the host, it can cause sepsis depending on its load and virulence. (c) Sepsis is by definition a disease with organ failure. The clinical manifestation can be heterogeneous.
- 11. Sepsis exists on a continuum of severity ranging from infection and bacteraemia to sepsis and septic shock, which can lead to MODS and death.
- 12. A clinical syndrome characterized by systemic inflammation caused by infection. In the USA, over 1.6 million cases of Sepsis occur every year, with a mortality rate of 20– 50%. Mortality of Septic Shock is 40– 50%.
- 13. The definitions of Sepsis and Septic Shock have rapidly evolved since the early 1990s
- 14. The SIRS is no longer included in the definition since it is not always caused by infection.
- 15. The Center for Medicare and Medicaid Services (CMS) still continues to support the previous definition of SIRS, Sepsis, and Severe Sepsis.
- 16. Sepsis Organ dysfunction Organ dysfunction is defined by the 2016 SCCM/ESICM task force as an increase of two or more points in the SOFA score . The predictive validity of the SOFA score for in-hospital mortality was superior to that for the SIRS criteria . Importantly, the SOFA score is an organ dysfunction score. It is not diagnostic of sepsis nor does it identify those whose organ dysfunction is truly due to infection but rather helps identify patients who potentially have a high risk of dying from infection.
- 17. Septic shock Septic shock is a type of Vasodilatory or distributive shock. Septic shock is defined as sepsis that has circulatory, cellular, and metabolic abnormalities that are associated with a greater risk of mortality than sepsis alone . Clinically, this includes patients who fulfill the criteria for sepsis who, despite adequate fluid resuscitation, require vasopressors to maintain a MAP ≥65 mmHg and have a lactate >18 mg/dL. Per predictions from the SOFA score , patients who fulfill these criteria for septic shock have a higher mortality than those who do not (≥40 versus ≥10 %).
- 18. Severe Sepsis • The term severe sepsis, which originally referred to sepsis that was associated with tissue hypoperfusion (eg, elevated lactate, oliguria) or organ dysfunction (eg, elevated creatinine, coagulopathy), and the term SIRS are no longer used since the 2016 sepsis and septic shock definitions include patients with evidence of tissue hypoperfusion and organ dysfunction.
- 20. Sepsis
- 21. 1. Early sepsis a. Infection and bacteremia b. Identification of early sepsis (qSOFA, NEWS) 2. Sepsis 3. Septic shock 4. Others 1. Multiple organ dysfunction syndrome 2. Systemic inflammatory response Sepsis
- 22. Multiple Organ Dysfunction Syndrome (MODS) MODS refers to progressive organ dysfunction in an acutely ill patient, such that homeostasis cannot be maintained without intervention. It is at the severe end of the severity of illness spectrum of both infectious (sepsis, septic shock) and noninfectious conditions (eg, SIRS from pancreatitis). MODS can be classified as primary or secondary: 1. Primary MODS is the result of a well-defined insult in which organ dysfunction occurs early and can be directly attributable to the insult itself (eg, renal failure due to rhabdomyolysis). 2. Secondary MODS is organ failure that is not in direct response to the insult itself, but is a consequence of the host's response (eg, acute respiratory distress syndrome in patients with pancreatitis). There are no universally accepted criteria for individual organ dysfunction in MODS. However, progressive abnormalities of the following organ-specific parameters are commonly used to diagnose MODS and are also used in scoring systems (eg, SOFA or LODS) to predict ICU mortality : 1. Respiratory – Partial pressure of arterial oxygen (PaO2)/fraction of inspired oxygen (FiO2) ratio 2. Hematology – Platelet count 3. Liver – Serum bilirubin 4. Renal – Serum creatinine (or urine output) 5. Brain – Glasgow coma score 6. Cardiovascular – Hypotension and vasopressor requirement In general, the greater the number of organ failures, the higher the mortality, with the greatest risk being associated with respiratory failure requiring mechanical ventilation.
- 23. 1. Early sepsis a. Infection and bacteremia b. Identification of early sepsis (qSOFA, NEWS) 2. Sepsis 3. Septic shock 4. Others 1. Multiple organ dysfunction syndrome 2. Systemic inflammatory response Sepsis
- 24. The use of SIRS criteria to identify those with sepsis has fallen out of favor since it is considered by many experts that SIRS criteria are present in many hospitalized patients who do not develop infection, and their ability to predict death is poor when compared with other scores such as the SOFA score . SIRS is considered a clinical syndrome that is a form of dysregulated inflammation. It was previously defined as two or more abnormalities in temperature, heart rate, respiration, or WBC count . SIRS may occur in several conditions related, or not, to infection. Noninfectious conditions classically associated with SIRS include autoimmune disorders, pancreatitis, vasculitis, thromboembolism, burns, or surgery. Systemic Inflammatory Response Syndrome (SIRS)
- 26. Definitions The definitions of sepsis are constantly evolving. ‘Sepsis-3’, published in February 2016, moved away from the use of SIRS in the identification of sepsis focussing instead on life-threatening organ dysfunction. • Fever— defined as ‘a state of elevated core temperature which is often, but not necessarily, part of the defensive responses of a multicellular organism (the host) to the invasion of live (microorganisms) or inanimate matter recognized as pathogenic or alien to the host’. • Infection— the presence of organisms in a normally sterile site, usually accompanied by a host inflammatory response. • Bacteraemia— the presence of bacteria in the blood; may be transient. • Systemic inflammatory response syndrome (SIRS)— response to a widevariety of clinical insults which include infectious and non- infectious causes. • Sepsis— a clinical syndrome defined as life-threatening organ dysfunction caused by a dysregulated immune response to infection. • Septic shock— that subset of sepsis in which underlying circulatory and cellular/metabolic abnormalities are profound enough to increase mortality.
- 28. Fever has been recognized as a clinical syndrome since the sixth century BC. Several centuries later, Hippocratic physicians proposed that body temperature was a balance between the four corporal humours— blood, phlegm, black bile, and yellow bile. Devices to measure body temperature have been around since the first century BC. Thermometry became a part of clinical practice in 1868, when Wunderlich declared 37.4°C (98.6°F) to be the normal body temperature and described the diurnal variation of body temperature.
- 30. Clinical Features ‘Sepsis-3’ proposes using the Sequential (sepsis-related) Organ Failure Assessment (SOFA) score to assess organ dysfunction in the presence of infection.
- 31. Clinical Features At present most hospitals will use these clinical definitions: Sepsis is defined as the presence of infection with systemic manifestations, including: (i) physiological variables, e.g. temperature >38.3°C or <36°C, pulse >90 beats/ min, systolic blood pressure <90mmHg, respiratory rate >20/ min, altered mental state, significant oedema or positive fluid balance, hyperglycaemia; (ii) inflammatory variables, e.g. leucocytosis >12 000 cells/ microlitre, leucopenia <4000 cells/ microlitre, C- reactive protein (CRP) >2 standard deviations above normal, plasma procalcitonin > 2 standard deviations above normal value; (iii) organ dysfunction, e.g. arterial hypoxaemia, acute oliguria, creatinine increase >44.2 micromoles/ L, coagulation abnormalities, ileus, thrombocytopenia, hyperbilirubinaemia;
- 32. Severe sepsis refers to sepsis- induced tissue hypoperfusion or organ dysfunction with any of the following thought to be due to the infection: (i) sepsis- induced hypotension; (ii) lactate above ULN; (iii) urine output <0.5mL/ kg/ h for 2h, despite adequate fluid resuscitation; (iv) acute lung injury with PaO2/ FiO2 ratio <250 in the absence of pneumonia as infection source; (v) acute lung injury with PaO2/ FiO2 ratio <200 in the presence of pneumonia as infection source; (vi) serum creatinine >176.8 micromoles/ L; (vii) serum bilirubin >34.2 micromoles/ L; (viii) platelet count <100 000/ microlitre; (ix) coagulopathy INR >1.5. Clinical Features
- 33. Pathogenesis of sepsis (a) Sepsis is defined as a dysregulated host response to infection, leading to life-threatening organ dysfunction. The normally careful inflammatory balance is disturbed, and this dysregulation is associated with a failure to return to homeostasis. Hyperinflammation and immune suppression ensue, to an extent that is detrimental to the host. (b) Once a pathogen has succeeded to cross the mucosal barrier of the host, it can cause sepsis depending on its load and virulence. The host defense system can recognize molecular components of invading pathogens (PAMPs) with specialized receptors (PRRs). Stimulation of PRRs has proinflammatory and immune suppressive consequences. It leads to activation of target genes coding for proinflammatory cytokines (leukocyte activation), inefficient use of the complement system, activation of the coagulation system, and concurrent downregulation of anticoagulant mechanisms and necrotic cell death. This starts a vicious cycle with further progression to sepsis, due to the release of endogenous molecules by injured cells (DAMPs or alarmins), which can further stimulate PRRs. Immune suppression is characterized by massive apoptosis and thereby depletion of immune cells, reprogramming of monocytes and macrophages to a state of a decreased capacity to release proinflammatory cytokines and a disturbed balance in cellular metabolic processes. (c) Sepsis is by definition a disease with organ failure. The clinical
- 34. Laboratory diagnosis • Routine investigations may show a number of abnormalities, as • described in E Clinical features above. • • BCs and samples from suspected sites of infection (e.g. sputum, urine, • stool, pus) should be taken for culture, ideally prior to administration of • antimicrobial therapy.
- 35. Management • Therapeutic priorities— these include early initiation of supportive care to correct physiological abnormalities and institution of appropriate therapy for sepsis. • Stabilize respiration— supplemental oxygen should be given to all patients with sepsis, and oxygen saturations monitored. Intubation and mechanical ventilation may be required. A CXR and arterial blood gas (ABG) should be obtained. • Assess perfusion— blood pressure should be assessed early and often. An arterial line may be required in patients who are shut down or have labile blood pressures. • Establish central venous access— a CVC is inserted in most patients with severe sepsis, in order to infuse fluids and medications and to collect blood samples. • Initial resuscitation— goals during the first 6h, as suggested by the Surviving Sepsis Campaign Guidelines, include: (i) central venous pressure 8– 12mmHg; (ii) central venous (superior vena cava) or mixed venous oxygen saturation 70% or 65%, respectively; (iii) mean arterial pressure ≥65mmHg; (iv) urine output ≥0.5mL/ kg/ h. • Restoration of perfusion— rapid infusion of large volumes of IV fluid are administered, often in 500mL boluses. Careful monitoring is required, as patients may develop non- cardiogenic pulmonary oedema. Vasopressors, e.g. noradrenaline, may be required in patients who remain hypotensive, despite adequate fluid resuscitation. Additional therapies, such as inotropic therapy (e.g. dobutamine) or red cell transfusions, are sometimes given.
- 36. Management • Identification of septic focus— prompt identification and treatment of the focus of infection are essential. Biomarkers of sepsis, e.g. procalcitonin, TREM- 1 (triggering receptor expressed on myeloid cells- 1), and CD64 expression on neutrophils, may be useful to suggest bacterial infection. • Antimicrobial therapy— this should be instigated promptly; the empirical regimen will depend on the likely source of infection, local antibiotic policies, and antibiotic resistance profiles. Poor outcome is associated with delayed or inappropriate therapy. • Additional therapies— glucocorticoid therapy may be of benefit in patients with severe septic shock. Nutritional support improves nutritional outcomes in critically ill patients, but its impact on clinical outcomes from sepsis is uncertain. Intensive insulin therapy is helpful in diabetic patients with hyperglycaemia and insulin resistance. One study has suggested that external cooling may be helpful in patients with severe sepsis. Sepsis treatment protocols also appear to improve outcome.
- 37. Sepsis and septic shock • Sepsis is a life-threatening organ dysfunction that results from the body’s response to infection. • It requires prompt recognition, appropriate antibiotics, careful hemodynamic support, and control of the source of infection. • With the trend in management moving away from protocolized care in favor of appropriate usual care, an understanding of sepsis physiology and best practice guidelines is critical.
- 38. Sepsis and septic shock • Sepsis and particularly septic shock should be recognized as medical emergencies in which time matters, as in stroke and acute myocardial infarction. • Early recognition and rapid institution of resuscitative measures are critical.
- 39. DEFINITIONS HAVE EVOLVED In 1991, sepsis was first defined as a systemic inflammatory response syndrome (SIRS) due to a suspected or confirmed infection with 2 or more of the following criteria4: • Temperature below 36°C or above 38°C • Heart rate greater than 90/minute • Respiratory rate above 20/minute, or arterial partial pressure of carbon dioxide less than 32 mm Hg • White blood cell count less than 4 × 109/L or greater than 12 × 109/L, or more than 10% bands. Severe sepsis was defined as the progression of sepsis to organ dysfunction, tissue hypoperfusion, or hypotension. Septic shock was described as hypotension and organ dysfunction that persisted despite volume resuscitation, necessitating vasoactive medication, and with 2 or more of the SIRS criteria listed above. In 2001, definitions were updated with clinical and laboratory variables.5 In 2004, the Surviving Sepsis Campaign guidelines adopted those definitions, which led to the development of a protocol-driven model for sepsis care used worldwide.6 The US Centers for Medicare and Medicaid Services (CMS) followed suit, defining sepsis as the presence of at least 2 SIRS criteria plus infection; severe sepsis as sepsis with organ dysfunction (including serum lactate > 2 mmol/L); and septic shock as fluid-resistant hypotension requiring vasopressors, or a lactate level of at least 4 mmol/L.7 In 2016, the Sepsis-3 committee8 issued the following new definitions: • Sepsis—A life-threatening condition caused by a dysregulated host response to infection, resulting in organ dysfunction • Septic shock—Circulatory, cellular, and metabolic abnormalities in septic patients, presenting as fluid- refractory hypotension requiring vasopressor therapy with
- 40. Multiple definitions create confusion Both the CMS and international consensus definitions are currently used in clinical practice, with distinct terminology and different identification criteria, including blood pressure and lactate cutoff points. The CMS definition continues to recommend SIRS for sepsis identification, while Sepsis-3 uses sequential organ failure assessment (SOFA) or the quick version (qSOFA) to define sepsis (described below). This has led to confusion among clinicians and has been a contentious factor in the development of care protocols.
- 41. TOOLS FOR IDENTIFYING HIGH RISK: SOFA AND qSOFA • SOFA is cumbersome • SOFA is an objective scoring system to determine major organ dysfunction, based on oxygen levels (partial pressure of oxygen and fraction of inspired oxygen), platelet count, Glasgow Coma Scale score, bilirubin level, creatinine level (or urine output), and mean arterial pressure (or whether vasoactive agents are required). • It is routinely used in clinical and research practice to track individual and aggregate organ failure in critically ill patients.9 • But the information needed is burdensome to collect and not usually available at the bedside to help with clinical decision-making.
- 42. TOOLS FOR IDENTIFYING HIGH RISK: SOFA AND qSOFA qSOFA is simpler… Singer et al8 compared SOFA and SIRS and identified 3 independent predictors of organ dysfunction associated with poor outcomes in sepsis to create the simplified qSOFA: Respiratory rate at least 22 breaths/minute Systolic blood pressure 100 mm Hg or lower Altered mental status (Glasgow Coma Scale score < 15). A qSOFA score of 2 or more with a suspected or confirmed infection was proposed as a trigger for aggressive treatment, including frequent monitoring and ICU admission. qSOFA has the advantage of its elements being easy to obtain in clinical practice.
- 43. TOOLS FOR IDENTIFYING HIGH RISK: SOFA AND qSOFA • …but has limitations • Although qSOFA identifies severe organ dysfunction and predicts risk of death in sepsis, it needs careful interpretation for defining sepsis. • One problem is that it relies on the clinician’s ability to identify infection as the cause of organ dysfunction, which may not be apparent early on, making it less sensitive than SIRS for diagnosing early sepsis.10 • Also, preexisting chronic diseases may influence accurate qSOFA and SOFA measurement.11 • In addition, qSOFA has only been validated outside the ICU, with limited utility in patients already admitted to an ICU.12 • Studies have suggested that the SIRS criteria be used to detect sepsis, while qSOFA should be used only as a triaging tool.1