1031 talk2
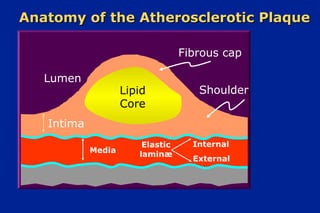
- 1. Anatomy of the Atherosclerotic PlaqueAnatomy of the Atherosclerotic Plaque Lumen Lipid Core Fibrous cap Shoulder Intima Media Elastic laminæ Internal External
- 2. Thrombosis of a DisruptedThrombosis of a Disrupted Atheroma, the Cause of Most AcuteAtheroma, the Cause of Most Acute Coronary Syndromes, Results from:Coronary Syndromes, Results from: Weakening ofWeakening of the fibrous capthe fibrous cap Thrombogenicity of the lipid core Illustration courtesy of Michael J. Davies, M.D.
- 3. Matrix Metabolism and Integrity ofMatrix Metabolism and Integrity of the Plaque’s Fibrous Capthe Plaque’s Fibrous Cap Libby P. Circulation 1995;91:2844-2850. + + + + + + – Synthesis Breakdown Lipid core IL-1 TNF-α MCP-1 M-CSF Fibrous capIFN-IFN-γγ CD-40L Collagen-degradingCollagen-degrading ProteinasesProteinases Tissue FactorTissue Factor ProcoagulantProcoagulant
- 4. Plaque Rupture with ThrombosisPlaque Rupture with Thrombosis Thrombus Fibrous cap 1 mm Lipid core Illustration courtesy of Frederick J. Schoen, M.D., Ph.D.
- 5. Potential Time Course of Statin EffectsPotential Time Course of Statin Effects * Time course established DaysDays YearsYears LDL-CLDL-C lowered*lowered* InflammationInflammation reducedreduced VulnerableVulnerable plaquesplaques stabilizedstabilized EndothelialEndothelial functionfunction restoredrestored IschemicIschemic episodesepisodes reducedreduced CardiacCardiac eventsevents reduced*reduced*
- 6. HDL Metabolism andHDL Metabolism and Reverse Cholesterol TransportReverse Cholesterol Transport A-I Liver CE CE CE FCFC LCAT FC Bile SR-BI A-I ABC1 = ATP-binding cassette protein 1; A-I = apolipoprotein A-I; CE = cholesteryl ester; FC = free cholesterol; LCAT = lecithin:cholesterol acyltransferase; SR-BI = scavenger receptor class BI ABC1 Macrophage Mature HDL Nascent HDL
- 7. Role of CETP in HDL MetabolismRole of CETP in HDL Metabolism A-I Liver CE CE FCFC LCAT FC Bile SR-BI A-I ABC1 Macrophage CE B CETP = cholesteryl ester transfer protein LDL = low-density lipoprotein LDLR = low-density lipoprotein receptor VLDL = very-low-density lipoprotein LDLR VLDL/LDL CETP Mature HDL Nascent HDL CE SRA Oxidation
- 8. CETP DeficiencyCETP Deficiency • Autosomal co-dominant; due to mutations in both alleles of CETP gene • Markedly elevated levels of HDL-C and apoA-I • Delayed catabolism of HDL cholesteryl ester and apoA- I • HDL particles enlarged and enriched in cholesteryl ester • No evidence of protection against atherosclerosis; possible increased risk of premature atherosclerotic vascular disease
- 9. SummarySummary • HDL metabolism is complex • HDL-C and apoA-I levels are determined by both production and catabolic rates • Rates of reverse cholesterol transport cannot be determined solely by steady-state levels of HDL-C and apoA-I • Effect of genetic defects or of interventions that alter HDL metabolism on atherosclerosis depends on specific metabolic effects on HDL • Genes and proteins involved in HDL metabolism are potential targets for development of novel therapeutic strategies for atherosclerosis
- 10. • Increase apo A-I production • Promote reverse cholesterol transport • Delay catabolism of HDL HDL as a Therapeutic Target:HDL as a Therapeutic Target: Potential StrategiesPotential Strategies
- 11. A-I HDL and Reverse CholesterolHDL and Reverse Cholesterol TransportTransport LiverLiver CECECE FC LCATLCATFCFC BileBile SR-BISR-BI ABCA1ABCA1 MacrophageMacrophage MatureMature HDLHDL NascentNascent HDLHDL A-IA-I FC CECE FC
- 12. • Antioxidant effects • Inhibition of adhesion molecule expression • Inhibition of platelet activation • Prostacyclin stabilization • Promotion of NO production Mechanisms Other Than ReverseMechanisms Other Than Reverse Cholesterol Transport by Which HDLCholesterol Transport by Which HDL May be AntiatherogenicMay be Antiatherogenic
- 13. ApoA-I MutationsApoA-I Mutations • Modest to marked reduction in HDL-C and apoA-I • Rapid catabolism of apoA-I • Systemic amyloidosis • Premature atherosclerotic disease (rare)
- 14. • Small molecule upregulation of apo A-I gene transcription • Intravenous infusion of recombinant protein (wild-type apo A-I, apo A-IMilano) • Administration of peptides based on apo A-I sequence • Somatic gene transfer of apo A-I DNA (liver, intestine, muscle, hematopoetic cells) Approaches to Increasing Apo A-IApproaches to Increasing Apo A-I ProductionProduction
- 15. CETP DeficiencyCETP Deficiency • Autosomal co-dominant; due to mutations in both alleles of CETP gene • Markedly elevated levels of HDL-C and apoA-I • Delayed catabolism of HDL cholesteryl ester and apoA- I • HDL particles enlarged and enriched in cholesteryl ester • No evidence of protection against atherosclerosis; possible increased risk of premature atherosclerotic vascular disease
- 16. Genes Involved in HDL MetabolismGenes Involved in HDL Metabolism Potential Targets for Development ofPotential Targets for Development of Novel Therapies for AtherosclerosisNovel Therapies for Atherosclerosis • HDL-associated apolipoproteins — ApoA-I — ApoE — ApoA-IV • HDL-modifying plasma enzymes and transfer proteins — LCAT — Lipoprotein lipase — CETP — Hepatic lipase — PLTP — Endothelial lipase • Cellular and cell-surface proteins that influence HDL metabolism — ABC1 — SR-BI
- 17. Gene Transfer of ApoA-I to LiverGene Transfer of ApoA-I to Liver Induces Regression of AtherosclerosisInduces Regression of Atherosclerosis in LDLRin LDLR–/––/– MiceMice 0 1 2 3 4 5 Baseline Adnull Aorticlesion(%) AdhapoA-I * * P ≤ 0.05 Tangirala R et al. Circulation 1999;100:1816–1822
- 18. Overexpression of LCAT PreventsOverexpression of LCAT Prevents Development of Atherosclerosis inDevelopment of Atherosclerosis in Transgenic RabbitsTransgenic Rabbits * P < 0.003 LCAT = lecithin-cholesterol acyltransferase; Tg = transgenic Hoeg JM et al. Proc Natl Acad Sci U S A. 1996;93:11448–11453 Copyright ©1996 National Academy of Sciences, USA. 0 10 20 30 40 50 Control LCAT Tg Atherosclerotic surfacearea(%) *
- 19. Inflammation and AtherosclerosisInflammation and Atherosclerosis Inflammation may determine plaque stability - Unstable plaques have increased leukocytic infiltrates - T cells, macrophages predominate rupture sites - Cytokines and metalloproteinases influence both stability and degradation of the fibrous cap Lipid lowering may reduce plaque inflammation - Decreased macrophage number - Decreased expression of collagenolytic enzymes (MMP-1) - Increased interstitial collagen - Decreased expression of E-selectin - Reduced calcium depositionLibby P. Circulation 1995;91:2844-2850. Ross R. N Engl J Med 1999;340:115-126.
- 20. • Reduced initiation and progression of atherosclerosis in transgenic mice and rabbits • Regression of pre-existing atherosclerosis in animals Increased Apo A-I Production isIncreased Apo A-I Production is Antiatherogenic in AnimalsAntiatherogenic in Animals
- 21. Lipid LevelsLipid Levels as the Targetas the Target AtherosclerosisAtherosclerosis as the Targetas the Target Treatment ApproachTreatment Approach Measure and treat levels Only patients with levels above normal benefit Start on low dose and titrate Goal is “normal” levels Benefit same regardless of Rx Based on epidemiologic and observational data Find patients with disease or at risk All patients benefit, regardless of lipid levels Start on clinical trial– proven doses Goal is getting on and staying on Rx Statins have independent benefits Based on randomized clinical trial evidence
- 22. Role of Lipoproteins inRole of Lipoproteins in InflammationInflammation
- 23. Atherosclerosis is an InflammatoryAtherosclerosis is an Inflammatory DiseaseDisease Ross R. N Engl J Med 1999;340:115-126. EndotheliumEndothelium Vessel LumenVessel Lumen IntimaIntimaFoam CellFoam Cell MonocyteMonocyte CytokinesCytokines Growth FactorsGrowth Factors MetalloproteinasesMetalloproteinases Cell ProliferationCell Proliferation Matrix DegradationMatrix Degradation MacrophageMacrophage
- 24. Lipoprotein Classes and InflammationLipoprotein Classes and Inflammation Doi H et al. Circulation 2000;102:670-676; Colome C et al. Atherosclerosis 2000; 149:295-302; Cockerill GW et al. Arterioscler Thromb Vasc Biol 1995;15:1987-1994. HDLHDLLDLLDLChylomicrons,Chylomicrons, VLDL, andVLDL, and their catabolictheir catabolic remnantsremnants > 30 nm> 30 nm 20–22 nm20–22 nm Potentially proinflammatoryPotentially proinflammatory 9–15 nm9–15 nm Potentially anti-Potentially anti- inflammatoryinflammatory
- 25. Structure of LDLStructure of LDL Murphy HC et al. Biochemistry 2000;39:9763-970. Hydrophobic CoreHydrophobic Core of Triglyceride andof Triglyceride and Cholesteryl EstersCholesteryl Esters apoBapoB Surface MonolayerSurface Monolayer of Phospholipidsof Phospholipids and Freeand Free CholesterolCholesterol
- 26. Role of LDL in InflammationRole of LDL in Inflammation Steinberg D et al. N Engl J Med 1989;320:915-924. EndotheliumEndothelium Vessel LumenVessel Lumen LDLLDL LDL Readily Enter the Artery Wall Where They May be ModifiedLDL Readily Enter the Artery Wall Where They May be Modified LDLLDL IntimaIntima Modified LDLModified LDL Modified LDL are ProinflammatoryModified LDL are Proinflammatory Hydrolysis of PhosphatidylcholineHydrolysis of Phosphatidylcholine to Lysophosphatidylcholineto Lysophosphatidylcholine Other Chemical ModificationsOther Chemical Modifications Oxidation of LipidsOxidation of Lipids and ApoBand ApoB AggregationAggregation
- 27. LDLLDL LDLLDL Modified LDL Stimulate Expression ofModified LDL Stimulate Expression of MCP-1 in Endothelial CellsMCP-1 in Endothelial Cells Navab M et al. J Clin Invest 1991;88:2039-2046. EndotheliumEndothelium Vessel LumenVessel Lumen IntimaIntima MonocyteMonocyte Modified LDLModified LDL MCP-1MCP-1
- 28. LDLLDL LDLLDL Differentiation of Monocytes intoDifferentiation of Monocytes into MacrophagesMacrophages Steinberg D et al. N Engl J Med 1989;320:915-924. EndotheliumEndothelium Vessel LumenVessel Lumen IntimaIntima MonocyteMonocyte Modified LDLModified LDL Modified LDL PromoteModified LDL Promote Differentiation ofDifferentiation of Monocytes intoMonocytes into MacrophagesMacrophages MCP-1MCP-1 MacrophageMacrophage
- 29. LDLLDL LDLLDL Modified LDL Induces Macrophages to ReleaseModified LDL Induces Macrophages to Release Cytokines That Stimulate Adhesion MoleculeCytokines That Stimulate Adhesion Molecule Expression in Endothelial CellsExpression in Endothelial Cells Nathan CF. J Clin Invest 1987;79:319-326. EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte Modified LDLModified LDL MacrophageMacrophage MCP-1MCP-1 AdhesionAdhesion MoleculesMolecules CytokinesCytokines IntimaIntima
- 30. LDLLDL LDLLDL EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte MacrophageMacrophage MCP-1MCP-1 AdhesionAdhesion MoleculesMolecules Steinberg D et al. N Engl J Med 1989;320:915-924. Macrophages Express ReceptorsMacrophages Express Receptors That Take up Modified LDLThat Take up Modified LDL Foam CellFoam Cell Modified LDLModified LDL Taken up byTaken up by MacrophageMacrophage IntimaIntima
- 31. LDLLDL LDLLDL EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte MacrophageMacrophage AdhesionAdhesion MoleculesMolecules Macrophages and Foam CellsMacrophages and Foam Cells Express Growth Factors andExpress Growth Factors and ProteinasesProteinases Foam CellFoam Cell IntimaIntima ModifiedModified LDLLDLCytokinesCytokines Cell ProliferationCell Proliferation Matrix DegradationMatrix Degradation Growth FactorsGrowth Factors MetalloproteinasesMetalloproteinases Ross R. N Engl J Med 1999;340:115-126. MCP-1MCP-1
- 32. EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte MacrophageMacrophage MCP-1MCP-1AdhesionAdhesion MoleculesMolecules The Remnants of VLDL and ChylomicronsThe Remnants of VLDL and Chylomicrons are Also Proinflammatoryare Also Proinflammatory Foam CellFoam Cell IntimaIntimaModifiedModified RemnantsRemnantsCytokinesCytokines Cell ProliferationCell Proliferation Matrix DegradationMatrix Degradation Doi H et al. Circulation 2000;102:670-676. Growth FactorsGrowth Factors MetalloproteinasesMetalloproteinases Remnant LipoproteinsRemnant Lipoproteins RemnantsRemnants
- 33. Structure of HDL ParticleStructure of HDL Particle A-I A-I A-II A-I, A-II = apolipoprotein A-I, A-II; CE = cholesteryl ester; TG = triglycerides CE TG
- 34. Structure of HDLStructure of HDL Rye KA et al. Atherosclerosis 1999;145:227-238. Hydrophobic CoreHydrophobic Core of Triglyceride andof Triglyceride and Cholesteryl EstersCholesteryl Esters apoA-IIapoA-II Surface MonolayerSurface Monolayer of Phospholipidsof Phospholipids and Freeand Free CholesterolCholesterolapoA-IapoA-I
- 35. LDLLDL LDLLDL Miyazaki A et al. Biochim Biophys Acta 1992;1126:73-80. EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte Modified LDLModified LDL MacrophageMacrophage MCP-1MCP-1 AdhesionAdhesion MoleculesMolecules CytokinesCytokines HDL Prevent Formation of Foam CellsHDL Prevent Formation of Foam Cells IntimaIntimaHDL Promote Cholesterol EffluxHDL Promote Cholesterol Efflux FoamFoam CellCell
- 36. LDLLDL LDLLDL Mackness MI et al. Biochem J 1993;294:829-834. EndotheliumEndothelium Vessel LumenVessel LumenMonocyteMonocyte Modified LDLModified LDL MacrophageMacrophage MCP-1MCP-1 AdhesionAdhesion MoleculesMolecules CytokinesCytokines HDL Inhibit the Oxidative Modification of LDLHDL Inhibit the Oxidative Modification of LDL FoamFoam CellCell HDL Promote Cholesterol EffluxHDL Promote Cholesterol Efflux IntimaIntima HDL InhibitHDL Inhibit OxidationOxidation of LDLof LDL
- 37. Inhibition of LDL Oxidation byInhibition of LDL Oxidation by HDL:HDL: Role of ParaoxonaseRole of Paraoxonase • Paraoxonase is transported in plasma as a component of HDL • Paraoxonase is known to inhibit the oxidative modification of LDL • Thus, the presence of paraoxonase in HDL may account for a proportion of the antioxidant properties of these lipoproteins Mackness MI et al. FEBS Lett 1991;286:152-154.
- 38. Role of HDL Apolipoproteins inRole of HDL Apolipoproteins in Removing Oxidized Lipids fromRemoving Oxidized Lipids from LDLLDL • CETP transfers oxidized lipids from LDL to HDL • The oxidized lipids in HDL are reduced by HDL apolipoproteins • The liver takes up reduced lipids from HDL more rapidly than from LDL Christison JK et al. J Lipid Res 1995;36:2017-2026; Gardner B et al. J Biol Chem 1998;273:6088-6095.
- 39. LDLLDL LDLLDL Cockerill GW et al. Arterioscler Thromb Vasc Biol 1995;15:1987-1994. EndotheliumEndothelium Vessel LumenVessel Lumen MonocyteMonocyte Modified LDLModified LDL MacrophageMacrophage MCP-1MCP-1 AdhesionAdhesion MoleculesMolecules CytokinesCytokines Inhibition of Adhesion MoleculesInhibition of Adhesion Molecules IntimaIntima HDL InhibitHDL Inhibit OxidationOxidation of LDLof LDL HDL Inhibit Adhesion Molecule ExpressionHDL Inhibit Adhesion Molecule Expression FoamFoam CellCell HDL Promote Cholesterol EffluxHDL Promote Cholesterol Efflux
- 40. EndotheliumEndothelium Vessel LumenVessel Lumen MCP-1MCP-1 E-SelectinE-Selectin Charo IF. Curr Opin Lipidol 1992;3:335-343. Recruitment of Blood Monocytes byRecruitment of Blood Monocytes by Endothelial Cell Adhesion MoleculesEndothelial Cell Adhesion Molecules IntimaIntima VCAM-1VCAM-1 ICAM-1ICAM-1 StickingSticking MonocyteMonocyte RollingRolling TransmigrationTransmigration
- 41. HDL Inhibit Endothelial CellHDL Inhibit Endothelial Cell Sphingosine KinaseSphingosine Kinase Xia P et al. J Biol Chem 1999;274:33143-33147. SphingomyelinSphingomyelin CeramideCeramide SphingosineSphingosine Sph-1-PSph-1-P HDLHDL NF-NF-KKBB Adhesion ProteinAdhesion Protein SynthesisSynthesis SM-aseSM-ase Sph KinaseSph Kinase ++ TNFTNFαα XX
- 42. Heterogeneity of HDLHeterogeneity of HDL Rye KA et al. Atherosclerosis 1999;145:227-238. Apolipoprotein CompositionApolipoprotein Composition A-I HDLA-I HDL A-I/A-II HDLA-I/A-II HDL A-II HDLA-II HDL Particle ShapeParticle Shape DiscoidalDiscoidal SphericalSpherical Lipid CompositionLipid Composition TG, CE, and PLTG, CE, and PL Particle SizeParticle Size HDLHDL2b2b HDLHDL2a2a HDLHDL3a3a HDLHDL3b3b HDLHDL3c3c
- 43. Inhibition of Endothelial CellInhibition of Endothelial Cell VCAM-1 Expression by HDL:VCAM-1 Expression by HDL: Effect of HDL CompositionEffect of HDL Composition • Inhibition unaffected by replacing apoA-I with apoA-II • Inhibition unaffected by replacing apoA-I with SAA • Inhibition unaffected by varying the cholesteryl ester or triglyceride content of HDL • Inhibition ISIS affected by varying HDL phospholipids Baker PW et al. J Lipid Res 1999;40:345-353.
- 44. Additional Anti-inflammatoryAdditional Anti-inflammatory Properties of HDLProperties of HDL • HDL bind and neutralize proinflammatory lipopolysaccharides • The acute phase reactant SAA binds to plasma HDL, which possibly neutralizes the effects of SAA Baumberger C et al. Pathobiology 1991;59:378-383; Benditt EP et al. Proc Natl Acad Sci U S A 1977;74:4025-4028.
- 45. Animal StudiesAnimal Studies • Increasing the concentration of LDL or remnant particles in animal models results in expression of endothelial cell adhesion molecules at the sites where atherosclerotic lesions develop • Infusion or overexpression of apoA-I in animal models reduces oxidation of LDL and reduces endothelial cell adhesion molecule expression Sakai A et al. Arterioscler Thromb Vasc Biol 1997;17:310-316; Dimayuga P et al. Biochem Biophys Res Commun 1999;264:465-468; Cockerill GW et al. Circulation 2001;103:108- 112; Theilmeier G et al. FASEB J 2000;14:2032-2039.
- 46. Studies in HumansStudies in Humans • Treatments that reduce the level of LDL reduce the plasma levels of C-reactive protein and soluble adhesion molecules BUT • These effects may represent pleiotropic effects of lipid-modifying agents and be unrelated to the changes in lipoprotein levels Ridker PM et al.Ridker PM et al. CirculationCirculation 1998;98:839-844; Hackman A et al.1998;98:839-844; Hackman A et al. CirculationCirculation 1996;93:1334-1338.1996;93:1334-1338.
- 47. SummarySummary • The evidence that atherosclerosis is an inflammatory disorder is overwhelming • LDL are subject to proinflammatory modifications that may account for their atherogenicity • HDL have anti-inflammatory properties that may contribute to their ability to protect against atherosclerosis
- 48. ConclusionsConclusions • Strategies that reduce proinflammatory modifications to LDL may reduce atherosclerosis • Strategies that increase the anti-inflammatory properties of HDL may also reduce atherosclerosis • More research is needed to determine whether pharmacological increases in HDL are anti- inflammatory and reduce atherosclerosis
- 49. HDL as a Therapeutic TargetHDL as a Therapeutic Target
- 50. Is HDL-C Simply a Marker ofIs HDL-C Simply a Marker of Increased Cardiovascular Risk?Increased Cardiovascular Risk? • Smoke • Are sedentary • Are obese • Are insulin resistant or diabetic • Have hypertriglyceridemia • Have chronic inflammatory disorders Low HDL-C levels are commonly found in patients who:
- 51. Production of Apo A-I by Liver andProduction of Apo A-I by Liver and IntestineIntestine A-IA-I A-IIA-II LiverLiver IntestineIntestine HDLHDL A-IA-I HDLHDL
- 52. • Reduced initiation and progression of atherosclerosis in transgenic mice and rabbits • Regression of pre-existing atherosclerosis in animals Increased Apo A-I Production isIncreased Apo A-I Production is Antiatherogenic in AnimalsAntiatherogenic in Animals
- 53. • Increase apo A-I production • Promote reverse cholesterol transport • Delay catabolism of HDL HDL Metabolism as a TherapeuticHDL Metabolism as a Therapeutic Target: Potential StrategiesTarget: Potential Strategies
- 54. • Small molecule upregulation of apo A-I gene transcription • Intravenous infusion of recombinant protein (wild-type apo A-I, apo A-IMilano) • Administration of peptides based on apo A-I sequence • Somatic gene transfer of apo A-I DNA (liver, intestine, muscle, hematopoetic cells) Approaches to Increasing Apo A-IApproaches to Increasing Apo A-I ProductionProduction
- 55. • Increase apo A-I production • Promote reverse cholesterol transport • Delay catabolism of HDL HDL as a Therapeutic Target:HDL as a Therapeutic Target: Potential StrategiesPotential Strategies
- 56. A-I HDL and Reverse CholesterolHDL and Reverse Cholesterol TransportTransport LiverLiver CECECE FC LCATLCATFCFC BileBile SR-BISR-BI ABCA1ABCA1 MacrophageMacrophage MatureMature HDLHDL NascentNascent HDLHDL A-IA-I FC CECE FC
- 57. Regulation of Cholesterol Efflux inRegulation of Cholesterol Efflux in the Macrophagethe Macrophage FC FC oxysterols LXR/RXRLXR/RXR ABCA1 PPARsPPARs A-I
- 58. Pharmacologic Manipulation ofPharmacologic Manipulation of Cholesterol EffluxCholesterol Efflux LXR/RXR PPARsPPARs Fibrates, TZDs, new agentsFibrates, TZDs, new agents New agents A-I FC ABCA1
- 59. • Increase apo A-I production • Promote reverse cholesterol transport • Delay catabolism of HDL HDL as a Therapeutic Target:HDL as a Therapeutic Target: Potential StrategiesPotential Strategies
- 60. • Antioxidant effects • Inhibition of adhesion molecule expression • Inhibition of platelet activation • Prostacyclin stabilization • Promotion of NO production Mechanisms Other Than ReverseMechanisms Other Than Reverse Cholesterol Transport by Which HDLCholesterol Transport by Which HDL May be AntiatherogenicMay be Antiatherogenic
- 61. LiverLiver CECECE FCFCFC LCATLCATFCFC BileBile SR-BISR-BI A-I ABCA1ABCA1 MacrophageMacrophage A-IA-I TGTG CECE HDL Metabolism: IntravascularHDL Metabolism: Intravascular Remodeling of HDLRemodeling of HDL KidneyKidney PLPL FCFC PLPL
- 62. LiverLiver HLHL A-IA-I TGTG CECE HDL Metabolism: Role of HepaticHDL Metabolism: Role of Hepatic LipaseLipase KidneyKidney PLPL HDLHDL22 A-IA-I CECE PLPL HDLHDL33
- 63. LiverLiver CECECE FCFCFC LCATLCATFCFC BileBile SR-BISR-BI A-I ABCA1ABCA1 MacrophageMacrophage A-IA-I FC CECE HDL Metabolism: Role of CETPHDL Metabolism: Role of CETP FCFC KidneyKidney LDLRLDLR CE TG CETPCETP BB VLDL/LDLVLDL/LDL
- 64. HDL Metabolism in CETP DeficiencyHDL Metabolism in CETP Deficiency CE FCFCFC LCATLCAT A-I ABCA1ABCA1 MacrophageMacrophage A-IA-I CECE FCFC CE TG CETPCETP BB VLDL/LDLVLDL/LDL DelayedDelayed catabolismcatabolism X
- 65. 0 5 10 15 20 25 30 35 Okamoto H et al. Nature 2000;406:203-207. Inhibition of CETP by JTT-705 inInhibition of CETP by JTT-705 in Cholesterol-Fed Rabbits SignificantlyCholesterol-Fed Rabbits Significantly Reduced Aortic AtherosclerosisReduced Aortic Atherosclerosis %AorticLes Control SimvastatinJTT-705
- 66. HDL Metabolism: Influence of CETPHDL Metabolism: Influence of CETP InhibitionInhibition LiverLiver CECECE FCFCFC LCATLCATFCFC BileBile SR-BISR-BI A-I ABCA1ABCA1 MacrophageMacrophage A-IA-I FC CECE FCFC LDLRLDLR CE TG CETPCETP BB VLDL/LDLVLDL/LDL X
- 67. • Weight reduction and increased physical activity • LDL-C is primary target of therapy • Non-HDL-C is secondary target of therapy (if triglycerides ≥200 mg/dL) • Consider nicotinic acid or fibrates Management of Low HDL-CManagement of Low HDL-C Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. JAMA 2001;285:2486-2497.
- 68. • Therapeutic lifestyle changes – Smoking cessation – Regular aerobic exercise – Weight loss – Alcohol use? Management of Low HDL-CManagement of Low HDL-C
- 69. • Therapeutic lifestyle changes • Pharmacologic therapy – Statins Management of Low HDL-CManagement of Low HDL-C
- 70. • Therapeutic lifestyle changes • Pharmacologic therapy – Statins – Fibrates Management of Low HDL-CManagement of Low HDL-C
- 71. • Therapeutic lifestyle changes • Pharmacologic therapy – Statins – Fibrates – Niacin Management of Low HDL-CManagement of Low HDL-C
- 72. • Lifestyle changes and secondary causes • Pharmacologic therapy – If LDL-C elevated: statin – If TG elevated: fibrate – If isolated low HDL-C: niacin • Combination therapy Management of Low HDL-CManagement of Low HDL-C
- 73. • LDL-C remains the primary target of lipid-altering therapies • HDL-C is an important CHD risk factor • Even small increases in HDL-C may confer substantial benefit • Intervention to raise HDL-C levels should be considered in high-risk patients SummarySummary
- 74. • 48-year-old man with metabolic syndrome and CHD • After therapeutic lifestyle changes and a starting dose of statin: Cholesterol 179 mg/dL Triglycerides 252 mg/dL LDL-C 97 mg/dL HDL-C 32 mg/dL Glucose 104 mg/dL Approach to the Patient with LowApproach to the Patient with Low HDL-CHDL-C
- 75. Drugs Main effects Sites of action abciximab anticoagulant stops platelet activation platelets amiloride (combination with frusemide is frumil) potassium sparing diuretic kidney (distal tubules) amiodarone class III anti-arrhythmic myocardium aspirin anticoagulant stops platelet activation platelets atropine (sometimes used to stop vagus bradycardia) parasympatholytic, increases heart rate pacemaker cells (sino-atrial node) captopril reduces arterial blood pressure relaxes vascular smooth muscle clopidogrel anticoagulant stops platelet activation platelets digitalis and ouabain increase cardiac contractility, delay AV node triggering all tissues, but the Na/Ca exchanger is mainly in heart dipyridamole (often used for X-ray imaging) coronary vasodilation coronary vasculature furosemide (= frusemide) diuretic kidney (loop of Henle) isoprenaline (and other adrenaline analogues) increase cardiac contractility many tissues losartan reduces arterial blood pressure relaxes vascular smooth muscle lovastatin reduces blood cholesterol levels liver morphine pain relief (mainly) brain nitroglycerine (and many other organic nitrates) reduce cardiac work load relaxes vascular smooth muscle propranolol reduces cardiac contractility, class II anti-arrhythmic many tissues quinidine, novocaine and other local anaesthetics class I anti-arrhythmics myocardium spironolactone (usually added to other diuretics) reduces diuretic potassium losses kidney (distal tubules) urokinase (streptokinase is cheaper but antigenic) dissolves blood clots (fibrinolytic) blood clots verapamil, nifedipine and other dihydropyridines reduce cardiac work load, class IV anti-arrhythmic myocardium; relax vascular smooth muscle warfarin anticoagulant vit. K antagonist liver Check list of common cardiac drugs
- 76. Plaque with multiple breaks in the cap and both an intraplaque and an intraluminal mural component of thrombosis
- 77. An episode of plaque disruption in which the torn cap projects into the lumen of the artery and thrombus is contained within the plaque core
- 78. Diagrammatic representation of stages of development of thrombosis after disruption
- 79. Schematic Time Course of HumanSchematic Time Course of Human AtherogenesisAtherogenesis Transition from chronic to acute atheromaTransition from chronic to acute atheroma Ischemic HeartIschemic Heart DiseaseDisease CerebrovascularCerebrovascular DiseaseDisease Peripheral VascularPeripheral Vascular DiseaseDisease
- 80. NormalNormal FattyFatty StreakStreak FibrousFibrous PlaquePlaque OcclusiveOcclusive AtheroscleroticAtherosclerotic PlaquePlaque PlaquePlaque Rupture/Rupture/ Fissure &Fissure & ThrombosisThrombosis MIMI StrokeStroke Critical LegCritical Leg IschemiaIschemia Clinically SilentClinically Silent CoronaryCoronary DeathDeath Increasing AgeIncreasing Age Effort AnginaEffort Angina ClaudicationClaudication UnstableUnstable AnginaAngina Atherosclerosis: A ProgressiveAtherosclerosis: A Progressive ProcessProcess Courtesy of P Ganz.
- 81. Libby P. Lancet. 1996;348:S4-S7. Media – T lymphocyte – Macrophage foam cell (tissue factor+ ) – “Activated” intimal SMC (HLA-DR+ ) – Normal medial SMC Fibrous cap Intima Lipid core Lumen The Anatomy of AtheroscleroticThe Anatomy of Atherosclerotic PlaquePlaque
- 82. Nissen et al. In: Topol. Interventional Cardiology Update. 14;1995. Angiographically InapparentAngiographically Inapparent AtheromaAtheroma
- 83. The Matrix Skeleton of UnstableThe Matrix Skeleton of Unstable Coronary Artery PlaqueCoronary Artery Plaque Davies MJ. Circulation. 1996;94:2013-2020. Fissures in the fibrous cap
- 84. Libby P. Circulation. 1995;91:2844-2850. Characteristics of Plaques Prone toCharacteristics of Plaques Prone to RuptureRupture – T lymphocyte – Macrophage foam cell (tissue factor+ ) – “Activated” intimal SMC (HLA-DR+ ) – Normal medial SMC “Stable” plaque “Vulnerable” plaque Lumen area of detail Media Fibrous cap Lumen Lipid core Lipid core
- 85. Libby P. Circulation. 1995;91:2844-2850. Proposed Mechanisms of EventProposed Mechanisms of Event Reduction by Lipid-Lowering TherapyReduction by Lipid-Lowering Therapy • Improved endothelium-dependent vasodilation • Stabilization of atherosclerotic lesions – especially nonobstructive, vulnerable plaques • Reduction in inflammatory stimuli – lipoproteins and modified lipoproteins • Prevention, slowed progression, or regression of atherosclerotic lesions
- 86. Atheroma are not merely filled withAtheroma are not merely filled with lipid, but contain cells whose functionslipid, but contain cells whose functions critically influence atherogenesis:critically influence atherogenesis: Intrinsic Vascular Wall Cells: Endothelium Smooth Muscle Cells Inflammatory Cells: Macrophages T Lymphocytes Mast Cells
- 87. Cell Types in the Human AtheromaCell Types in the Human Atheroma Monocyte/Monocyte/ MacrophageMacrophage T-lymphocytesT-lymphocytesTunica Media Intima Smooth muscle cells EndotheliumEndothelium
- 88. NoNo symptomssymptoms ++ SymptomsSymptoms Schematic Time Course of HumanSchematic Time Course of Human AtherogenesisAtherogenesis Time (y)Time (y) SymptomsSymptoms Lesion initiationLesion initiation Ischemic HeartIschemic Heart DiseaseDisease CerebrovascularCerebrovascular DiseaseDisease Peripheral VascularPeripheral Vascular DiseaseDisease
- 89. Macrophage Functions inMacrophage Functions in AtherogenesisAtherogenesis AttachmentAttachment
- 90. Leukocyte–Endothelial AdhesionLeukocyte–Endothelial Adhesion MoleculesMoleculesMonoMono TT BB PMNPMN
- 91. Vascular Cell Adhesion Molecule 1Vascular Cell Adhesion Molecule 1 (VCAM-1)(VCAM-1) Binds monocytes and lymphocytes - Cells found in atheroma Expressed by endothelium over nascent fatty streaks Expressed by microvessels of the mature atheroma
- 92. An atherogenic diet rapidly inducesAn atherogenic diet rapidly induces VCAM-1, a cytokine-regulatableVCAM-1, a cytokine-regulatable mononuclear leukocyte adhesionmononuclear leukocyte adhesion molecule, in rabbit aorticmolecule, in rabbit aortic endotheliumendothelium Li H et al. Arterioscler Thromb 1993;13:197-204.
- 93. VCAM-1 Expression in Rabbit AortaVCAM-1 Expression in Rabbit Aorta Li H et al. Arterioscler Thromb 1993;13:197-204. 3 weeks on atherogenic diet
- 94. PenetrationPenetration Macrophage Functions inMacrophage Functions in AtherogenesisAtherogenesis
- 95. Monocyte Chemoattractant Protein 1Monocyte Chemoattractant Protein 1 (MCP-1)(MCP-1) A potent mononuclear cell chemoattractant Produced by endothelial and smooth muscle cells Localizes in human and experimental atheroma
- 96. Absence of monocyteAbsence of monocyte chemoattractant protein-1 reduceschemoattractant protein-1 reduces atherosclerosis in low-densityatherosclerosis in low-density lipoprotein receptor–deficient micelipoprotein receptor–deficient mice Gu L et al. Mol Cell 1998;2:275-281.
- 97. Reduced Lipid Deposition in MCP-1–Reduced Lipid Deposition in MCP-1– Deficient Atherosclerotic MiceDeficient Atherosclerotic Mice Gu L et al. Mol Cell 1998;2:275-281. LDL-R –/–LDL-R –/– MCP-1 +/+MCP-1 +/+ LDL-R –/–LDL-R –/– MCP-1 –/–MCP-1 –/–
- 98. Gu L et al. Mol Cell 1998;2:275-281. Reduced Lipid Deposition in MCP-1–Reduced Lipid Deposition in MCP-1– Deficient Atherosclerotic MiceDeficient Atherosclerotic Mice 0 5 10 15 20 25 30 OilRedStaining %AorticSurfaceStained Time on Diet: 12 – 14 weeks +/+ -/- ** * +/+ -/- 20 – 25 weeks *P = 0.001 compared to +/+ **p = 0.005 compared to +/+
- 99. Macrophage Functions inMacrophage Functions in AtherogenesisAtherogenesis Division
- 100. Molecular Mediators of AtherogenesisMolecular Mediators of Atherogenesis M-CSFMCP-1 VCAM-1
- 101. Matrix Metabolism and Integrity ofMatrix Metabolism and Integrity of the Plaque’s Fibrous Capthe Plaque’s Fibrous Cap Libby P. Circulation 1995;91:2844-2850. + + + + + + – Synthesis Breakdown Lipid core IL-1 TNF-α MCP-1 M-CSF Fibrous capIFN-IFN-γγ CD-40L Collagen-degradingCollagen-degrading ProteinasesProteinases Tissue FactorTissue Factor ProcoagulantProcoagulant
- 102. Increased Expression of InterstitialIncreased Expression of Interstitial Collagenase (CL) by Smooth MuscleCollagenase (CL) by Smooth Muscle Cells (SMC) and Macrophages (MCells (SMC) and Macrophages (Mφφ) in) in Human AtheromaHuman Atheroma Galis ZS et al. J Clin Invest 1994;94:2493-2503.
Notes de l'éditeur
- Anatomy of the atherosclerotic plaque After the leukocytes have accumulated in the lesion, they often undergo death, sometimes by apoptosis, which can lead to a lipid core covered by a fibrous cap.
- Thrombosis of a disrupted atheroma: weakening of the fibrous cap Most coronary syndromes are caused by thrombosis of a disrupted atheroma, which can result from weakening of the fibrous cap and enhanced thrombogenicity of the lipid core.
- Matrix metabolism and integrity of the plaque&apos;s fibrous cap This slide depicts the current understanding of the dynamics of the plaque&apos;s stability and thrombogenicity. The inflammatory cells can send molecular messages to the smooth muscle cells (interferon-) that inhibit the ability of this cell type to synthesize new collagen to strengthen the plaque&apos;s fibrous cap. In addition, the inflammatory cells can release proteolytic enzymes capable of degrading collagen and other structurally important constituents of the plaque&apos;s fibrous cap. Thus, when there is inflammation in the intima, the collagen responsible for the integrity of the plaque&apos;s fibrous cap is under double attack, subject to both decreased synthesis and increased degradation. This sets the stage for plaque disruption. The inflammatory cells also are responsible for signaling and producing increased quantities of tissue factor, a potent procoagulant deemed responsible for thrombosis of ruptured plaques. Reference: Libby P. Molecular bases of the acute coronary syndromes. Circulation 1995;91:2844-2850.
- Plaque rupture with thrombosis It would matter little if there were a rupture in the plaque&apos;s fibrous cap were it not for the ensuing thrombus.
- Potential time course of statin effects CHD risk reduction with a statin appears to occur as a result of several related changes, including restoration of endothelial function, reduction in inflammation, and stabilization of vulnerable plaque. The time course for these antiatherosclerotic effects of statins ranges from days to years. Within weeks to months after beginning statin therapy, endothelial function of coronary arteries is restored. Concurrent with this or following by just a few months is a reduction in inflammatory markers, such as high-sensitivity C-reactive protein. These effects appear to coincide with the reduction in ischemic events demonstrated after about 18 months of statin therapy. After several years of therapy (i.e., 1.5–2.5 years), fatal and nonfatal myocardial infarction rates begin to decline in statin-treated patients, and after 5 years of therapy, significant reductions have been documented. These changes coincide somewhat with stabilization of vulnerable atherosclerotic plaque during which the lipid-rich core of plaque is replaced with connective tissue and matrix.
- HDL Metabolism and Reverse Cholesterol Transport Cholesterol that is synthesized or deposited in peripheral tissues is returned to the liver in a process referred to as reverse cholesterol transport in which high-density lipoprotein (HDL) plays a central role. HDL may be secreted by the liver or intestine in the form of nascent particles consisting of phospholipid and apolipoprotein A-I (apoA-I). Nascent HDL interacts with peripheral cells, such as macrophages, to facilitate the removal of excess free cholesterol (FC), a process facilitated by the ATP-binding cassette protein 1 (ABC1) gene. FC is generated in part by the hydrolysis of intracellular cholesteryl ester (CE) stores. HDL is then converted into mature CE–rich HDL as a result of the plasma cholesterol-esterifying enzyme lecithin:cholesterol acyltransferase (LCAT), which is activated by apoA-I. CE may be removed by several different pathways, including selective uptake by the liver, ie, the removal of lipid without the uptake of HDL proteins (shown in this slide). Selective uptake appears to be mediated by the scavenger receptor class-B, type I (SR-BI), which is expressed in the liver and has been shown to be a receptor for HDL. CE derived from HDL contributes to the hepatic–cholesterol pool used for bile acid synthesis. Cholesterol is eventually excreted from the body either as bile acid or as free cholesterol in the bile. References: Fielding CJ, Fielding PE. Molecular physiology of reverse cholesterol transport. J Lipid Res. 1995;36:211–228. Breslow JL. Familial disorders of high-density lipoprotein metabolism. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. 7th ed. New York: McGraw-Hill; 1995:2031–2052. Acton S, Rigotti A, Landschulz KT, et al. Identification of scavenger receptor SR-BI as a high-density lipoprotein receptor. Science. 1996;271:518–520.
- Role of CETP in HDL Metabolism This slide shows the selective uptake of high-density lipoprotein (HDL) cholesteryl ester (CE), described in the previous slide, together with another important pathway of reverse cholesterol transport involving the action of plasma CE transfer protein (CETP). CE can be transferred from HDL to apolipoprotein (apo) B-containing proteins, such as very-low-density lipoproteins (VLDLs) and low-density lipoproteins (LDLs), by CETP. Through uptake of LDL by the liver via hepatic LDL receptors, cholesterol can then be returned to the liver, where it may eventually be excreted as bile. (This slide also illustrates the current belief that only modified apoB-containing proteins are taken up by macrophages. “Oxidation” is given as an example of modification.) References Havel RJ, Kane JP. Introduction: structure and metabolism of plasma lipoproteins. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. 7th ed. New York: McGraw-Hill; 1995:1841–1851. Tall AR. Plasma cholesteryl ester transfer protein. J Lipid Res. 1993;34:1255–1274. Steinberg D. A docking receptor for HDL cholesterol esters. Science. 1996;271:460–461.
- CETP Deficiency It appears that factors regulating the exchange of high-density lipoprotein (HDL) cholesteryl ester (CE) with very-low-density lipoprotein (VLDL) triglycerides, and the subsequent catabolism of HDL triglycerides, play an important role in regulating HDL levels. CE transfer protein (CETP) facilitates the transfer of CEs among lipoproteins. Deficiencies in the gene coding for CETP have been described. Four different CETP gene mutations were reported in Japanese subjects. For example, a splicing defect, present in approximately 2% of the population, is a null mutation; homozygotes have markedly elevated levels of HDL-cholesterol (100–250 mg/dL) and of apolipoprotein (apo) AI. CETP deficiency results in delayed catabolism of CE in HDL and of apoA-I. This leads to the production of large HDL particles, enriched in CE. It has not been demonstrated that CETP deficiency is associated with a decreased risk of atherosclerotic cardiovascular disease; in fact, there is some evidence that the impaired reverse cholesterol transport resulting from genetic CETP deficiency leads to an increased risk of premature atherosclerotic vascular disease. References: Tall AR, Dammerman M, Breslow JL. Disorders of lipoprotein metabolism. In: Chien KR, ed. Molecular Basis of Cardiovascular Disease: A Companion to Braunwald’s Heart Disease. Philadelphia: W.B. Saunders; 1999:413–427. Tall AR. Plasma high density lipoproteins: metabolism and relationship to atherogenesis. J Clin Invest. 1990;86:379–384. Tall AR. Plasma lipid transfer proteins. J Lipid Res. 1986;27:361–368. Tall AR. Plasma lipid transfer proteins. Annu Rev Biochem. 1995;64:235–257.
- Summary The metabolism of high-density lipoprotein (HDL) is a complex process. Metabolic turnover studies suggest that plasma levels of HDL-cholesterol (HDL-C) and apolipoprotein (apo) AI (the major structural component of HDL) are determined by the rate of synthesis versus the rate of catabolism. Rates of reverse cholesterol transport cannot be determined solely by steady-state levels of HDL-C and apoA-I. Genetic defects in HDL metabolism or therapeutic interventions that alter HDL metabolism may affect the development of atherosclerosis. Current research is directed at the genes and proteins that regulate HDL metabolism with the goal of identifying new therapeutic targets for the prevention and treatment of atherosclerosis.
- HDL metabolism as a therapeutic target: potential strategies (II) Another approach to targeting HDL would be to promote the process of reverse cholesterol transport.
- HDL and reverse cholesterol transport HDL is believed to protect against atherosclerosis at least in part through the process of reverse cholesterol transport, whereby excess free cholesterol (FC) is removed from cells in peripheral tissues, such as macrophages within the arterial wall, and returned to the liver for excretion in the bile. FC is generated in part by the hydrolysis of intracellular cholesteryl ester (CE) stores. Several key molecules play a role in reverse cholesterol transport, including ATP-binding cassette protein A1 (ABCA1), lecithin:cholesterol acyltransferase (LCAT), and scavenger receptor class-B, type I (SR-BI). Promotion of this pathway could in theory help reduce atherosclerosis.
- Mechanisms other than reverse cholesterol transport by which HDL may be antiatherogenic It is important to keep in mind that reverse cholesterol transport is only one mechanism by which HDL may directly protect against atherosclerosis. There are a variety of other properties of HDL that have been described, primarily in in vitro studies, which could theoretically contribute to the antiatherogenic effect of HDL. If these properties are indeed operative, a strategy that raises HDL, even if it does not promote reverse cholesterol transport, could theoretically be effective against atherosclerosis.
- ApoA-I Mutations Mutations in the apolipoprotein A-I (apoA-I) gene may also lead to marked reductions in levels of high-density lipoprotein cholesterol (HDL-C) (usually 15–30 mg/dL) and apoA-I protein. The decrease in apoA-I levels among individuals with these structural mutations is the result of rapid catabolism of apoA-I. The first apoA-I mutation to be described was apoA-IMilano, which results in an average 40% decrease in apoA-I and a 67% decrease in HDL-C. Subjects with structural apoA-I mutations do not appear to have clinical sequelae, although a mutation in the apoA-I gene at the amino-terminus has been described in association with systemic amyloidosis. ApoA-I structural mutations are only rarely associated with premature atherosclerotic disease. References: Rader DJ. Lipid disorders. In: Topol EJ, ed. Textbook of Cardiovascular Medicine. Philadelphia: Lippincott-Raven; 1998:59–90. Franceschini G, Sirtori CR, Capurso A, Weisgraber KH, Mahley RW. A-IMilano apoprotein: decreased high-density lipoprotein cholesterol levels with significant lipoprotein modifications and without clinical atherosclerosis in an Italian family. J Clin Invest. 1980;66:892–900. Weisgraber KH, Bersot TP, Mahley RW, Franceschini G, Sirtori CR. A-IMilano apoprotein: isolation and characterization of a cysteine-containing variant of the A-I apoprotein from human high-density lipoproteins. J Clin Invest. 1980;66:901–907. Tall AR, Dammerman M, Breslow JL. Disorders of lipoprotein metabolism. In: Chien KR, ed. Molecular Basis of Cardiovascular Disease: A Companion to Braunwald’s Heart Disease. Philadelphia: W.B. Saunders; 1999:413–427. Nichols WC, Dwulet FE, Liepnieks J, et al. Variant apolipoprotein AI as a major constituent of a human hereditary amyloid. Biochem Biophys Res Commun. 1988;156:762–768. Soutar AK, Hawkins PN, Vigushin DM, et al. Apolipoprotein AI mutation Arg-60 causes autosomal dominant amyloidosis. Proc Natl Acad Sci U S A. 1992;89:7389–7393.
- Approaches to increasing apo A-I production Multiple approaches to increasing apo A-I production are in development in preclinical animal models, and some are in early clinical trials. Perhaps the most desirable approach would be a small molecule that upregulates apo A-I gene transcription. Another approach is the intravenous infusion of a recombinant apo A-I protein. A clinical trial on apo A-IMilano is currently in progress. Administration of peptides based on apo A-I sequence has been shown to reduce atherosclerosis in mice. Finally, the concept of using somatic gene transfer of apo A-I DNA to a tissue in which apo A-I could be made and secreted is attractive and is being piloted in animal studies.
- CETP Deficiency It appears that factors regulating the exchange of high-density lipoprotein (HDL) cholesteryl ester (CE) with very-low-density lipoprotein (VLDL) triglycerides, and the subsequent catabolism of HDL triglycerides, play an important role in regulating HDL levels. CE transfer protein (CETP) facilitates the transfer of CEs among lipoproteins. Deficiencies in the gene coding for CETP have been described. Four different CETP gene mutations were reported in Japanese subjects. For example, a splicing defect, present in approximately 2% of the population, is a null mutation; homozygotes have markedly elevated levels of HDL-cholesterol (100–250 mg/dL) and of apolipoprotein (apo) AI. CETP deficiency results in delayed catabolism of CE in HDL and of apoA-I. This leads to the production of large HDL particles, enriched in CE. It has not been demonstrated that CETP deficiency is associated with a decreased risk of atherosclerotic cardiovascular disease; in fact, there is some evidence that the impaired reverse cholesterol transport resulting from genetic CETP deficiency leads to an increased risk of premature atherosclerotic vascular disease. References: Tall AR, Dammerman M, Breslow JL. Disorders of lipoprotein metabolism. In: Chien KR, ed. Molecular Basis of Cardiovascular Disease: A Companion to Braunwald’s Heart Disease. Philadelphia: W.B. Saunders; 1999:413–427. Tall AR. Plasma high density lipoproteins: metabolism and relationship to atherogenesis. J Clin Invest. 1990;86:379–384. Tall AR. Plasma lipid transfer proteins. J Lipid Res. 1986;27:361–368. Tall AR. Plasma lipid transfer proteins. Annu Rev Biochem. 1995;64:235–257.
- Genes Involved in HDL Metabolism Potential Targets for Development of Novel Therapies for Atherosclerosis Further elucidation of the molecular mechanisms involved in high-density lipoprotein (HDL) metabolism promises to help identify potential targets for decreasing the incidence and progression of atherosclerotic cardiovascular disease. Investigations of the genetic mechanisms involved in normal and defective HDL metabolism may lead to the development of novel therapies. Research is focusing on three areas: HDL-associated apolipoproteins; HDL-modifying plasma enzymes and transfer proteins (eg, lecithin:cholesterol acyltransferase [LCAT], cholesteryl ester transfer protein [CETP], and hepatic lipase); and cellular and cell-surface proteins involved in HDL metabolism (eg, ATP-binding cassette transporter 1[ABC1] and scavenger receptor class-B, type I [SR-BI]). References: Rader DJ. Gene therapy for atherosclerosis. Mol Ther. 1998;1:680–689. Fruchart JC, Duriez P. High-density lipoproteins and coronary heart disease: future prospects in gene therapy. Biochimie. 1998;80:167–172. Acton SL, Kozarsky KF, Rigotti A. The HDL receptor SR-BI: a new therapeutic target for atherosclerosis? Mol Med Today. 1999;5:518–524. Rader DJ, Mauglais C. Genes influencing HDL metabolism: new perspectives and implications for atherosclerosis prevention and treatment. Mol Med Today. 2000; in press.
- Gene Transfer of ApoA-I to Liver Induces Regression of Atherosclerosis in LDLR–/– Mice In the study represented by this slide, low-density lipoprotein (LDL)-receptor–deficient mice (ie, LDLR-/-) were fed a diet to induce atherosclerotic lesions. Recombinant adenovirus encoding human apolipoprotein A-I (adhapoA-I) or control adenovirus was injected intravenously to express apoA-I in the liver. Mice injected with apoA-I were found to produce significantly higher apoA-I and high-density lipoprotein (HDL)-cholesterol than did control mice (adnull). Furthermore, as shown in this slide, compared with mice at baseline, atherosclerosis progressed in mice injected with the control adenovirus. In addition, in adhapoA-I mice, the total aortic lesion area was reduced by 70% compared with that in baseline mice. Thus, liver-directed gene transfer of human apoA-I was shown to result in significant regression of pre-existing atherosclerotic lesions in LDL-receptor–deficient mice. Reference: Tangirala RK, Tsukamoto K, Chun SH, Usher D, Pure E, Rader DJ. Regression of atherosclerosis induced by liver-directed gene transfer of apolipoprotein A-I in mice. Circulation. 1999;100:1816–1822.
- Overexpression of LCAT Prevents Development of Atherosclerosis in Transgenic Rabbits Lecithin:cholesterol acyltransferase (LCAT) is a key enzyme in high-density lipoprotein (HDL) and cholesterol metabolism. Hoeg et al demonstrated that transgenic (Tg) rabbits overexpressing human LCAT had a 15-fold greater LCAT activity compared with non-Tg control animals, and that this overexpression was associated with a 6.7-fold increase in plasma HDL-cholesterol (HDL-C) concentrations. In addition, a 0.3% cholesterol diet significantly increased HDL-C concentrations in both groups. The cholesterol-rich diet raised non–HDL-C concentrations in both groups as well, but to a significantly greater extent in control animals compared with the LCAT Tg group. These differences in plasma lipoprotein response to a cholesterol-rich diet paralleled the susceptibility to developing aortic atherosclerosis. Compared with non-Tg controls, LCAT Tg rabbits were protected from diet-induced atherosclerosis. An 86% reduction in atherosclerotic surface area was found in the LCAT Tg group compared with controls (P &lt; 0.003). These results suggest that LCAT may be a potential new target for therapy to prevent atherosclerosis. Reference: Hoeg JM, Santamarina-Fojo S, Berard AM, et al. Overexpression of lecithin:cholesterol acyltransferase in transgenic rabbits prevents diet-induced atherosclerosis. Proc Natl Acad Sci U S A. 1996;93:11448–11453.
- Inflammation and atherosclerosis Why study inflammation in heart disease? Two general hypotheses emerging from the basic science community have driven this research. The first is the concept that inflammation itself may determine plaque stability. Unstable plaques have increased leukocytic infiltrates in them, and T-cells and macrophages predominate at the rupture sites in these plaques. Also, cytokines and metalloproteinases may influence plaque stability and the degradation of the fibrous cap. But in addition to the idea that atherosclerosis is fundamentally an inflammatory disorder is the recognition in the basic science literature that lipid lowering in general may reduce plaque inflammation. That is to say, experimental studies have now demonstrated reduced macrophage number within atherosclerotic plaques treated with lipid-lowering statin therapy as well as decreased expression of collagenolytic enzymes and the attenuation of other markers of the inflammatory process. References: Libby P. Molecular bases of the acute coronary syndromes. Circulation 1995;91:2844-2850. Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med 1999;340:115-126.
- Increased apo A-I production is antiatherogenic in animals Studies in transgenic mice and rabbits have clearly established that overexpression of apo A-I reduces the initiation and progression of atherosclerosis. Studies using somatic gene transfer to liver in mice have demonstrated regression of pre-existing atherosclerotic lesions.
- Treatment approach The clinical trials with HMG-CoA reductase inhibitors provided evidence that in patients with established atherosclerosis, even those considered as having normal or low total cholesterol or LDL-C levels benefited from statin treatment. There has also been a growing body of experimental evidence that statins may have benefits beyond reducing LDL-C and increasing HDL-C. This evidence can be used to create a treatment framework that focuses on targeting the underlying atherosclerotic vascular disease process as the primary treatment target. The presence of atherosclerosis would itself be considered sufficient evidence that that the patient would benefit from statin treatment (&quot;whatever the patient&apos;s lipid level is, it is too high for them, because they have the disease&quot;). In other words, statins become a &quot;treatment for atherosclerosis&quot; as opposed to merely a more expensive way of lowering cholesterol. The focus shifts to reducing risk through a combination of cardioprotective therapies rather than modifying individual risk factors in isolation. Reference: Fonarow GC, Gawlinski A. Rationale and design of the Cardiac Hospitalization Atherosclerosis Management Program at the University of California Los Angeles. Am J Cardiol. 2000;85:10A-17A.
- Role of lipoproteins in inflammation
- Atherosclerosis is an inflammatory disease Atherosclerosis involves the cellular infiltration of several cell types, including monocytes, T lymphocytes, and perhaps even mast cells. Monocytes interact with the endothelial layer, attach firmly to the endothelium, and migrate into the subendothelial space, where the monocytes differentiate into macrophages. Macrophages release a variety of chemicals, including cytokines, and also take up lipids, becoming foam cells. Macrophages and foam cells secrete growth factors, which lead to cell proliferation and matrix production, as well as metalloproteinases, which lead to matrix degeneration. Thus, macrophages and foam cells both contribute to lesion growth and may contribute to instability and thrombotic events. Reference: Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med 1999;340:115-126.
- Lipoprotein classes and inflammation All the major lipoprotein classes impact in some way on the inflammatory process that leads to development of atherosclerosis. The triglyceride-rich lipoproteins—chylomicrons, very low density lipoprotein (VLDL), and their catabolic remnants—and low-density lipoprotein (LDL) are potentially proinflammatory, whereas high-density lipoprotein (HDL) is potentially anti-inflammatory. References: Doi H, Kugiyama K, Oka H, Sugiyama S, Ogata N, Koide SI, Nakamura SI, Yasue H. Remnant lipoproteins induce proatherothrombogenic molecules in endothelial cells through a redox-sensitive mechanism. Circulation 2000;102:670-676. Colome C, Martinez‑Gonzalez J, Vidal F, de Castellarnau C, Badimon L. Small oxidative changes in atherogenic LDL concentrations irreversibly regulate adhesiveness of human endothelial cells: effect of the lazaroid U74500A. Atherosclerosis 2000;149:295-302. Cockerill GW, Rye K-A, Gamble JR, Vadas MA, Barter PJ. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler Thromb Vasc Biol 1995;15:1987-1994.
- Structure of LDL Of all of the plasma lipoproteins, LDL has been most investigated in terms of its role in inflammation. LDL consists of a surface monolayer of phospholipids and free cholesterol and a single molecule of apolipoprotein (apo) B, which encircles the lipoprotein. This surface monolayer surrounds a hydrophobic core of mainly cholesteryl esters but also some triglycerides. In itself, LDL is almost certainly not proinflammatory, but the particle can become modified in many ways. It is the modified LDL particle that is proinflammatory and proatherogenic. Reference: Murphy HC, Burns SP, White JJ, Bell JD, Iles RA. Investigation of human low-density lipoprotein by 1H nuclear magnetic resonance spectroscopy: mobility of phosphatidylcholine and sphingomyelin headgroups characterizes the surface layer. Biochemistry 2000;39:9763-9770.
- Role of LDL in inflammation LDL readily enters the artery wall by crossing the endothelial membrane. Once in the arterial wall, if LDL accumulates, it is subject to a variety of modifications. The best known of these is oxidation, both of the lipids and of the apo B. LDL is also subject to aggregation, and its phospholipids are subject to hydrolysis by phospholipases to form lysophosphatidylcholine. Several other chemical modifications have also been reported. The net effect of these changes is the production of a variety of modified LDL particles, and the evidence is now very strong that these modified LDL particles are proinflammatory. Reference: Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL. Beyond cholesterol: modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med 1989;320:915-924.
- Modified LDL stimulate expression of MCP-1 in endothelial cells Modified LDL is involved in many stages of the inflammatory process that leads to the development of atherosclerosis. Modified LDL activates endothelial cells to express monocyte chemotactic protein 1 (MCP-1), which attracts monocytes from the vessel lumen and into the subendothelial space, in what is one of the very early stages in the inflammatory process leading to the development of atherosclerosis. Reference: Navab M, Imes SS, Hama SY, Hough GP, Ross LA, Bork RW, Valente AJ, Berliner JA, Drinkwater DC, Laks H, et al. Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J Clin Invest 1991;88:2039-2046.
- Differentiation of monocytes into macrophages The modified LDL plays an important role in promoting the differentiation of monocytes into macrophages, a key step in the inflammatory process on the way to the development of atherosclerosis. Reference: Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL. Beyond cholesterol: modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med 1989;320:915-924.
- Modified LDL induces macrophages to release cytokines that stimulate adhesion molecule expression in endothelial cells After modified LDL promotes the differentiation of monocytes into macrophages, the macrophages release a variety of chemicals, including cytokines. Of these cytokines, tumor necrosis factor α (TNF-α) and interleukin-1 (IL-1) activate endothelial cells to express adhesion molecules that bind monocytes, making them available for recruitment into the subendothelial space by MCP-1. Reference: Nathan CF. Secretory products of macrophages. J Clin Invest 1987;79:319-326.
- Macrophages express receptors that take up modified LDL The activated macrophages also express a variety of scavenger receptors, several of which recognize the different forms of modified LDL. The macrophages take up the LDL through these scavenger receptors, accumulate the lipid, and are converted into the lipid-rich foam cells that are the hallmark of atherosclerosis. Reference: Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL. Beyond cholesterol: modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med 1989;320:915-924.
- Macrophages and foam cells express growth factors and proteinases Once the macrophage has taken up lipid and been converted into a foam cell, all the cell types necessary for the inflammatory process that leads to atherosclerosis are present. Macrophages and foam cells produce not only cytokines but also a variety of growth factors that lead to cell proliferation and matrix production, and metalloproteinases that lead to matrix degeneration. Thus, macrophages and foam cells both contribute to lesion growth and may contribute to instability and thrombotic events. Reference: Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med 1999;340:115-126.
- The remnants of VLDL and chylomicrons are also pro-inflammatory VLDL remnants and chylomicron remnants behave in much the same way as LDL. They enter the subendothelial space, where they become modified, and the modified remnants stimulate MCP-1, promote the differentiation of monocytes into macrophages, and are taken up by the macrophages to form foam cells. Like LDL, the remnant lipoproteins are proinflammatory and proatherogenic. References: Doi H, Kugiyama K, Oka H, Sugiyama S, Ogata N, Koide SI, Nakamura SI, Yasue H. Remnant lipoproteins induce proatherothrombogenic molecules in endothelial cells through a redox-sensitive mechanism. Circulation 2000;102:670-676.
- Structure of HDL Particle The function of lipoproteins is to transport cholesterol and triglycerides (TGs) in the blood. The five major families of lipoproteins are: chylomicrons, very-low-density lipoproteins (VLDLs), low-density lipoproteins (LDLs), intermediate-density lipoproteins (IDLs), and high-density lipoproteins (HDLs). HDL is the smallest lipoprotein and contains the least amount of lipid. This slide shows the structure of this lipoprotein particle. HDL contains a lipid core of cholesteryl esters (CEs) and TGs surrounded by phospholipids and specialized proteins known as apolipoproteins (apos). Apos are required for the structural integrity of lipoproteins and direct their metabolic interactions with enzymes, lipid transport proteins, and cell-surface receptors (as described in subsequent slides). ApoA-I is a major component of all HDL particles and is synthesized in the liver and intestine (see next slide). ApoA-II, the second most abundant apolipoprotein in HDL, is synthesized in the liver; its function is unclear. References: Havel RJ, Kane JP. Introduction: structure and metabolism of plasma lipoproteins. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. 7th ed. New York: McGraw-Hill; 1995:1841–1851. Breslow JL. Familial disorders of high-density lipoprotein metabolism. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. 7th ed. New York: McGraw-Hill; 1995:2031–2052.
- Structure of HDL HDL has the same essential structure as LDL, with a surface monolayer of phospholipids and free cholesterol and a hydrophobic core consisting mainly of cholesteryl esters but also some triglyceride. However, HDL particles are smaller and contain different apolipoproteins, mainly apo A-I and apo A-II. Both these apolipoproteins have properties that protect the lipids against oxidative modification. In addition, some of the other proteins transported by HDL, such as paraoxonase, have antioxidant properties. Therefore, whereas LDL is very susceptible to oxidative modification, HDL is relatively resistant to it, and this is one of the reasons underlying the anti-inflammatory properties of HDL. Reference: Rye KA, Clay MA, Barter PJ. Remodelling of high density lipoproteins by plasma factors. Atherosclerosis 1999;145:227-238.
- HDL prevent formation of foam cells Perhaps the best-known function of HDL is the promotion of cholesterol efflux from cells. Efflux of cholesterol from foam cells leads to a reduction in foam cell formation; although the macrophages may accumulate, they are not converted into foam cells. As a result, the inflammatory process is arrested to a certain extent. Therefore, HDL is anti-inflammatory and also protects against the development of atherosclerosis. Reference: Miyazaki A, Rahim AT, Ohta T, Morino Y, Horiuchi S. High density lipoprotein mediates selective reduction in cholesteryl esters from macrophage foam cells. Biochim Biophys Acta 1992;1126:73-80.
- HDL inhibit the oxidative modification of LDL HDL has protective effects in addition to promoting cholesterol efflux. One of the best known of these is the ability to inhibit the oxidation of LDL. To the extent that LDL oxidation is an important step in the development of the inflammatory process, this property of HDL is clearly anti-inflammatory. Reference: Mackness MI, Abbott C, Arrol S, Durrington PN. The role of high-density lipoprotein and lipid-soluble antioxidant vitamins in inhibiting low-density lipoprotein oxidation. Biochem J 1993;294:829-834.
- Inhibition of LDL oxidation by HDL: role of paraoxonase The importance of paraoxonase is now fairly well established. Paraoxonase is transported in plasma as a component of HDL, and it has also been shown in vitro in many studies that paraoxonase inhibits the oxidative modification of LDL. The working hypothesis of a number of groups is that the presence of paraoxonase in HDL may account for at least a proportion of the antioxidant properties of these lipoproteins, and thus contributes to HDL&apos;s anti-inflammatory effect. Reference: Mackness MI, Arrol S, Durrington PN. Paraoxonase prevents accumulation of lipoperoxides in low-density lipoprotein. FEBS Lett 1991;286:152-154.
- Role of HDL apolipoproteins in removing oxidized lipids from LDL HDL has an antioxidant and anti-inflammatory effect beyond transporting paraoxonase. Cholesteryl ester transfer protein (CETP) transfers oxidized lipids from LDL to HDL. Once these oxidized lipids are in HDL, they are reduced by HDL apolipoproteins; this has been shown for both apo A-I and apo A-II. It has also been shown that the liver takes up reduced lipids from HDL more rapidly than from LDL. Therefore, HDL reduces the oxidized lipids in LDL, a further anti-inflammatory effect of HDL. References: Christison JK, Rye KA, Stocker R. Exchange of oxidized cholesteryl linoleate between LDL and HDL mediated by cholesteryl ester transfer protein. J Lipid Res 1995;36:2017-2026. Garner B, Waldeck AR, Witting PK, Rye KA, Stocker R. Oxidation of high density lipoproteins. II. Evidence for direct reduction of lipid hydroperoxides by methionine residues of apolipoproteins AI and AII. J Biol Chem 1998;273:6088-6095.
- Inhibition of adhesion molecules The cytokine-induced expression of adhesion molecules in endothelial cells has been shown in vitro and more recently in vivo to be inhibited by HDL, in a process that potentially blocks a very early inflammatory stage in the development of atherosclerosis. Reference: Cockerill GW, Rye K-A, Gamble JR, Vadas MA, Barter PJ. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler Thromb Vasc Biol 1995;15:1987-1994.
- Recruitment of blood monocytes by endothelial cell adhesion molecules Adhesion molecules are involved in the adhesion of monocytes to endothelial cells. Monocytes come in random contact with endothelial cells, and the adhesion molecule E-selectin slows the monocyte by inducing rolling of the monocyte along the endothelial surface before firm attachment to vascular cell adhesion molecule 1 (VCAM-1) or intercellular adhesion molecule 1 (ICAM-1), which interact with integrins on the monocyte surface. Once the monocyte is tightly bound, it then migrates between endothelial cells in response to MCP-1. Reference: Charo IF. Monocyte–endothelial cell interactions. Curr Opin Lipidol 1992;3:335-343.
- HDL inhibit endothelial cell sphingosine kinase The sphingomyelin pathway has been shown to be involved in the mechanism by which TNF-α stimulates the expression of adhesion molecules in endothelial cells. TNF-α activates sphingomyelinase, which begins the sphingomyelin pathway through ceramide, sphingosine, sphingosine 1-phosphate, and then to the nuclear transcription factor NK-κB and ultimately to the expression of a variety of adhesion proteins. In a recently reported study, HDL has been shown to inhibit sphingosine kinase, which catalyzes the sphingosine-to–sphingosine 1-phosphate step. This is at least one of the mechanisms by which HDL inhibits adhesion molecule expression. Reference: Xia P, Vadas MA, Rye KA, Barter PJ, Gamble JR. High density lipoproteins (HDL) interrupt the sphingosine kinase signaling pathway: a possible mechanism for protection against atherosclerosis by HDL. J Biol Chem 1999;274:33143-33147.
- Heterogeneity of HDL The HDL particles in human plasma are heterogeneous. They vary in particle shape; most are spherical, but there is a small population of discoidal particles. Particles also vary in apolipoprotein composition, lipid composition, and size. Nevertheless, all of these subpopulations inhibit the expression of adhesion molecules on endothelial cells. Reference: Rye KA, Clay MA, Barter PJ. Remodelling of high density lipoproteins by plasma factors. Atherosclerosis 1999;145:227-238.
- Inhibition of endothelial cell VCAM-1 expression by HDL: effect of HDL composition In studies conducted with either native human HDL or reconstituted HDL, it has been shown that the ability of HDL to inhibit endothelial cell VCAM-1 is unaffected by changing the apolipoprotein composition; for example, by replacing apo A-I with apo A-II. In a recently published paper, even replacing apo A-I with the acute phase reactant serum amyloid A (SAA) did not affect the ability of HDL to inhibit adhesion molecule expression. The inhibition is also unaffected by varying the cholesteryl ester or triglyceride content of HDL. However, the inhibition is affected by varying the composition of HDL phospholipids, and it has been shown that the phospholipid component of HDL is the key component responsible for inhibiting adhesion molecule expression. References: Baker PW, Rye KA, Gamble JR, Vadas MA, Barter PJ. Ability of reconstituted high density lipoproteins to inhibit cytokine-induced expression of vascular cell adhesion molecule-1 in human umbilical vein endothelial cells. J Lipid Res 1999;40:345-353. Ashby D, Gamble J, Vadas M, Fidge N, Siggins S, Rye K, Barter PJ. Lack of effect of serum amyloid A (SAA) on the ability of high-density lipoproteins to inhibit endothelial cell adhesion molecule expression. Atherosclerosis 2001;154:113-121.
- Additional anti-inflammatory properties of HDL In addition to HDL&apos;s cholesterol efflux properties, antioxidant properties, and ability to inhibit adhesion molecule expression in endothelial cells, over the last 10 to 15 years HDL has been shown to have many other effects, several of which are potentially anti-inflammatory. HDL can bind and neutralize the proinflammatory lipopolysaccharides, and may also neutralize the effects of the acute phase reactant SAA, which when it is released into the blood is transported predominantly bound to HDL. References: Baumberger C, Ulevitch RJ, Dayer JM. Modulation of endotoxic activity of lipopolysaccharide by high-density lipoprotein. Pathobiology 1991;59:378-383. Benditt EP, Eriksen N. Amyloid protein SAA is associated with high density lipoprotein from human serum. Proc Natl Acad Sci U S A 1977;74:4025-4028.
- Animal studies Much of what has been shown in vitro is now being observed in vivo, at least in animal studies. In a variety of animal models in which the concentration of either LDL or remnant particles were increased, there was an associated increase in the expression of endothelial cell adhesion molecules, which has been shown in several studies to occur at the sites where atherosclerotic lesions subsequently developed. It has also been shown more recently that infusion of either HDL- or apo A-I–containing vesicles into transgenic animals that were overexpressing apo A-I resulted in the reduced oxidation of LDL. Also, endothelial cell adhesion molecule expression was reduced both in an acute inflammatory model in pigs and in apo E–knockout mice. References: Sakai A, Kume N, Nishi E, Tanoue K, Miyasaka M, Kita T. P-selectin and vascular cell adhesion molecule-1 are focally expressed in aortas of hypercholesterolemic rabbits before intimal accumulation of macrophages and T lymphocytes. Arterioscler Thromb Vasc Biol 1997;17:310-316. Dimayuga P, Zhu J, Oguchi S, Chyu KY, Xu XO, Yano J, Shah PK, Nilsson J, Cercek B. Reconstituted HDL containing human apolipoprotein A-1 reduces VCAM-1 expression and neointima formation following periadventitial cuff-induced carotid injury in apoE null mice. Biochem Biophys Res Commun 1999;264:465-468. Cockerill GW, Huehns TY, Weerasinghe A, Stocker C, Lerch PG, Miller NE, Haskard DO. Elevation of plasma high-density lipoprotein concentration reduces interleukin-1–induced expression of E-selectin in an in vivo model of acute inflammation. Circulation 2001;103:108-112. Theilmeier G, De Geest B, Van Veldhoven PP, Stengel D, Michiels C, Lox M, Landeloos M, Chapman MJ, Ninio E, Collen D, Himpens B, Holvoet P. HDL-associated PAF-AH reduces endothelial adhesiveness in apoE–/– mice. FASEB J 2000;14:2032-2039.
- Studies in humans There is still not a lot of hard evidence in vivo in human studies about the role of lipoproteins in inflammation or about the atherogenic or antiatherogenic properties of lipoproteins. However, it has been shown that treatments that reduced the level of LDL also reduced plasma levels of C-reactive protein and soluble adhesion molecules. These studies have generally been conducted with statins, and because there is growing evidence that statins have a variety of pleiotropic effects in addition to their lipid-modifying role, it remains an open question whether the changes in inflammatory mediators such as C-reactive protein and soluble adhesion molecules are secondary to the LDL reduction or to the pleiotropic effects. The studies in humans are consistent with the in vitro studies and the animal studies, but the proof is still far from certain. References: Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, Flaker GC, Braunwald E, for the Cholesterol and Recurrent Events (CARE) Investigators. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Circulation 1998;98:839-844. Hackman A, Abe Y, Insull W Jr, Pownall H, Smith L, Dunn K, Gotto AM Jr, Ballantyne CM. Levels of soluble cell adhesion molecules in patients with dyslipidemia. Circulation 1996;93:1334-1338.
- Summary In summary, the evidence that atherosclerosis is an inflammatory disorder is overwhelming and now accepted by virtually all investigators in the field. It is also widely accepted that LDL are subject to a variety of proinflammatory modifications that may play a large role in their atherogenicity. In addition, the protective effect of HDL is now recognized as having at least some anti-inflammatory components.
- Slide 28. Conclusions Strategies that reduce the proinflammatory modifications to LDL may indeed be very useful in reducing atherosclerosis, and there is a lot of research continuing along these directions. Also, strategies that increase the anti-inflammatory properties of HDL, especially by changing the phospholipid composition towards a more anti-inflammatory composition, may reduce atherosclerosis. However, these conclusions are still tentative, and we need more research. Keywords: inflammation, HDL, LDL Slide type: text
- HDL as a Therapeutic Target
- Is HDL-C simply a marker of increased cardiovascular risk? Low HDL-C levels are commonly found in patients who smoke, who are sedentary or obese, who are insulin resistant or diabetic, who have high triglycerides, or who have chronic inflammatory disorders. Part of the predictive nature of low HDL-C could be related to the fact that it is associated with other cardiovascular risk factors. This raises the question of whether HDL-C is in fact directly protective or simply a marker of cardiovascular risk.
- Production of apo A-I by liver and intestine The best data indicating that HDL is directly protective come from animal models in which the liver has been engineered to overproduce apolipoprotein (apo) A-I, the major protein in HDL.
- Increased apo A-I production is antiatherogenic in animals Studies in transgenic mice and rabbits have clearly established that overexpression of apo A-I reduces the initiation and progression of atherosclerosis. Studies using somatic gene transfer to liver in mice have demonstrated regression of pre-existing atherosclerotic lesions.
- HDL metabolism as a therapeutic target: potential strategies (I) When thinking about HDL as a therapeutic target for atherosclerosis, one may think of three categories of intervention. The one that is most supported by animal data is intervention to increase apo A-I production.
- Approaches to increasing apo A-I production Multiple approaches to increasing apo A-I production are in development in preclinical animal models, and some are in early clinical trials. Perhaps the most desirable approach would be a small molecule that upregulates apo A-I gene transcription. Another approach is the intravenous infusion of a recombinant apo A-I protein. A clinical trial on apo A-IMilano is currently in progress. Administration of peptides based on apo A-I sequence has been shown to reduce atherosclerosis in mice. Finally, the concept of using somatic gene transfer of apo A-I DNA to a tissue in which apo A-I could be made and secreted is attractive and is being piloted in animal studies.
- HDL metabolism as a therapeutic target: potential strategies (II) Another approach to targeting HDL would be to promote the process of reverse cholesterol transport.
- HDL and reverse cholesterol transport HDL is believed to protect against atherosclerosis at least in part through the process of reverse cholesterol transport, whereby excess free cholesterol (FC) is removed from cells in peripheral tissues, such as macrophages within the arterial wall, and returned to the liver for excretion in the bile. FC is generated in part by the hydrolysis of intracellular cholesteryl ester (CE) stores. Several key molecules play a role in reverse cholesterol transport, including ATP-binding cassette protein A1 (ABCA1), lecithin:cholesterol acyltransferase (LCAT), and scavenger receptor class-B, type I (SR-BI). Promotion of this pathway could in theory help reduce atherosclerosis.
- Regulation of cholesterol efflux in the macrophage A great deal has been learned about the regulation of cholesterol efflux in the macrophage. The cellular transporter ABCA1 is a critical protein that transports excess free cholesterol (FC) out of the cell to an acceptor, lipid-poor apo A-I. ABCA1 gene transcription is regulated by the nuclear receptor heterodimer liver X receptor/retinoid X receptor (LXR/RXR). Cellular oxysterols appear to be one of the endogenous ligands for LXR and promote the transcription of ABCA1. Oxysterols are generated from free cholesterol. Presumably, this represents a homeostatic mechanism by which macrophages rid themselves of excess free cholesterol. LXR gene transcription is also influenced by both peroxisome proliferator-activated receptor (PPAR-) and PPAR-.
- Pharmacologic manipulation of cholesterol efflux These discoveries have led to interest in pharmacologic manipulation of cholesterol efflux in the macrophage. Both fibrates, which are PPAR- agonists, and thiazolidinediones (TZDs), or glitazones, which are PPAR- agonists, are already on the market and may raise HDL and reduce atherosclerosis in part through this mechanism. New agents are also being developed that target the PPARs. Agents are also being developed that target LXR or RXR as potential strategies for upregulating ABCA1 and promoting cholesterol efflux.
- HDL as a therapeutic target: potential strategies (III) A third strategy for increasing HDL could be to delay the catabolism of HDL, thereby raising the levels in plasma.
- Mechanisms other than reverse cholesterol transport by which HDL may be antiatherogenic It is important to keep in mind that reverse cholesterol transport is only one mechanism by which HDL may directly protect against atherosclerosis. There are a variety of other properties of HDL that have been described, primarily in in vitro studies, which could theoretically contribute to the antiatherogenic effect of HDL. If these properties are indeed operative, a strategy that raises HDL, even if it does not promote reverse cholesterol transport, could theoretically be effective against atherosclerosis.
- HDL metabolism: intravascular remodeling of HDL Delaying the catabolism of HDL requires a sophisticated understanding of HDL metabolism. One concept in HDL metabolism is that of intravascular remodeling, by which larger HDL particles are converted to smaller particles. These smaller particles are at higher likelihood of being removed, at least in part, through the kidney. Inhibition of remodeling would be expected to lead to larger HDL particles and higher levels of both HDL and apo A-I.
- HDL metabolism: role of hepatic lipase Hepatic lipase is the best established molecule responsible for intravascular remodeling. It converts the larger HDL2 to the smaller HDL3. In theory, inhibition of hepatic lipase would be expected to increase HDL and apo A-I levels.
- HDL metabolism: role of CETP Another key protein involved in the intravascular remodeling of HDL is the cholesteryl ester transfer protein (CETP). CETP transfers cholesteryl esters (CE) from HDL to the apo B–containing lipoproteins, very low density lipoprotein (VLDL) and LDL. CETP has a major effect on the metabolism of HDL.
- HDL metabolism in CETP deficiency Genetic deficiency in CETP has been shown to be associated with exceptionally elevated levels of HDL-C and apo A-I, due to delayed catabolism of HDL. This led to the concept that inhibition of CETP might be a pharmacologic strategy for raising HDL.
- Inhibition of CETP by JTT-705 in cholesterol-fed rabbits significantly reduced aortic atherosclerosis An inhibitor of CETP, JTT-705, significantly reduced atherosclerosis in cholesterol-fed rabbits. This supports the concept that inhibition of CETP may reduce atherosclerosis. Reference: Okamoto H, Yonemori F, Wakitani K, Minowa T, Maeda K, Shinkai H. A cholesteryl ester transfer protein inhibitor attenuates atherosclerosis in rabbits. Nature 2000;406:203-207.
- HDL metabolism: influence of CETP inhibition Therefore, pharmacologic inhibition of CETP would be expected to raise levels of HDL-C and apo A-I. The impact of CETP inhibition on atherosclerosis in humans remains to be determined. CETP inhibitors are in clinical trials.
- Management of low HDL-C The ATP III guidelines made recommendations about the management of patients with low HDL-C. Therapeutic lifestyle changes such as weight reduction and increased physical activity are the cornerstone of therapy. LDL-C remains the primary target of pharmacologic therapy. Non-HDL-C is a secondary target of therapy in patients with triglycerides 200 mg/dL or higher. Selected patients may be considered for HDL-raising therapy with nicotinic acid or fibrates. Reference: Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486-2497.
- Management of low HDL-C: therapeutic lifestyle changes Therapeutic lifestyle changes are the cornerstone of managing patients with low HDL-C. Smoking cessation, regular aerobic exercise, and weight loss are all important. Alcohol does raise levels of HDL-C, though its clinical role is uncertain; in general, the prescription of alcohol for the goal of HDL-raising is discouraged.
- Management of low HDL-C: pharmacologic therapy: statins With regard to pharmacologic therapy in patients with low HDL-C, there are several considerations. The first category of lipid-altering drugs to be considered in most patients with low HDL-C is statins.
- Management of low HDL-C: pharmacologic therapy: fibrates A second category of medications to be considered in patients with low HDL-C is fibrates.
- Management of low HDL-C: pharmacologic therapy: niacin The third category of medication for consideration in patients with low HDL is niacin.
- Management of low HDL-C: combination therapy Combination therapy is often a consideration in patients with low HDL-C. The majority of these patients are candidates for statins as initial therapy, but still have low HDL-C levels even after treatment with statins.
- Summary In summary, LDL-C remains the primary goal of lipid-altering therapies, but HDL-C is an important risk factor. Even small increases in HDL-C may confer substantial benefit. Intervention to raise HDL-C levels should be considered in high-risk individuals.
- Approach to the patient with low HDL-C This demonstrates a fairly typical case of a 48-year-old man with the metabolic syndrome and coronary heart disease. After therapeutic lifestyle changes and a starting dose of a statin, his lipids are as shown here. His LDL-C is at target (&lt;100 mg/dL), but because triglycerides are &gt;200 mg/dL, non-HDL-C should be calculated. In this patient, the non-HDL-C is 147 mg/dL, which is higher than the target of &lt;130 mg/dL for patients in this risk category. Therefore, additional therapy is indicated. The HDL-C remains quite low at 32 mg/dL. Options would be intensification of statin therapy, addition of niacin to the statin, or addition of a fibrate to the statin. No clinical outcome trials have addressed whether one of these options is better than another.