Primary Maternal Care: The puerperium and family planning
- 1. 6 The puerperium and family planning Before you begin this unit, please take the THE PUERPERIUM corresponding test at the end of the book to assess your knowledge of the subject matter. 6-1 What is the puerperium? Objectives The puerperium is the period from the end of the third stage of labour until most of the patient’s organs have returned to their pre- When you have completed this unit you pregnant state. should be able to: • Define the puerperium and list the 6-2 How long does the puerperium last? physical changes which occur during the The puerperium starts when the placenta is puerperium. completely delivered and lasts for 6 weeks. • Manage the normal puerperium. However, some organs may only return • Assess a patient at the 6 week postnatal to their pre-pregnant state weeks or even visit. months after the 6 weeks have elapsed (e.g. the • Diagnose and manage the various ureters). Other organs never regain their pre- pregnant state (e.g. the perineum). causes of puerperal pyrexia. • Recognise the puerperal psychiatric It is important for the midwife or doctor disorders. to assess whether the patient has returned, as closely as possible, to normal health and • Diagnose and manage secondary activity by the end of the puerperium. postpartum haemorrhage. • Teach the patient the concept of ‘the The puerperium starts when the placenta is mother as a monitor’. delivered and lasts for 6 weeks. • Explain the wider meaning of family planning and give contraceptive 6-3 Why is the puerperium important? counselling. 1. The patient recovers from her labour, • List the health benefits, efficiency, which often leaves her tired and even contraindications and side effects of the exhausted. There is, nevertheless, a feeling various contraceptive methods. of great relief and happiness • Advise a postpartum patient on the most 2. The patient undergoes what is probably the appropriate method of contraception. most important psychological experience of
- 2. THE PUERPERIUM AND FAMILY PLANNING 105 her life, as she realises that she is responsible an enema on admission in labour is of for another human being, her infant. no advantage to her and contributes to 3. Breastfeeding should be established. constipation in the puerperium. 4. The patient should decide, with the 4. Urinary tract. guidance of a midwife or doctor, on an • Retention of urine is common and appropriate contraceptive method. may result from decreased tone of the bladder in pregnancy and oedema of 6-4 What physical changes the urethra following delivery. Dysuria occur in the puerperium? (discomfort or pain) and difficulty in passing urine may lead to complete Almost every organ undergoes change in the urinary retention or retention with puerperium. These adjustments range from overflow incontinence. A full bladder mild to marked. Only those changes which are will interfere with uterine contraction. important in the management of the normal • A diuresis usually occurs on the puerperium following discharge from the second or third day of the puerperium. hospital or clinic (midwife obstetric unit– In oedematous patients it may start MOU) will be described here. immediately after delivery. 1. Skin. • Stress incontinence (a leak of urine) • The increased pigmentation of the face, is common when the patient laughs abdominal wall and vulva lightens but or coughs. It may first be noted the areolae may remain darker than during the puerperium or follow they were before pregnancy. stress incontinence which was present • With the onset of diuresis (increased during pregnancy. Often stress amount of urine passed) the general incontinence becomes worse initially puffiness and any oedema disappear in but tends to improve with time and a few days. with pelvic floor exercises. • Marked sweating may occur for some Pelvic floor exercises are also known as days. pinch or ‘knyp’ exercises. The muscles that 2. Abdominal wall. are exercised are those used to suddenly • The abdominal wall is flaccid (loose stop a stream of urine midway through and wrinkled) and some separation micturition. These muscles should be (divarication) of the abdominal tightened, as strongly as possible, 10 times muscles occurs. in succession on at least 4 occasions a day. • Pregnancy marks (striae gravidarum), 5. Blood. where present, do not disappear but do • The haemoglobin concentration tend to become less red in time. becomes stable around the 4th day of 3. Gastrointestinal tract. the puerperium. • Thirst is common. • The platelet count is raised and the • The appetite varies from anorexia to platelets become more sticky from the ravenous hunger. 4th to 10th day after delivery. These • There may be flatulence (excess wind). and other changes in the clotting • Many patients are constipated as a (coagulation) factors may cause result of decreased tone of the bowel thrombo-embolism in the puerperium. during pregnancy and, decreased food 6. Breasts. intake during labour. They may also Marked changes occur during the have passed stool during labour and puerperium with the production of milk delivery. Constipation is common 7. Genital tract. in the presence of an episiotomy or Very marked changes occur in the genital painful haemorrhoids. Giving a patient tract during the puerperium:
- 3. 106 PRIMAR Y MATERNAL CARE • Vulva: The vulva is swollen and MANAGEMENT OF congested after delivery, but these features rapidly disappear. Tears and/or THE PUERPERIUM an episiotomy usually heal easily. • Vagina: Immediately after delivery The management of the puerperium may be the vagina is large, smooth walled, divided into 3 stages: oedematous and congested. It rapidly 1. The management of the first hour after shrinks in size and rugae return by the delivery of the placenta (sometimes called third week. The vaginal walls remain the fourth stage of labour). laxer than before and some degree of 2. The management of the rest of the vaginal prolapse (cystocoele and/or puerperium. rectocoele) is common after a vaginal 3. The 6 week postnatal visit. delivery. Small vaginal tears, which are very common, usually heal in 7 to 10 days. 6-5 When should a postpartum • Cervix: After the first vaginal delivery patient be allowed to go home? the circular external os of the nullipara This will depend on: becomes slit like. For the first few 1. Whether the patient had a normal days after delivery the cervix remains pregnancy and delivery. partially open, admitting 1 or 2 fingers. 2. The circumstances of the hospital or clinic By the 7th day postpartum the cervical where the patient was delivered. os will have closed so that a finger can no longer be passed through it. • Uterus: The most important change 6-6 When should a patient be occurring in the uterus is involution. allowed to go home following a After delivery the uterus is about the normal pregnancy and delivery? size of a 20 week pregnancy. By the end A patient who has had a normal pregnancy of the first week it is about 12 weeks and delivery may be allowed to go home about in size. At 14 days the fundus of the 6 hours after the birth of her infant, provided: uterus should no longer be palpable above the symphysis pubis. After 6 1. The observations done on the mother and weeks it has decreased to the size of a infant since delivery have been normal. normal multiparous uterus, which is 2. The mother and infant are normal on slightly larger than a nulliparous one. examination, and the infant is sucking well. This remarkable decrease in size is the 3. The patient is able to attend her nearest result of contraction and retraction clinic on the day after delivery (day 1) and of the uterine muscle. The normally then again on days 3 and 5 after delivery involuting uterus should be firm and for postnatal care, or be visited at home non-tender. The decidua of the uterus by a midwife on those days. Primigravidas necroses (dies), due to ischaemia, and is should be seen again on day 7, especially to shed as the lochia. The average duration ensure that breastfeeding is well established. of red lochia is 24 days. Thereafter, the A patient should only be discharged home lochia becomes straw coloured. Normal after delivery if no abnormalities are lochia has a typical, non-offensive smell. found when the following examinations Offensive lochia is always abnormal. are performed: • A general examination, paying particular attention to the: • Pulse rate. • Blood pressure.
- 4. THE PUERPERIUM AND FAMILY PLANNING 107 • Temperature. 6-8 How will the circumstances at a clinic or • Haemoglobin concentration. hospital influence the time of discharge? • An abdominal examination, paying 1. Some clinics have no space to accom- particular attention to the state of modate patients for longer than 6 hours contraction and/or tenderness of the uterus. after delivery. Therefore, patients who • An inspection of the episiotomy site and cannot be discharged safely at 6 hours will the amount, colour and odour of the lochia. have to be transferred to a hospital. • Patients who received no antenatal care 2. Some hospitals manage patients who live and delivered without having any screening in remote areas where follow-up is not tests, must have a rapid syphilis test and a possible. These patients will have to be kept rapid test for Rhesus grouping. Counselling in hospital longer before discharge. for HIV testing must also be done. It is important to arrange for suitable contra- ception before the patient is discharged home. 6-9 What postnatal care should be given during the puerperium after the The Essential Postnatal Obstetric Care (EPOC) patient has left the hospital or clinic? card with the mother’s and infant’s discharge information could now be completed. If any Ideally, visits for postnatal care must be of the shaded blocks are ticked, treatment is scheduled for the day following discharge required or the mother needs to be referred (day 1), day 3 and day 5 or 6. Limited health to the next level of care. The checklist will care facilities or long distances may require the again be used during the day-5 or -6 visit to visits to be limited to a single visit on day 5 or 6. check that all the important tasks have been The following observations must be done on completed (i.e. as a quality control tool). the mother: 1. Assess the patient’s general condition. 6-7 When should a patient be 2. Ask about problems with breathing and discharged from hospital following a coughing. complicated pregnancy and delivery? 3. Observe the pulse rate, blood pressure and This will depend on the nature of the temperature. complication and the method of delivery. For 4. Determine the height of the uterine fundus example: and assess whether any uterine tenderness is present. 1. A patient with pre-eclampsia should 5. Assess whether the amount of vaginal be kept in hospital until her blood bleeding is more than normal. pressure has returned to normal or is well 6. Asses the amount, colour and odour of the controlled with oral drugs. lochia. 2. A patient who has had a caesarean section 7. Check whether the episiotomy is healing will usually stay in hospital for 2 days or satisfactorily. longer. 8. Ask if the patient passes urine normally 3. A patient who has had a postpartum and enquire about any urinary symptoms. haemorrhage must be kept in hospital for Reassure the patient if she has not passed a at least 24 hours to ensure that her uterus stool by day 5. is well contracted and that there is no 9. Measure the haemoglobin concentration if further bleeding. the patient appears pale. 4. HIV-positive patients are at increased risk 10. Assess the condition of the patient’s breasts for infections. Careful examination for and nipples. Determine whether successful any signs of infection is required and the breastfeeding has been established. patients should be kept in hospital or the delivery clinic for 24 hours.
- 5. 108 PRIMAR Y MATERNAL CARE The following observations must be done on 5. Any special arrangements for the next the infant: pregnancy and delivery. 6. When to start coitus again. Usually coitus 1. Assess whether the infant is feeding well can be started 3 to 4 weeks postpartum and is satisfied after a feed. when the episiotomy or tears have healed. 2. Assess whether the infant appears well and is thriving. Patient education is an important and often 3. Check whether the infant is jaundiced. neglected part of postnatal care. 4. Examine the umbilical stump for signs of infection. 5. Examine the eyes for conjunctivitis. 6-12 When should a patient be seen again 6. Ask whether the infant has passed urine after postnatal care has been completed? and stool. The postnatal visit is usually held 6 weeks after The successful establishment of breastfeeding is delivery. By this time almost all the organ one of the most important goals of patient care changes which occurred during pregnancy should have disappeared. during the puerperium. The EPOC card for the day 5 to 6 visit could now be completed. The checklist will again be THE SIX WEEK used during the 6 weeks visit. POSTNATAL VISIT 6-10 How can you help to establish successful breastfeeding? 6-13 Which patients need to attend a 6 week postnatal clinic? By providing patient education and motivation. This should preferably start Patients with specific problems that need to be before pregnancy and continue throughout followed up 6 weeks postpartum, e.g. patients the antenatal period and after delivery. who were discharged with hypertension need Encouragement and support are very to come back to have their blood pressure important during the first weeks after delivery. measured. Patients who are healthy may be The important role of successful breastfeeding referred directly to the mother and child in lowering infant mortality in poor health clinics for follow up and need not communities must be remembered. attend a special 6 week postnatal clinic. 6-11 Which topics should you 6-14 What are the objectives of include under patient education the 6-week postnatal visit? in the puerperium? It is important to identify the reason why the Patient education regarding herself, her patient was asked to attend the clinic and to infant and her family should not start during determine whether: the puerperium, but should be part of any 1. The patient is healthy and has returned to woman’s general education, starting at school. her normal activities. Topics which should be emphasised in patient 2. The infant is well and growing normally. education in the puerperium include: 3. Breastfeeding has been satisfactorily 1. Personal and infant care. established. 2. Offensive lochia, fever or severe abdominal 4. Contraception has been arranged to the pain must be reported immediately. patient’s satisfaction. 3. The ‘puerperal blues’. 5. The patient has been referred to a maternal 4. Family planning and safer sex. and child health clinic for further care.
- 6. THE PUERPERIUM AND FAMILY PLANNING 109 6. The patient has any questions about for a clinical assessment and CD4 count herself, her infant or her family. every 6 months. 2. Patients on antiretroviral treatment must 6-15 How should the 6 week be encouraged to be compliant with regular postnatal visit be conducted? clinic visits and adherence to medication. 3. Blood must be taken from the infant for a 1. The patient is asked how she and her infant DNA PCR test and an appointment made have been since the last postnatal care visit. so that the infant’s result can be obtained 2. The patient is then examined. On exam- and further management planned. The ination pay particular attention to the blood DNA PCR will determine whether the pressure and breasts, and look for signs infant is HIV infected. of anaemia. An abdominal examination 4. The essential postpartum care (EPOC) is followed by a speculum examination to card (Figure 61-I) for the 6 weeks visit check whether the episiotomy, vulval or could now be completed.d. vaginal tears have healed. 3. A cytology smear of the cervix should be taken if the patient is 30 years or older and has not previously had a normal cervical PUERPERAL PYREXIA smear. A cervical smear should also be taken on any woman who has previously 6-17 When is puerperal pyrexia present? had an abnormal smear. 4. The haemoglobin is measured and the A patient has puerperal pyrexia if her oral urine tested for glucose and protein. temperature rises to 38 °C or higher during 5. Attention must be given to any specific the puerperium. reason why the patient is being followed up, e.g. arrangements for the management 6-18 Why is puerperal pyrexia important? of patients who remain hypertensive after Because it may be caused by serious delivery. complications of the puerperium. Breast- 6. The patient is given health education. It feeding may be interfered with. The patient should again be remembered to ask her may become very ill or even die. whether she has any questions she would like to ask. Puerperal pyrexia may be caused by a serious If the patient and her infant are both well, they complication of the puerperium. are referred to their local maternal and child health clinic for further follow-up. 6-19 What are the causes of A patient and her infant should only be discharged puerperal pyrexia? if they are both well and have been referred to 1. Genital tract infection. the local maternal and child health clinic, and the 2. Urinary tract infection. patient has received contraceptive counselling. 3. Mastitis or breast abscess. 4. Thrombophlebitis (superficial vein thrombosis). 6-16 What additional management is 5. Respiratory tract infection. needed for HIV-positive patients? 6. Other infections. 1. Patients that do not require antiretroviral treatment (CD4 count 250 cells/ml or more and stage 1 or 2 disease) must be encouraged to attend their nearest clinic
- 7. 110 PRIMAR Y MATERNAL CARE 6-20 What is the cause of 6-23 How must a patient with genital tract infection? offensive lochia be managed? Genital tract infection (or puerperal sepsis) 1. If the patient has a pyrexia she must be is caused by bacterial infection of the raw admitted to hospital. placental site or lacerations of the cervix, 2. If the patient has a normal temperature vagina or perineum. and normal involution of her uterus, she can be managed as an out patient with oral 6-21 How should you diagnose ampicillin and metronidazole (Flagyl). genital tract infection? Offensive lochia is an important sign of genital 1. History. tract infection. If one or more of the following is present: • Preterm or prelabour rupture of the 6-24 How should you diagnose membranes, a long labour, operative a urinary tract infection? delivery or incomplete delivery of the placenta or membranes may have 1. History. occurred. • The patient may have been catheterised • The patient will feel generally unwell. during labour or in the puerperium. • Lower abdominal pain. • Lower abdominal pain and/or pain in 2. Examination. the lower back over one or both the • Pyrexia, usually developing within the kidneys (the loins). first 24 hours after delivery. Rigors may • Dysuria and frequency. However, these occur. are not reliable symptoms of urinary • Marked tachycardia. tract infection. • Lower abdominal tenderness. 2. Examination. • Offensive lochia. • Pyrexia, often with rigors (shivering). • The episiotomy wound or perineal or • Tachycardia. vaginal tears may be infected. • Suprapubic and flank tenderness and/or tenderness, especially to light 6-22 How should you manage percussion, over the kidneys (punch genital tract infection? tenderness in the renal angles). 3. Side room and special investigations. These patients require admission to a hospital • Microscopy of a midstream or catheter urgently and must be referred. While waiting specimen of urine usually shows large to be transferred treatment could be initiated: numbers of pus cells and bacteria. • Measures to bring down the • Culture and sensitivity tests of the temperature, e.g. tepid sponging. urine must be done if the facilities are • Analgesia, e.g. paracetamol (Panado) available. 1 g (2 adult tablets) orally 6 hourly. The presence of pyrexia and punch tenderness • Intravenous fluids. in the renal angles indicates an upper renal • Broad-spectrum antibiotics, e.g. tract infection and a diagnosis of acute ampicillin and metronidazole (Flagyl). pyelonephritis must be made. Antibiotic treatment must be started before transfer.
- 8. THE PUERPERIUM AND FAMILY PLANNING 111 6-25 How should you manage a patient 6-29 How should you diagnose a with a urinary tract infection? lower respiratory tract infection? 1. Prevention. A lower respiratory tract infection, such as • Avoid catheterisation whenever possible. acute bronchitis or pneumonia, is diagnosed If catheterisation is essential, it must be as follows: done with strict aseptic precautions. 1. History. 2. Treatment. • The patient may have had general These patients require admission to a anaesthesia with endotracheal hospital urgently and must be referred. intubation, e.g. for a caesarean section. While waiting to be transferred treatment • Cough, which may be productive. could be initiated: • Pain in the chest. • Measures to bring down the • A recent upper respiratory tract temperature, e.g. tepid sponging. infection. • Analgesia, e.g. paracetamol (Panado) 2. Examination. 1 g (2 adult tablets) orally 6 hourly. • Pyrexia. • Intravenous fluids. • Tachypnoea (breathing rapidly). Antibiotics should not be given to a patient • Tachycardia. 3. Special investigations. with puerperal pyrexia until she has been fully • A chest X-ray is useful in diagnosing investigated. pneumonia. 6-26 What is superficial vein 6-30 How should you manage a patient thrombophlebitis? with a lower respiratory tract infection? This is a non-infective inflammation and 1. Treatment thrombosis of the superficial veins of the These patients require admission to a leg or forearm where an infusion was given. hospital urgently and must be referred Thrombophlebitis commonly occurs during unless the infection is very mild. While the puerperium, especially in varicose veins. waiting to be transferred treatment could be initiated: 6-27 How should you diagnose • Oxygen if required. superficial leg vein thrombophlebitis? • Ampicillin orally or intravenously depending on the severity of the 1. History. infection. • Painful swelling of the leg or arm. • Analgesia, e.g. paracetamol (Panado) • Presence of varicose veins. 1 g. 2. Examination. 2. Special investigations: • Pyrexia. • Send a sample of sputum for • Tachycardia. microscopy, culture and sensitivity • Presence of a localised area of the leg or testing if possible. arm which is swollen, red and tender. 6-31 Which other infections may 6-28 How should you manage a patient cause puerperal pyrexia? with superficial vein thrombophlebitis? Tonsillitis, influenza and any other acute 1. Give analgesia, e.g. aspirin 300 mg (1 adult infection, e.g. acute appendicitis or meningitis. tablet) 6 hourly. 2. Support the leg with an elastic bandage. 3. Encourage the patient to walk around.
- 9. 112 PRIMAR Y MATERNAL CARE 6-32 What should you do if a patient 6-34 Why is it important to recognise the presents with puerperal pyrexia? various puerperal psychiatric disorders? 1. Ask the patient what she thinks is wrong 1. The ‘puerperal blues’ are very common with her. in the first week after delivery, especially 2. Specifically ask for symptoms which point on day 3. The patient feels miserable and to: cries easily. Although the patient may be • An infection of the throat or ears. very distressed, all that is required is an • Mastitis or breast abscess. explanation, reassurance, and a caring, • A chest infection. sympathetic attitude and emotional support. • A urinary tract infection. The condition improves within a few days. • An infected abdominal wound if the 2. Postnatal depression is much more common patient had a caesarean section or a than is generally realised. The onset is puerperal sterilisation. later than ‘puerperal blues’ and it may last • Genital tract infection. for months or even years. The patients • Superficial leg vein thrombophlebitis. may need to be referred to a psychiatrist. 3. Examine the patient systematically, Patients with postnatal depression usually including the: present with a depressed mood that cannot • Throat and ears. be relieved, a lack of interest in their • Breasts. surroundings, a poor or excessive appetite, • Chest. sleeping difficulties, feelings of inadequacy, • Abdominal wound, if present. guilt and helplessness, and sometimes • Urinary tract. suicidal thoughts. • Genital tract. 3. Puerperal psychosis is an uncommon but • Legs, especially the calves. very important condition. The onset is 4. Perform the necessary special usually acute and an observant attendant investigations, but always send off a: will notice the sudden and marked change • Endocervical swab. in the patient’s behaviour. She may rapidly • Midstream or catheter specimen of pose a threat to her infant, the staff and urine. herself. Such a patient must be referred 5. Start the appropriate treatment. urgently to a psychiatrist and will usually need admission to a psychiatric unit. If a patient presents with puerperal pyrexia Patients with puerperal psychosis are the cause of the pyrexia must be found and unable to care for themselves or their appropriately treated. infants. They are often disoriented and paranoid and may have hallucinations. They may also be severely depressed or manic. PUERPERAL PSYCHIATRIC DISORDERS SECONDARY POSTPARTUM HAEMORRHAGE 6-33 Which are the puerperal psychiatric disorders? 6-35 What is secondary 1. The ‘puerperal blues’. postpartum haemorrhage? 2. Temporary postnatal depression. This is any amount of vaginal bleeding, other 3. Puerperal psychosis. than the normal amount of lochia, occurring after the first 24 hours postpartum until the end of the puerperium. It commonly occurs
- 10. THE PUERPERIUM AND FAMILY PLANNING 113 between the fifth and fifteenth days after • Give Syntometrine 1 ml intra- delivery. muscularly or 20 units oxytocin in an intravenous infusion if excessive 6-36 Why is secondary postpartum haemorrhage is present. haemorrhage important? 6-40 What may you find on physical 1. A secondary postpartum haemorrhage examination to suggest that retained may be so severe that it causes shock. pieces of placenta or membranes 2. Unless the cause of the secondary are the cause of a secondary postpartum haemorrhage is treated, the postpartum haemorrhage? vaginal bleeding will continue. 1. The uterus will be involuting slower than 6-37 What are the causes of secondary usual. postpartum haemorrhage? 2. Even though the patient may be more than 7 days postpartum, the cervical os will have 1. Genital tract infection with or without remained open and a finger can be passed retention of a piece of placenta or part of the through the cervix. membranes. This is the commonest cause. 2. Separation of an infected slough in a cervical or vaginal laceration. 3. Breakdown (dehiscence) of a caesarean SELF-MONITORING section wound of the uterus. However, the cause is unknown in up to 6-41 What is meant by the concept half of these patients. of ‘the mother as a monitor’? 6-38 What clinical features should alert you This is a concept where the patient is made to the possibility of the patient developing aware of the many ways in which she can secondary postpartum haemorrhage? monitor her own, as well as her fetus’ or infant’s 1. A history of incomplete delivery of the wellbeing, during pregnancy, in labour and in placenta and/or membranes. the puerperium. This has two major advantages: 2. Unexplained puerperal pyrexia. 1. The patient becomes much more involved 3. Delayed involution of the uterus. in her own perinatal care. 4. Offensive and/or persistently red lochia. 2. Possible complications will be reported by the patient at the earliest opportunity. 6-39 How should you manage a patient with secondary postpartum haemorrhage? 6-42 How can the patient act as a 1. Treatment. monitor in the puerperium? These patients require admission to a The patient must be encouraged to report hospital and must be referred unless the the following complications as soon as she haemorrhage is very mild. While waiting to becomes aware of them: be transferred treatment could be initiated: • Review of the clinical notes with regard 1. Maternal complications. to completeness of the placenta and • Symptoms of puerperal pyrexia. membranes. • Breakdown of an episiotomy. • Obtain an endocervical swab for • Breastfeeding problems. bacteriology. • Excessive or offensive lochia. • Give ampicillin and metronidazole • Recurrence of vaginal bleeding, i.e. (Flagyl) orally. secondary postpartum haemorrhage. • Prolonged postnatal depression.
- 11. 114 PRIMAR Y MATERNAL CARE 2. Complications in the infant. the parents. It is then continued at school and • Poor feeding or other feeding throughout the rest of the individual’s life. problems. • Lethargy. 6-45 Who needs contraceptive counselling? • Jaundice. • Conjunctivitis. Every person who is sexually active, or • Infection of the umbilical cord stump. who probably will soon become sexually active, needs contraceptive counselling (i.e. Each patient must be taught to monitor her own information and advice about birth control). wellbeing, as well as that of her fetus or infant. While the best time to advise a woman on contraception is before the first coitus, the antenatal and postdelivery periods provide an excellent opportunity to provide contraceptive FAMILY PLANNING IN counselling. Some patients will ask you for THE PUERPERIUM contraceptive advice. However, you will often have to first motivate a patient to accept contraception before you can advise her about 6-43 What is family planning? an appropriate method of contraception. Family planning is far more than simply birth 6-46 How should you motivate a patient control, and aims at improving the quality of life to accept contraception after delivery? for everybody. Family planning is an important part of primary health care and includes: A good way to motivate a patient to accept contraception is to discuss with her, or 1. Promoting a caring and responsible preferably with both her and her partner, the attitude to sexual behaviour. health and socio-economic effects further 2. Ensuring that every child is wanted. children could have on her and the rest of the 3. Encouraging the planning and spacing family. Explain the immediate benefits of a of the number of children according to smaller, well-spaced family. a family’s home conditions and financial income. It is generally hopeless to try and promote 4. Providing the highest quality of maternal contraception by itself. To gain individual and child care. and community support, family planning 5. Educating the community with regard must be seen as part of total primary health to the disastrous effects of unchecked care. A high perinatal or infant mortality population growth on the environment. rate in a community is likely to result in a rejection of contraception. It is essential to obtain prior community acceptance of, and promote community 6-47 How should you give participation in, any family planning contraceptive advice after delivery? programme if the programme is to succeed in that community. There are 5 important steps which should be followed: 6-44 Who requires family Step 1: Discussion of the patient’s future planning education? reproductive career Because family planning aims at improving Ideally a woman should consider and plan the quality of life for everybody, every person, her family before her first pregnancy, just as female or male, requires family planning she would have considered her professional education. Such education should ideally start career. Unfortunately in practice this hardly during childhood and be given in the home by ever happens and many women only discuss
- 12. THE PUERPERIUM AND FAMILY PLANNING 115 their reproductive careers for the first time Step 4: Selection of the most appropriate when they are already pregnant or after the alternative method of contraception birth of the infant. The selection of the most suitable alternative When planning her family the woman (or method of contraception after delivery will preferably the couple) should decide on: depend on a number of factors including the patient’s wishes, her age, the risk of side effects 1. The number of children wanted. and whether or not a very effective method of 2. The time intervals between pregnancies contraception is required. as this will influence the method of contraception used. Step 5: Counselling the patient once the 3. The contraceptive method of choice when contraceptive method has been chosen the family is complete. Virtually every contraceptive method has its Very often the patient will be unable or own side effects. It is a most important part unwilling to make these decisions immediately of contraceptive counselling to explain the after delivery. However, it is essential to discuss possible side effects to the patient. Expert contraception with the patient so that she can family planning advice must be sought if the plan her family. This should be done together local clinic is unable to deal satisfactorily with her husband and, where appropriate, with the patient’s problem. If family planning other members of her family or friends. method problems are not satisfactorily solved, the patient will probably stop using Step 2: The patient’s choice of a contraceptive any form of contraception. method The patient should always be asked which After delivery the reproductive career of each contraceptive method she would prefer as this patient must be discussed with her in order to will obviously be the method with which she is decide on the most appropriate method of family most likely to continue. planning to be used. Step 3: Consideration of contraindications to the patient’s preferred method 6-48 What contraceptive methods You must decide whether the patient’s choice can be offered after delivery? of a contraceptive method is suitable, taking 1. Sterilisation. Either tubal ligation (tubal into consideration: occlusion) or vasectomy. 1. The effectiveness of each contraceptive 2. Injectables (i.e. an intramuscular injection method. of depot progestogen). 2. The contraindications to each 3. Oral contraceptives. Either the combined contraceptive method. pill (containing both oestrogen and 3. The side effects of each contraceptive progestogen) or a progestogen-only pill method. (the ‘minipill’). 4. The general health benefits of each 4. An intra-uterine contraceptive device contraceptive method. (IUCD). 5. The condom. If the contraceptive efficiency of the preferred method is appropriate, if there are no Breastfeeding, spermicides alone, coitus contraindications to it, and if the patient is interruptus and the ‘safe period’ are all very prepared to accept the possible side effects, unreliable. All women should know about then the method chosen by the patient should postcoital contraception. be used. Otherwise proceed to step 4. Breastfeeding cannot be relied upon to provide postpartum contraception.
- 13. 116 PRIMAR Y MATERNAL CARE 6-49 How effective are the various • Forced or hasty decision. contraceptive methods? • Gynaecological problem requiring hysterectomy. Contraceptive methods for use after delivery 2. Injectables: may be divided into very effective and less • Depression. effective ones. Sterilisation, injectables, oral • Pregnancy planned within 1 year. contraceptives and intra-uterine contraceptive 3. Combined pills: devices are very effective. Condoms are less • A history of venous thrombo- effective contraceptives. embolism. • Age 35 years or more with risk factors 6-50 How effective is postcoital for cardiovascular disease (i.e. smoking). contraception? • Anyone of 50 or more years. 1. Norlevo, E Gen-C or Ovral are effective • Oestrogen-dependent malignancies within 5 days of unprotected sexual such as breast or uterine cancer. intercourse, but are more reliable the 4. Progestogen-only pill (minipill): earlier they are used. • None. 2. A copper intra-uterine contraceptive 5. Intra-uterine contraceptive device: device can be inserted within 6 days of • A history of excessive menstruation. unprotected intercourse. • Anaemia. 3. Postcoital methods should only be used in • Multiple sex partners when the risk of an emergency and not as a regular method genital infection is high. of contraception. • Pelvic inflammatory disease. 4. If Norlevo is used, one tablet should be • Immuno-compromised patients (i.e. taken as soon as possible after intercourse, AIDS). followed by another one tablet after exactly A menstrual abnormality is a contra- 12 hours. indication to any of the hormonal 5. If Ovral or E-Gen-C is used, two tablets are contraceptive methods (injectables, combined taken as soon as possible after intercourse, pill or progestogen-only pill) until the cause of followed by another two tablets exactly 12 the menstrual irregularity has been diagnosed. hours later. Thereafter, hormonal contraception may often The tablets for postcoital contraception often be used to correct the menstrual irregularity. cause nausea and vomiting which reduce However, during the puerperium a previous their effectiveness. These side effects are less history of menstrual irregularity before with Norlevo which contains no oestrogen. the pregnancy is not a contraindication to Therefore Norlevo is a more reliable method hormonal contraception. and should be used if available. Norlevo as a single dose method is available and on code in 6-52 What are the major side effects of the public sector in South Africa. the various contraceptive methods? Most contraceptive methods have side 6-51 What are the contraindications to effects. Some side effects are unacceptable to the various contraceptive methods? a patient and will cause her to discontinue The following are the common or important the particular method. However, in many conditions where the various contraceptive instances side effects are mild or disappear methods should not be used: with time. It is, therefore, very important to counsel a patient carefully about the side 1. Sterilisation: effects of the various contraceptive methods, • Marital disharmony. and to determine whether she would find • Psychological problems. any of them unacceptable. At the same time
- 14. THE PUERPERIUM AND FAMILY PLANNING 117 the patient may be reassured that some other • Progesterone-containing devices side effects will most likely become less or (Mirena) have fewer side effects disappear after a few months’ use. and reduce menstrual blood loss. These devices are expensive and not The major side effects of the various generally available in the public health contraceptive methods used after delivery are: sector facilities. 1. Sterilisation: 6. Condom: Tubal ligation and vasectomy have no • Decreased sensation for both partners. medical side effects and, therefore, • Not socially acceptable to everyone. should be highly recommended during counselling of patients who have completed If a couple have completed their family the their families. Menstrual irregularities are contraceptive method of choice is tubal ligation NOT a problem. However, about 5% of or vasectomy. women later regret sterilisation. 2. Injectables: Additional contraceptive precautions must be • Menstrual abnormalities, e.g. taken when the contraceptive effectiveness of amenorrhoea, irregular menstruation an oral contraceptive may be impaired, e.g. or spotting. diarrhoea or when taking antibiotics. There • Weight gain. is no medical reason for stopping a hormonal • Headaches. method periodically to ‘give the body a rest’. • Delayed return to fertility within a year of stopping the method. There is 6-53 What are the important health no evidence that fertility is reduced benefits of contraceptives? thereafter. 3. Combined pill: The main objective of all contraceptive • Reduction of lactation. methods is to prevent pregnancy. In developing • Menstrual abnormalities, e.g. spotting countries pregnancy is a major cause of between periods. mortality and morbidity in women. Therefore, • Nausea and vomiting. the prevention of pregnancy is a very important • Depression. general health benefit of all contraceptives. • Fluid retention and breast tenderness. Various methods of contraception have • Chloasma (a brown mark on the face). a number of additional health benefits. • Headaches and migraine. Although these benefits are often important, 4. Progestogen-only pill: they are not generally appreciated by many • Menstrual abnormalities, e.g. irregular patients and health-care workers: menstruation. • Headaches. 1. Injectables: • Weight gain. • Decrease in dysmenorrhoea. 5. Intra-uterine contraceptive device: • Less premenstrual tension. • Expulsion in 5–15 cases per 100 • Less iron-deficiency anaemia due to women who use the device for one year. decreased menstrual flow. • Pain at insertion. • No effect on lactation. • Dysmenorrhoea. 2. Combined pill: • Menorrhagia (excessive and/or • Decrease in dysmenorrhoea. prolonged bleeding). • Decrease in menorrhagia (heavy and/or • Increase in pelvic inflammatory prolonged menstruation). disease. • Less iron-deficiency anaemia. • Perforation of the uterus is uncommon. • Less premenstrual tension. • Ectopic pregnancy is not prevented. • Fewer ovarian cysts.
- 15. 118 PRIMAR Y MATERNAL CARE • Less benign breast disease. • An injectable, e.g. Depo-Provera or • Less endometrial and ovarian Petogen (12 weekly) or Nur-Isterate (8 carcinoma. weekly). 3. Progestogen-only pill: • A combined pill until 35 years of age if • No effect on lactation. there are risk factors for cardiovascular 4. Condom: disease, or until 50 years if these risk • Less risk of HIV infection and other factors are absent. sexually transmitted diseases. 5. Patients of 35 years or over without risk • Less pelvic inflammatory disease. factors for cardiovascular disease: • Less cervical intra-epithelial neoplasia. • Tubal ligation or vasectomy is the logical method. The condom is the only contraceptive method • A combined pill until 50 years. that provides protection against HIV infection. • An injectable until 50 years of age. • A progestogen-only pill until 50 years of age. 6-54 What is the most appropriate • An intra-uterine contraceptive device method of contraception for until 1 year after the periods have a patient after delivery? stopped, i.e. when there is no further The most suitable methods for the following risk of pregnancy. groups of patients are: 6. Patients of 35 years or over with risk factors for cardiovascular disease: 1. Lactating patients: • As above but NO combination pill. • An injectable, but not if a further pregnancy is planned within the next The puerperium is the most convenient time year. for the patient to have a bilateral tubal ligation • A progestogen-only pill (minipill) for 3 performed. months, then the combined pill. • An intra-uterine contraceptive device. Every effort should be made to provide Non-lactating patients can start the facilities for tubal ligation during the combined pill following one month’s use of puerperium for all patients who request a progesterone-only pill. sterilisation after delivery. 2. Teenagers and patients with multiple sexual partners: Remember that sperms may be present in • An injectable, as this is a reliable method the ejaculate for up to 3 months following even with unreliable patients who might vasectomy. Therefore, an additional forget to use another method. contraceptive method must be used during • Additional protection against HIV this time. infection by using a condom is essential. It is important to stress 6-55 What are the risk factors for that the patient should only have cardiovascular disease in women intercourse with a partner who is taking the combined pill? willing to use a condom. The risk of cardiovascular disease increases 3. HIV-positive patients: markedly in women of 35 or more years of • Condoms must be used in addition to age who have 1 or more of the following risk the appropriate contraceptive method factors: (dual contraception). 4. Patients whose families are complete: 1. Smoking. • Tubal ligation or vasectomy is the 2. Hypertension. logical choice. 3. Diabetes.
- 16. THE PUERPERIUM AND FAMILY PLANNING 119 4. Hypercholesterolaemia. time. However, pelvic floor exercises must 5. A personal history of cardiovascular disease. be explained to her as they will hasten improvement of her incontinence. She need Smoking is a risk factor for cardiovascular disease. not be worried about not having passed a stool as this is normal during the first few days of the puerperium. 6-56 When should an intra- uterine contraceptive device be inserted after delivery? 3. Why is the patient regretting her pregnancy and crying for It should not be inserted before 6 weeks as the no apparent reason? uterine cavity would not yet have returned to its normal size. At 6 weeks or more after She probably has the ‘puerperal blues’ which delivery there is the lowest risk of: are common in the puerperium. Listen sympathetically to the patient’s complaints 1. Pregnancy. and reassure her that she is managing well as 2. Expulsion. a mother. Also explain that her feelings are Postpartum patients choosing this method must normal and are experienced by most mothers. be discharged on an injectable contraceptive or progestogen-only pill until an intra-uterine 4. What educational topics must be contraceptive device has been inserted. discussed with the patient during this visit? 1. Family size and when she plans to have her next infant. CASE STUDY 1 2. Which contraceptive method she should use and how to use it correctly. A patient returns to a clinic for a visit 3 days 3. The care and feeding of her infant, after a normal first pregnancy and delivery. stressing the importance of breastfeeding. She complains of leaking urine when 4. Symptoms of a genital tract infection, coughing or laughing, and she is also worried i.e. offensive lochia, fever and lower that she has not passed a stool since the abdominal pain. delivery. She starts to cry and says that she 5. The time that coitus can be resumed. should not have fallen pregnant. Her infant Also ask about, and discuss, any other takes the breast well and sleeps well after each uncertainties which the patient may have. feed. On examination the patient appears well, her observations are normal, the uterus is the size of a 16 week pregnant uterus, and the lochia is red and not offensive. CASE STUDY 2 1. Is her puerperium progressing normally? Following a prolonged first stage of labour due to an occipito-posterior position, a patient Yes. The patient appears healthy with normal has a spontaneous vertex delivery in hospital. observations, and the involution of her uterus The placenta and membranes are complete. is satisfactory. There is no excessive postpartum blood loss and the patient is discharged home after 6 2. What should be done about hours. Within 24 hours of delivery the patient the patient’s complaints? is brought back to the clinic nearest to her home. She has a temperature of 39 °C, a pulse Stress incontinence is common during rate of 110 beats per minute and complains the puerperium. Therefore, the patient of a headache and lower abdominal pain. The must be reassured that it will improve over uterus is tender to palpation.
- 17. 120 PRIMAR Y MATERNAL CARE 1. What does the patient present with? made and the patient is given oral ampicillin. She is asked to come back to the clinic on day 7. Puerperal pyrexia. 1. Are you satisfied with the 2. What is the most likely cause diagnosis of puerperal pyrexia? of the puerperal pyrexia? No. Puerperal pyrexia is a clinical sign and Genital tract infection, i.e. puerperal sepsis. not a diagnosis. The cause of the pyrexia must This diagnosis is suggested by the general signs be found by taking a history, doing a physical of infection and the uterine tenderness. The examination and, if indicated, completing patient had a prolonged first stage of labour, special investigations. which is usually accompanied by a greater than usual number of vaginal examinations and, therefore, predisposes to genital tract infection. 2. What is the most likely cause of the patient’s pyrexia? 3. Was the early postnatal management An upper urinary tract infection as suggested of this patient correct? by the pyrexia, rigors, lower abdominal pain and tenderness over the kidneys. No. The patient should not have been discharged home so early as she had a prolonged first stage of labour which places 3. Do you agree with the management her at a higher risk of infection. She should given to the patient? have been observed for at least 24 hours. No. A urinary tract infection that causes puerperal pyrexia is an indication for 4. How should you manage this admitting the patient to hospital. An patient further in the clinic? intravenous broad-spectrum antibiotic (ampicillin or cefuroxime) must be given as She must be made comfortable. Paracetamol this will lead to a rapid recovery and prevent (Panado) 1 g orally may be given for the serious complications. headache. If necessary she should be given a tepid sponging. An intravenous infusion should be started and she must then 4. Why is a puerperal patient at be referred to hospital. If at all possible risk of a urinary tract infection and the infant must accompany the patient how may this be prevented? to hospital. The need to start antibiotic Catheterisation is often required and this treatment, e.g. intravenous ampicillin and increases the risk of a urinary tract infection. oral metronidazole (Flagyl), before transfer Catheterisation must only be carried out when must be discussed with the doctor. necessary and must always be done as an aseptic procedure. CASE STUDY 3 CASE STUDY 4 A patient is seen at a clinic on day 5 days following a normal pregnancy, labour and A 36 year old woman that delivered her fourth delivery. She complains of rigors and lower child in a midwife obstetric unit the previous abdominal pain. She has a temperature of day is seen at a clinic for postnatal care. All 38.5 °C, tenderness over both kidneys (loins) her children are alive and well. She is a smoker and tenderness to percussion over both renal but is otherwise healthy. She has never used angles. A diagnosis of puerperal pyrexia is contraception.
- 18. THE PUERPERIUM AND FAMILY PLANNING 121 1. Should you counsel this patient CASE STUDY 5 about contraception? Yes. Every sexually active person needs A 15 year old primigravida is attending contraceptive counselling. This patient in the antenatal clinic. She has never used particular needs counselling as she is at an contraception. Her mother asks you for increased risk of maternal and perinatal contraceptive advice for her daughter after complications, should she fall pregnant again, delivery. The patient’s boyfriend has deserted because of her age and parity. her. 2. Which contraceptive methods would 1. Does this young teenager require be appropriate for this patient? contraceptive advice after delivery? Tubal ligation or vasectomy would be the Yes, she will certainly need contraceptive most appropriate method of contraception if counselling. She needs to learn sexual she does not want further children. Should responsibility and must be told to attend a she not want sterilisation, either an injectable family planning clinic. She also needs to know contraceptive or an intra-uterine contraceptive about postcoital contraception. device would be the next best choice. 2. Which contraceptive method would be 3. If the patient accepts tubal ligation, most the appropriate for this patient? when should this be done? An injectable contraceptive would probably be The most convenient time for the patient and the best method for her as she needs reliable her family is shortly after delivery (postpartum contraception for a long time. sterilisation). Every effort should be made to provide facilities for postpartum sterilisation 3. Why would she need a long- for all patients who request it. term contraceptive? Because she should only have her next child 4. If the couple decides not to have a when she is much older and has a stable tubal ligation or vasectomy, how will relationship. you determine whether an injectable or an intra-uterine contraceptive device would be the best choice? 4. If the patient prefers to use an oral contraceptive, would you regard Assessing the risk for pelvic inflammatory this as an appropriate method disease will determine which of the 2 methods of contraception for her? to use. If the patient has a stable relationship, an intra-uterine contraceptive device may be more No. A method which she is more likely to appropriate. However, if she or her husband use correctly and reliably would be more (or boyfriend) has other sexual partners, an appropriate. Oral contraceptives are only injectable contraceptive would be indicated. reliable if taken every day. 5. What other advice must be given 5. The patient and her mother are worried to a patient at risk of sexually that the long-term effect of injectable transmitted infections? contraception could be harmful to a girl of 15 years. What would be your advice? The patient must insist that her partner wears a condom during sexual intercourse. This will Injectable contraception is extremely safe and, reduce the risk of HIV infection. therefore, is an appropriate method for long-
- 19. 122 PRIMAR Y MATERNAL CARE term use. This method will not reduce her contraceptive pills may reduce milk production future fertility. while breastfeeding is being established. Progestogen-only pills have no effect on breastfeeding and must be used at least for the CASE STUDY 6 first 3 months following delivery of her baby. A healthy 32 year old woman visits a clinic for postnatal care. She had a normal delivery 3 days CASE STUDY 7 ago. In discussing contraception with her, she mentions that she is planning to fall pregnant A married primipara from a rural area has again within a year after she stops breastfeeding. just been delivered in hospital. She has a stable She is a school teacher and would like to relationship with her husband and they decide continue her career after having 2 children. to have their next infant in 5 years time. The patient would like to have an intra-uterine 1. The patient says that she has used contraceptive device inserted. an injectable contraceptive for 5 years before this pregnancy and would 1. Is this an appropriate like to continue with this method. method for this patient? What would your advice be? Yes, as the risk of developing pelvic Injectable contraception would not be inflammatory disease is low. appropriate as she plans her next pregnancy within a year, and there may be a delayed 2. When should the device be inserted? return to fertility. Six weeks or more after delivery as there is an increased risk of expulsion if the device is 2. If the patient insists on using an inserted earlier. injectable contraceptive, which drug would you advise her to use? 3. Could the patient, in the Any one of the injectables can be used (Depo meantime, rely on breastfeeding Provera, Petogen or Nur-Isterate) could be as a contraceptive method? used as there is no proven advantage of any one above the others. No. The risk of pregnancy is too high. She should use reliable contraception, such as injectable contraception or the progestogen- 3. Following further counselling, the only pill, until the device is inserted. patient decides on oral contraception and is given a combined pill. Do you agree with this management? No. As she plans to breastfeed, she should be given a progestogen-only pill. Combined oral
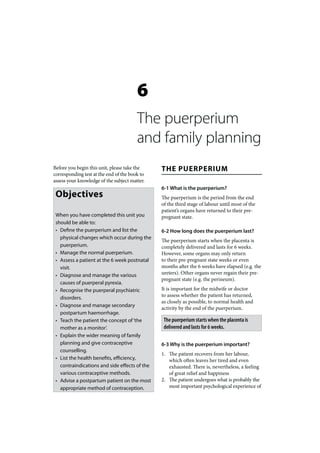
- 20. Patient details Examination within 1 Examination at 6 weeks Patient details Examination within 1 Examination at 6 weeks Discharge (Infant) week (Infant) (Infant) Discharge (Mother) week (Mother) (Mother) Date: Date: Date: Date: Date: Date: Exam by: Exam by: Exam by: Exam by: Exam by: Exam by: Delivered at: Clinic: Clinic: Delivered at: Clinic: Clinic: Infant’s name Infant’s name *Ask the following: Antenatal card no: Clinic no: Feeding EBF FF Mixed Mother’s name * Ask the mother the following: * Ask the mother the following: Feeding? EBF FF Other *Ask the following: Feeling unhappy? YES NO Able to resume YES NO Feeding EBF FF Mixed Problems? YES NO YES Hosp no Poor appetite? YES NO normal activities? Address Problems with YES NO Feeding well? YES NO YES Excessive sleeping/ YES NO Not alert? Problems with YES NO infant feeding? Examination at discharge Problems? Pale YES NO e *Examine the following: infant feeding? Cough/breathing YES NO Record weight and head Cough/breathing YES NO difficulties? circumference on Road to Health circu Tel/cellphone no difficulties? Problems with YES NO Birth weight Gestational Passed urine? Cyan YES NO nosis chart age Age Parity Gravidity Lochia foul YES NO C/S wound? Jaundice? YES NO smelling? Problems with YES NO Jaundice? Respiratory Pale? YES NO ANC complications Heavy vaginal YES NO episitomy? Passed stool? YES NO problems? bleeding? Vaginal YES NO YES NO YES NO Cyanosis? YES NO Urinary YES NO discahrge? incontinence? Fig 6-I: The essential postpartum care card CVS Abdomen Urinary YES NO *Examine the following: Responds to sound? YES NO problems? problems? Delivery route * Examine the following: incontinence? Birth weight Temp Pulse BP * Examine the following: YES NO YES NO Temperature (axillary) Eyes (white spot)? YES NO Date of delivery UMAC Temp Pulse BP Genitalia CNS problems? Pale? YES NO Thrush? YES NO Gestational age Pale? YES NO * problems? Complications in labour YES NO YES NO Fontanelle abnormal YES NO If breastfeeding, YES NO If breastfeeding, YES NO (anterior)? nipples cracked/ nipples cracked/ Umbilical Hip Jaundiced? YES NO Heart murmur? YES NO breast inflamed? breast inflamed? problems? dislocation? Uterus involuted YES NO * Test the following: YES NO YES NO Conjunctivitis? YES NO Abdominal mass? YES NO Postpartum course appropriately? Urine normal? YES NO Uterine YES NO Hb g/l (value) If ticks in shaded area Umbilical cord YES NO * If ticks in shaded areas comment tenderness? comment on back as to smelly? on back. Refer, if cannot treat If C/S, wound YES NO Hb< 10g/dl? YES NO problems and actions taken * If ticks in shaded area infected? * Vaccinate Rh RPR Hb Sutures removed? YES NO * If ticks in shaded areas comment NVP? YES NO N/A comment on back Refer, if PCR test? N/A YES NO on back Refer, if cannot treat AZT? YES NO N/A cannot treat Code Episiotomy YES NO CD4 YES NO N/A HAART? YES NO N/A infected? taken? AZT 7 days 28 days Vitamin A given? YES NO * Test the following: Type of contraception Permission for PCR? Consent given? YES NO N/A Iron/folate YES NO Urine normal? YES NO YES NO N/A given? Hb g/l (value) * If ticks in shaded area comment Mother’s name Bactrim YES NO N/A Type of contraception Hb<10g/dl? YES NO as to why on back prophylaxis? * If ticks in shaded area * If ticks in shaded areas comment as to why on back comment on back Refer, if Signature (mother) Vitamin A YES NO N/A supplementation? cannot treat Signature (witness) * If ticks in shaded area please explain why on back * UMAC = upper mid-arm circumferemce
